Search
- Page Path
- HOME > Search
Case Reports
- Hepatic basidiobolomycosis masquerading as cholangiocarcinoma: a case report and literature review
- Roopali Sehrawat, Nalini Bansal, Ajitabh Srivastava, Dharmender Malik, Vivek Vij
- J Liver Cancer. 2023;23(2):389-396. Published online August 17, 2023
- DOI: https://doi.org/10.17998/jlc.2023.06.07
- 1,248 Views
- 57 Downloads
-
 Abstract
Abstract
 PDF
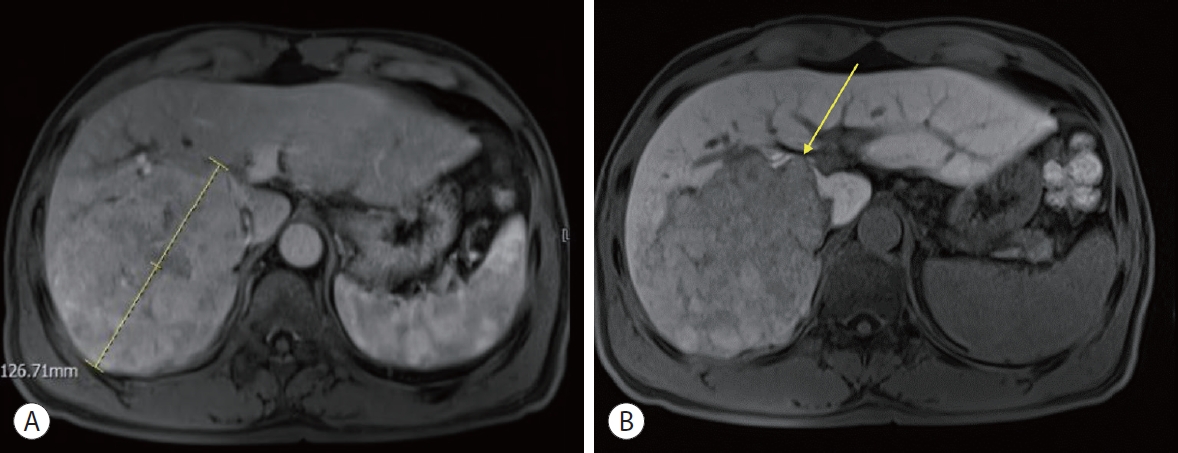
PDF - Basidiobolus ranarum is known to cause subcutaneous mycoses; however, rare cases of hepatic and gastrointestinal involvement by basidiobolomycosis have been reported. Hepatic basidiobolomycosis may be confused with a carcinoma on imaging, and histological examination and fungal culture can help distinguish between these two. We report a rare case of basidiobolomycosis in a 16-year-old male with liver and gastrointestinal involvement.

- Favorable response of hepatocellular carcinoma with portal vein tumor thrombosis after radiotherapy combined with atezolizumab plus bevacizumab
- Yong Tae Kim, Jina Kim, Jinsil Seong
- J Liver Cancer. 2023;23(1):225-229. Published online March 16, 2023
- DOI: https://doi.org/10.17998/jlc.2023.02.27

- 1,389 Views
- 74 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
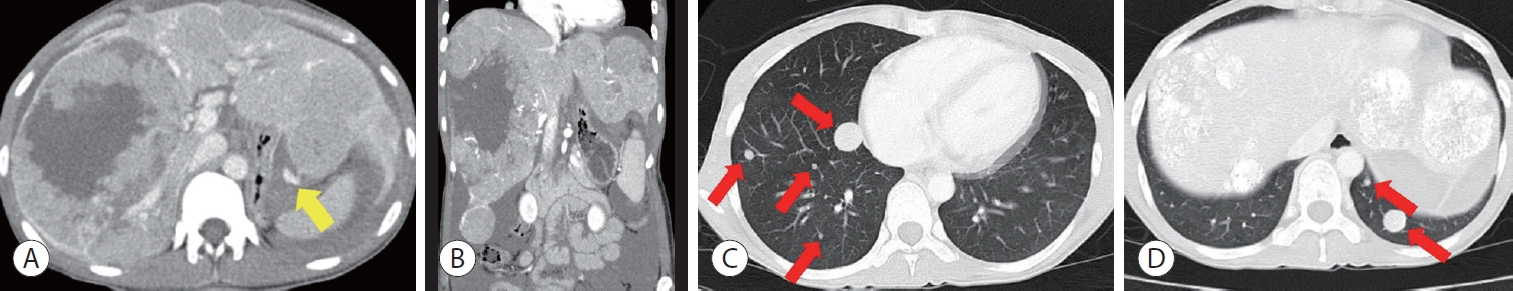
PDF - Recently, the superiority of atezolizumab plus bevacizumab (AteBeva) over sorafenib was proven in the IMbrave150 trial, and AteBeva became the first-line systemic treatment for untreated, unresectable hepatocellular carcinoma (HCC). While the results are encouraging, more than half of patients with advanced HCC are still being treated in a palliative setting. Radiotherapy (RT) is known to induce immunogenic effects that may enhance the therapeutic efficacy of immune checkpoint inhibitors. Herein, we report the case of a patient with advanced HCC with massive portal vein tumor thrombosis treated with a combination of RT and AteBeva, who showed near complete response in tumor thrombosis and favorable response to HCC. Although this is a rare case, it shows the importance of reducing the tumor burden via RT to combination immunotherapy in patients with advanced HCC.
-
Citations
Citations to this article as recorded by- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Carbon Ion Radiotherapy in the Treatment of Hepatocellular Carcinoma
Hwa Kyung Byun, Changhwan Kim, Jinsil Seong
Clinical and Molecular Hepatology.2023; 29(4): 945. CrossRef
- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab

- Multidisciplinary approach for hepatocellular carcinoma arising from cirrhotic liver with Budd-Chiari syndrome: a case report
- Sangmi Kim, Ji Hoon Kim, Ji Won Han, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon, Pil Soo Sung
- J Liver Cancer. 2022;22(2):202-206. Published online September 20, 2022
- DOI: https://doi.org/10.17998/jlc.2022.09.17
- 2,213 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
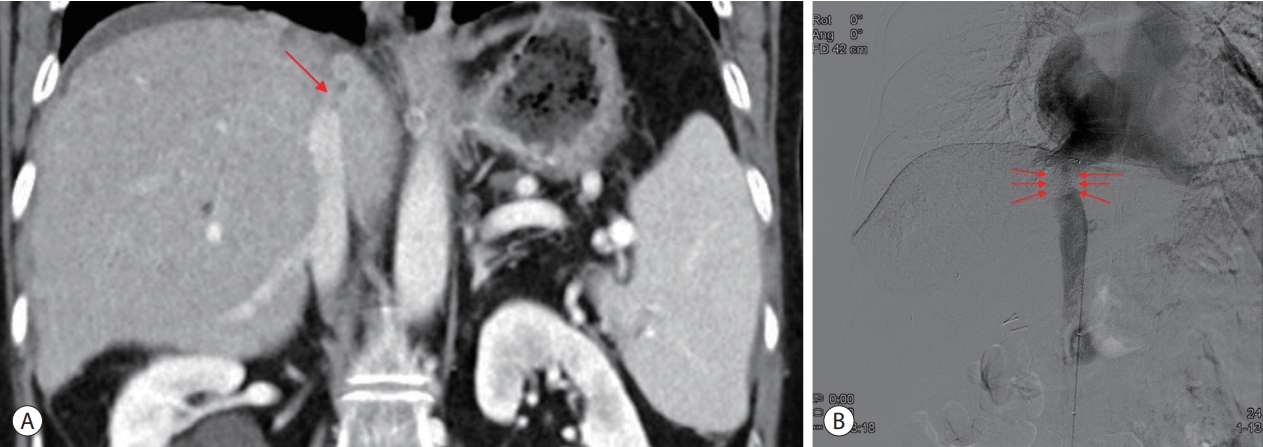
PDF - Budd-Chiari syndrome (BCS) is defined by the obstruction of the hepatic venous outflow between the small hepatic veins and the junction of the inferior vena cava (IVC) with the right atrium. BCS with IVC obstruction occasionally progresses to hepatocellular carcinoma (HCC). Here, we report the case of a patient with HCC arising from a cirrhotic liver with BCS, in whom the hepatic portion of the IVC was obstructed, and who had a favorable outcome with a multidisciplinary approach and IVC balloon angioplasty.

- Hepatocellular carcinoma with Budd-Chiari syndrome due to membranous obstruction of the inferior vena cava with long-term follow-up: a case report
- Choong Hee Kim, Gwang Hyeon Choi, Hee Young Na, Chang Jin Yoon, Jai Young Cho, Sangmi Jang, Ji Hye Kim, Eun Sun Jang, Jin-Wook Kim, Sook-Hyang Jeong
- J Liver Cancer. 2022;22(2):194-201. Published online September 15, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.24
- 2,784 Views
- 62 Downloads
-
 Abstract
Abstract
 PDF
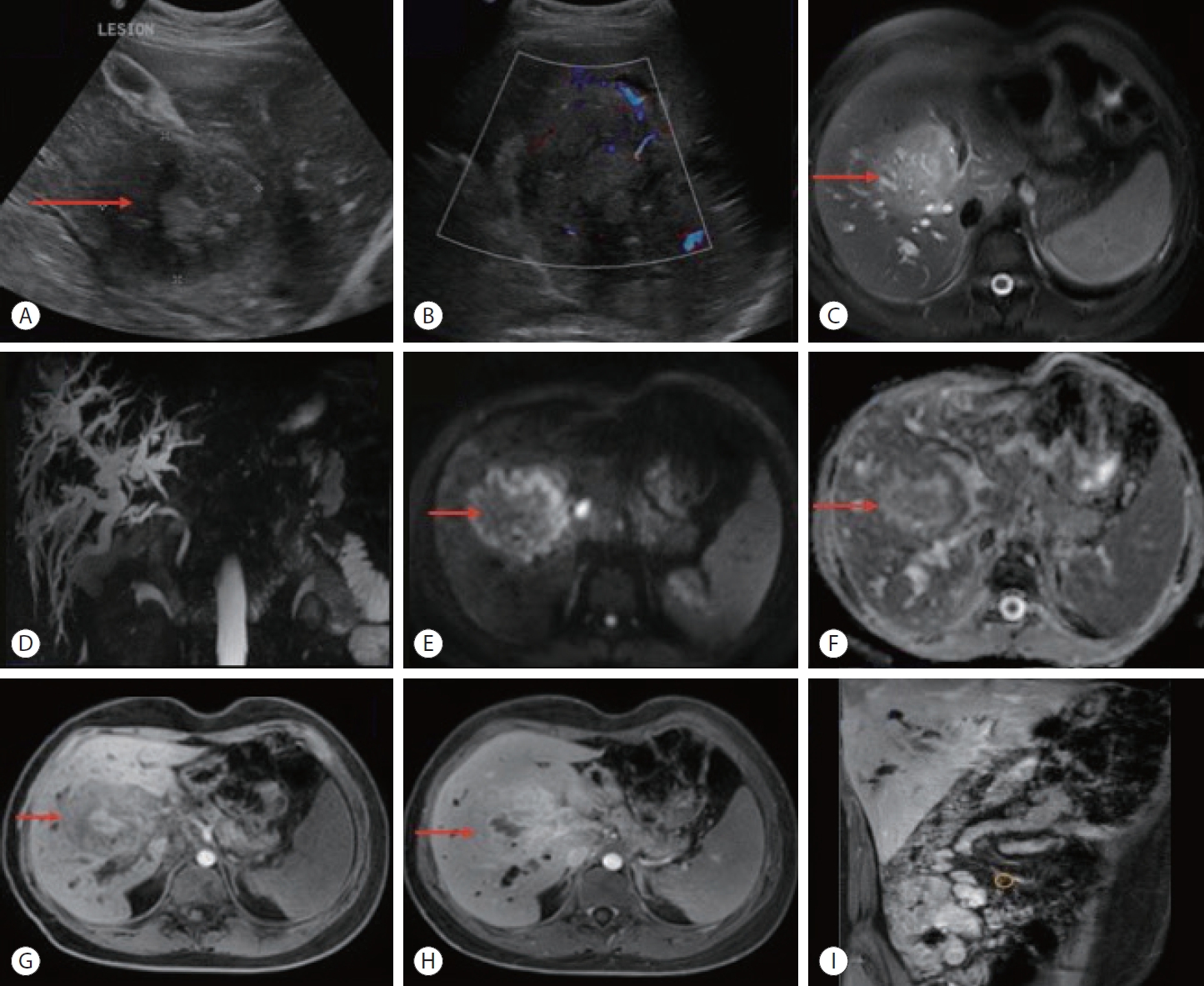
PDF - Membranous obstruction of the inferior vena cava (MOVC) is a rare subset of Budd-Chiari syndrome (BCS) with a subacute onset that is often complicated by cirrhosis and hepatocellular carcinoma (HCC). Here we report a case of recurrent HCC in a patient with cirrhosis and BCS that was treated with several episodes of transarterial chemoembolization followed by surgical tumorectomy, whereas the MOVC was successfully treated with balloon angioplasty followed by endovascular stenting. The patient was followed up for 9.9 years without anticoagulation and experienced no stent thrombosis. After the tumorectomy, the patient was HCC-free for 4.4 years of follow-up.

- Hepatocellular carcinoma diagnosed in a patient who had Fontan operation 30 years ago: a case report
- Moon Haeng Hur, Haeryoung Kim, Jeong-Hoon Lee
- J Liver Cancer. 2022;22(2):188-193. Published online August 31, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.17
- 2,611 Views
- 65 Downloads
-
 Abstract
Abstract
 PDF
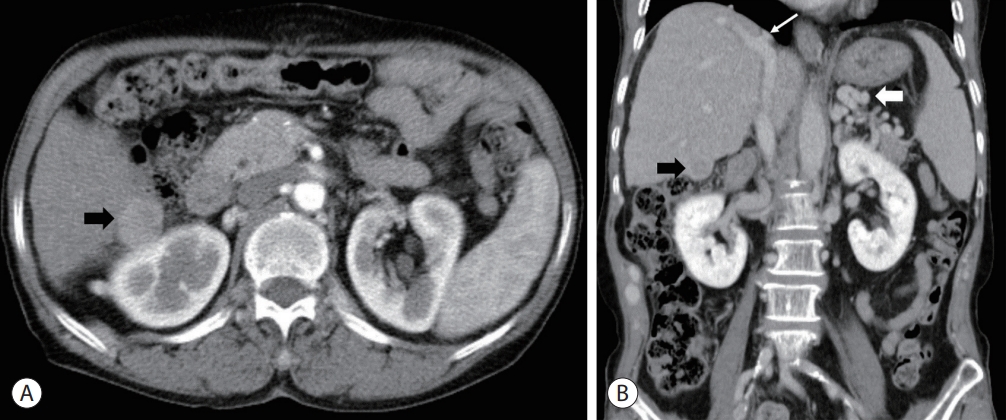
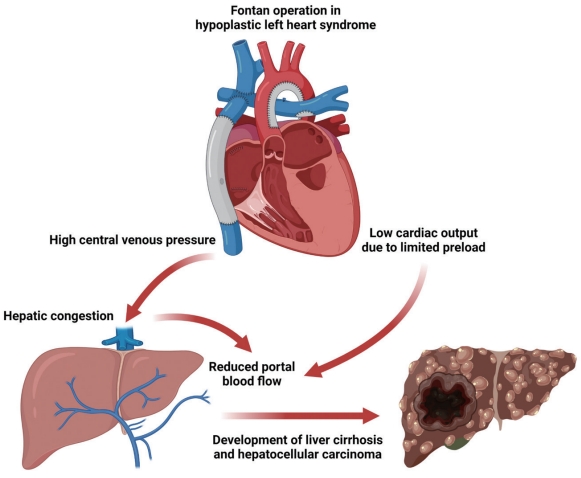
PDF - The Fontan operation is performed in patients with a single ventricle. As the systemic venous return is directly connected to the pulmonary circulation during this procedure, chronic hepatic congestion is induced, leading to Fontan-associated liver disease (FALD) including liver cirrhosis and hepatocellular carcinoma (HCC). In this report, we present a case of HCC diagnosed in a patient who underwent the Fontan operation 30 years ago. The patient underwent regular surveillance for FALD, which revealed a 4 cm-sized hepatic mass with elevated serum alpha-fetoprotein. After surgical treatment, there was no evidence of HCC recurrence during 3 years of follow-up. As the risk of HCC and Fontan-associated liver cirrhosis increases with the duration elapsed since the operation, regular surveillance should be emphasized. Serial follow-up of serum alpha-fetoprotein levels and abdominal imaging are necessary to achieve early and accurate diagnosis of HCC in post-Fontan patients.

- Novel management of expected post-radiotherapy complications in hepatocellular carcinoma patients: a case report
- Sung Hoon Chang, Tae Suk Kim, Yong Hwan Jeon, Nuri Hyun Jung, Dae Hee Choi
- J Liver Cancer. 2022;22(2):183-187. Published online August 24, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.03
- 2,027 Views
- 55 Downloads
-
 Abstract
Abstract
 PDF
PDF - In recent years, radiotherapy (RT) has been used to treat hepatocellular carcinoma (HCC) at each stage. This clinical trend has developed with the increasing improvement of RT techniques, which show clinical results comparable to those of other treatment modalities. Intensity-modulated radiotherapy uses a high radiation dose to improve treatment effectiveness. However, the associated radiation toxicity can damage adjacent organs. Radiation-induced gastric damage with gastric ulcers is a complication of RT. This report presents a novel management strategy for preventing post-RT gastric ulcers. We present the case of a 53-year-old male patient diagnosed with HCC, who experienced gastric ulcer after RT. Before the second round of RT, the patient was administered a gas-foaming agent, which was effective in preventing RT complications.

- Fibrolamellar hepatocellular carcinoma that was successfully treated with surgical resection: a case report
- Seong Kyun Na
- J Liver Cancer. 2022;22(2):178-182. Published online June 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.06.10

- 2,575 Views
- 72 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Fibrolamellar hepatocellular carcinoma (FLHCC) is a rare malignant hepatic cancer with characteristics that differ from those of typical hepatocellular carcinoma (HCC). Unlike conventional HCC, FLHCC is common in young patients without any underlying liver disease and is known to be associated with a unique gene mutation. This cancer type is rare in Asia, with only a few cases being reported in Korea. We report a case of FLHCC in a young woman that successfully underwent surgical resection. The efficacy of alternative treatments, such as transarterial chemoembolization or systemic chemotherapies, has not yet been established. To conclude, early diagnosis and appropriate surgical resection are important for the treatment of FLHCC.
-
Citations
Citations to this article as recorded by- Fibrolamellar Hepatocellular Carcinoma (FLHCC) in a Young Patient Presenting With Nausea and Vomiting After a Greasy Meal
Mohamed Ismail , Sahiba Singh, Menna-Allah Elaskandrany , David s Kim, Yazan Abboud, Michael Bebawy, Abena Oduro, Ritik mahaveer Goyal, Omar Mohamed , Weizheng Wang
Cureus.2024;[Epub] CrossRef
- Fibrolamellar Hepatocellular Carcinoma (FLHCC) in a Young Patient Presenting With Nausea and Vomiting After a Greasy Meal

- Long-term survival after CCRT and HAIC followed by ALPPS for hepatocellular carcinoma with portal vein invasion: a case report
- In-Jung Kim, Sung Hwan Yoo, Jung Il Lee, Kwan Sik Lee, Hyun Woong Lee, Jin Hong Lim
- J Liver Cancer. 2022;22(1):84-90. Published online March 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.07
- 3,251 Views
- 74 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
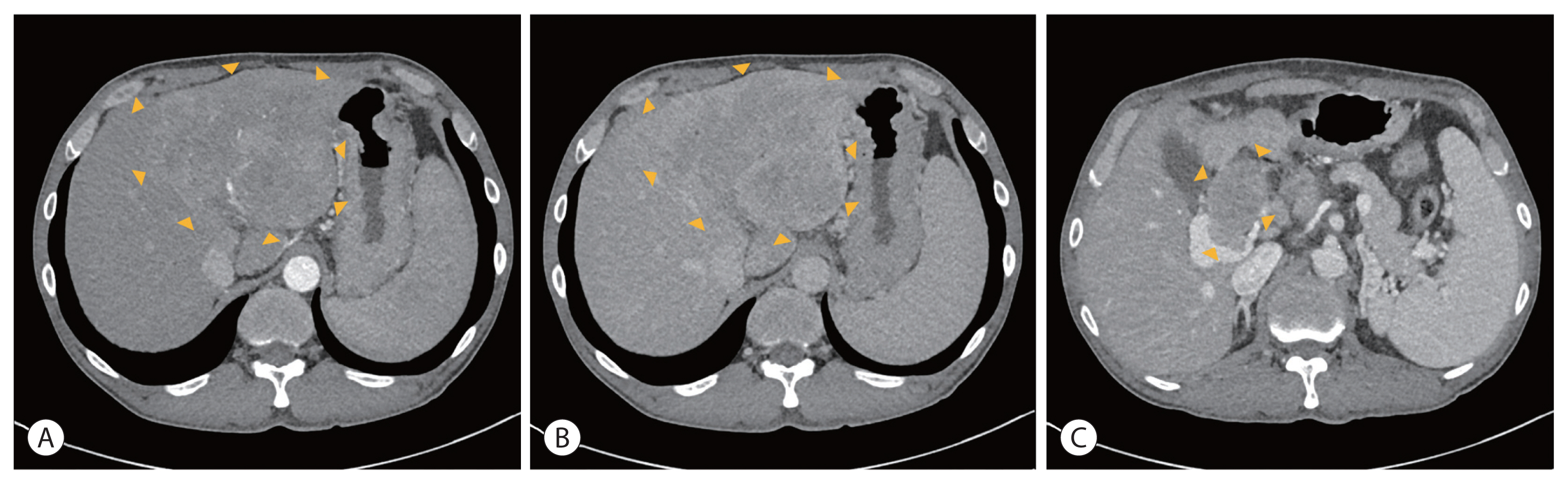
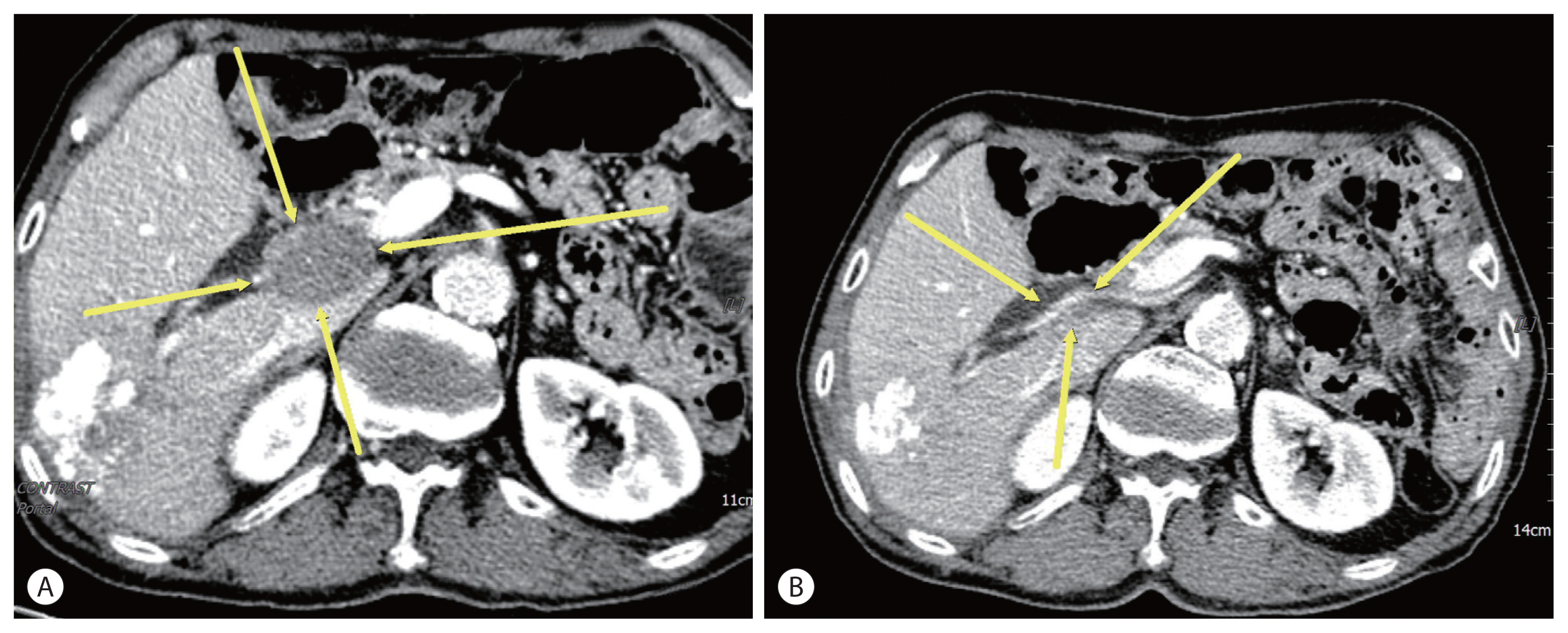
PDF - There are various methods for treating advanced hepatocellular carcinoma with portal vein invasion, such as systemic chemotherapy, transarterial chemoembolization, transarterial radioembolization, and concurrent chemoradiotherapy. These methods have similar clinical efficacy but are designed with a palliative aim. Herein, we report a case that experienced complete remission through “associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)” after concurrent chemoradiotherapy and hepatic artery infusion chemotherapy. In this patient, concurrent chemoradiotherapy and hepatic artery infusion chemotherapy induced substantial tumor shrinkage, and hypertrophy of the nontumor liver was sufficiently induced by portal vein ligation (stage 1 surgery) followed by curative resection (stage 2 surgery). Using this approach, long-term survival with no evidence of recurrence was achieved at 16 months. Therefore, the optimal use of ALPPS requires sufficient consideration in cases of significant hepatocellular carcinoma shrinkage for curative purposes.
-
Citations
Citations to this article as recorded by- Higher objective responses by hepatic arterial infusion chemotherapy following atezolizumab and bevacizumab failure than when used as initial therapy in hepatocellular carcinoma: a retrospective study
Jae-Sung Yoo, Ji Hoon Kim, Hee Sun Cho, Ji Won Han, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon, Suho Kim, Jung Suk Oh, Ho Jong Chun, Pil Soo Sung
Abdominal Radiology.2024;[Epub] CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Higher objective responses by hepatic arterial infusion chemotherapy following atezolizumab and bevacizumab failure than when used as initial therapy in hepatocellular carcinoma: a retrospective study

- Concurrent transarterial radioembolization and combination atezolizumab/ bevacizumab treatment of infiltrative hepatocellular carcinoma with portal vein tumor thrombosis: a case report
- Min Kyung Park, Su Jong Yu
- J Liver Cancer. 2022;22(1):69-74. Published online March 21, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.09
- 3,745 Views
- 112 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
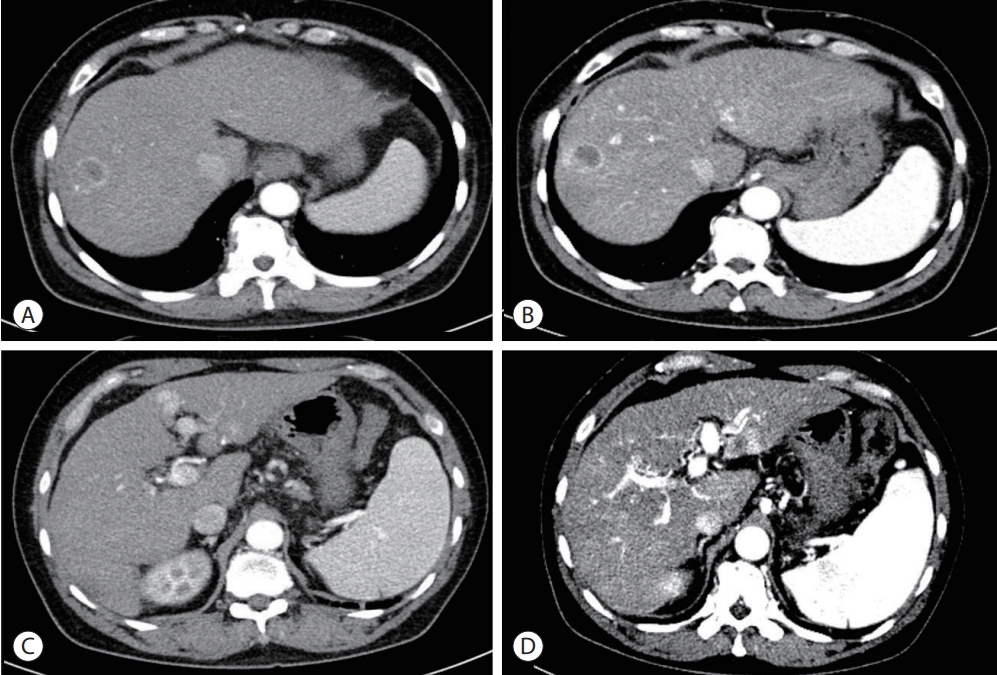
PDF - Treatment options for advanced hepatocellular carcinoma (HCC) have been rapidly evolving. Herein, we describe a patient with advanced HCC and portal vein tumor thrombosis (PVTT) who responded decisively to a multidisciplinary approach. The patient had an ill-defined infiltrative HCC (diffuse subtype), with several intrahepatic metastasis and tumor invasion of left portal vein. Concurrent use of transarterial radioembolization (TARE) and systemic therapeutics (atezolizumab + bevacizumab) ultimately proved successful. There was marked reduction in tumor volume after TARE and an additional three cycles of atezolizumab plus bevacizumab. This concurrent treatment was well tolerated, without adverse events during immunotherapy. The impressive results achieved suggest that concurrent TARE and combination atezolizumab/bevacizumab is a promising treatment approach for advanced HCC with PVTT.
-
Citations
Citations to this article as recorded by- Biologics, Immunotherapies, and Cytotoxic Chemotherapy for Hepatocellular Carcinoma following Current Recommendations by the BCLC: A Review of Agents
Rajangad S. Gurtatta, Sydney E. Whalen, Charles E. Ray
Seminars in Interventional Radiology.2024; 41(01): 084. CrossRef - Combining immunotherapy with transarterial radioembolization
ZeynepCeren Balaban Genc, Efe Soydemır, SevalAy Ersoy, Tunc Ones
Indian Journal of Nuclear Medicine.2023; 38(2): 145. CrossRef - The New Era of Systemic Treatment for Hepatocellular Carcinoma: From the First Line to the Optimal Sequence
Maria Cerreto, Ferdinando Cardone, Lucia Cerrito, Leonardo Stella, Francesco Santopaolo, Maria Pallozzi, Antonio Gasbarrini, Francesca Romana Ponziani
Current Oncology.2023; 30(10): 8774. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Biologics, Immunotherapies, and Cytotoxic Chemotherapy for Hepatocellular Carcinoma following Current Recommendations by the BCLC: A Review of Agents

- Multidisciplinary treatment with immune checkpoint inhibitors for advanced stage hepatocellular carcinoma
- Ahlim Lee, Jaejun Lee, Hyun Yang, Soo-Yoon Sung, Chang Ho Jeon, Su Ho Kim, Moon Hyung Choi, Young Joon Lee, Ho Jong Chun, Si Hyun Bae
- J Liver Cancer. 2022;22(1):75-83. Published online March 18, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.04
- 4,464 Views
- 98 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
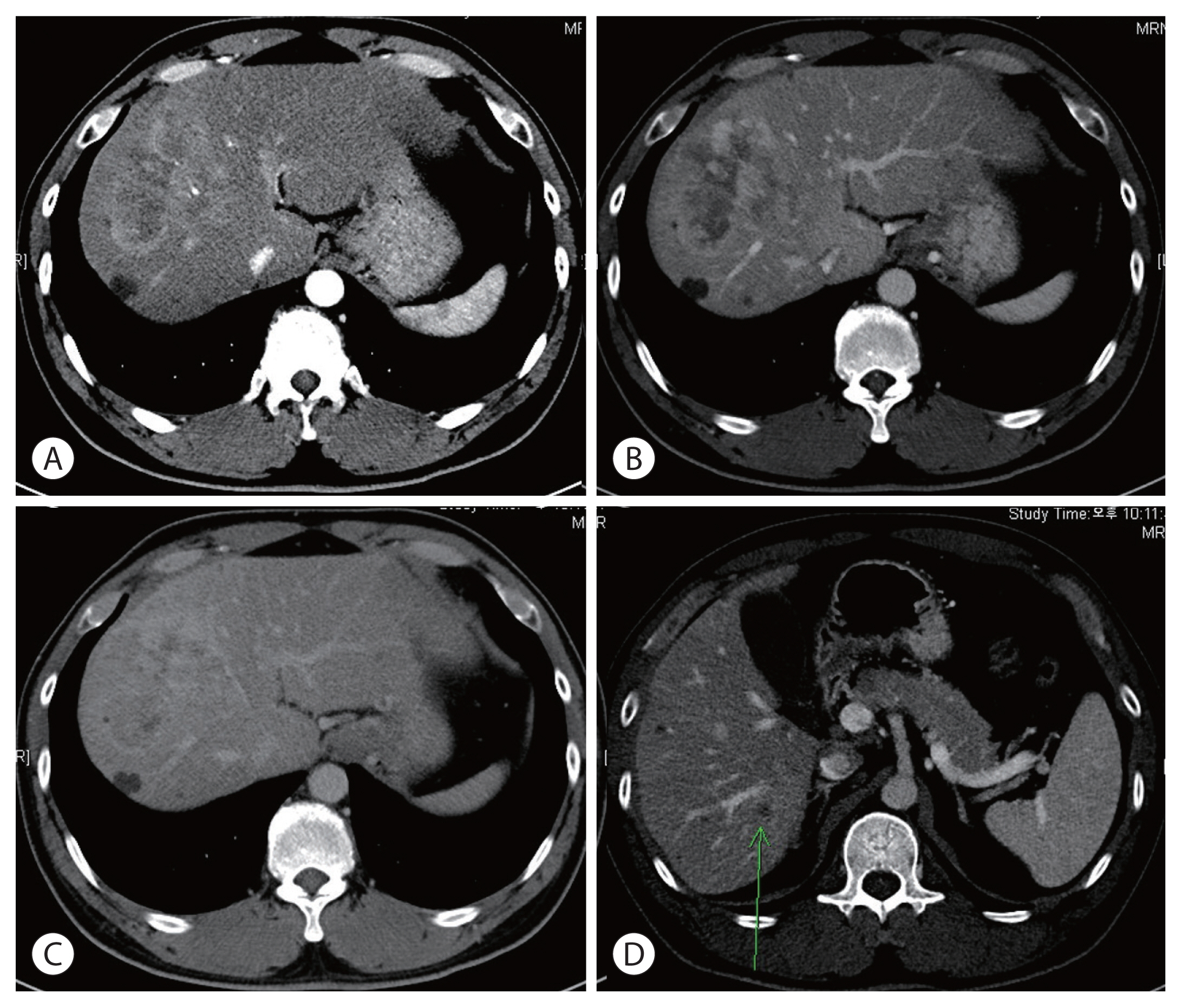
PDF - Hepatocellular carcinoma (HCC) is a cytotoxic chemotherapy-resistant tumor and most HCCs arise in a background of liver cirrhosis of various causes. Although the IMBrave150 trial showed remarkable advancements in the treatment of unresectable HCC with atezolizumab plus bevacizumab (AteBeva), therapeutic outcomes were unsatisfactory in more than half of the patients. Accordingly, many ongoing trials combine conventional modalities with new drugs such as immune checkpoint inhibitors for better treatment outcomes, and they are expected to benefit patients with limited responses to conventional treatment. Here, two patients with advanced stage HCC with preserved liver function and good performance status showed partial response after treatment with combination or sequential therapy of AteBeva, hepatic arterial infusion chemotherapy, radiation therapy, and transarterial chemoembolization. These findings indicate the efficacy of multidisciplinary treatment against advanced HCC. Additional studies are required to establish optimal treatment strategies.
-
Citations
Citations to this article as recorded by- Complications of immunotherapy in advanced hepatocellular carcinoma
Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Journal of Liver Cancer.2024; 24(1): 9. CrossRef - Higher objective responses by hepatic arterial infusion chemotherapy following atezolizumab and bevacizumab failure than when used as initial therapy in hepatocellular carcinoma: a retrospective study
Jae-Sung Yoo, Ji Hoon Kim, Hee Sun Cho, Ji Won Han, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon, Suho Kim, Jung Suk Oh, Ho Jong Chun, Pil Soo Sung
Abdominal Radiology.2024;[Epub] CrossRef - Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Complications of immunotherapy in advanced hepatocellular carcinoma

- Sorafenib combined with radiation therapy for advanced hepatocellular carcinoma with portal and hepatic vein invasion extending to the inferior vena cava: a complete response case according to modified RECIST criteria
- Yuri Cho, Bo Hyun Kim, Tae Hyun Kim, Young Hwan Koh, Joong-Won Park
- J Liver Cancer. 2022;22(1):63-68. Published online February 14, 2022
- DOI: https://doi.org/10.17998/jlc.2022.01.18

- 3,030 Views
- 93 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
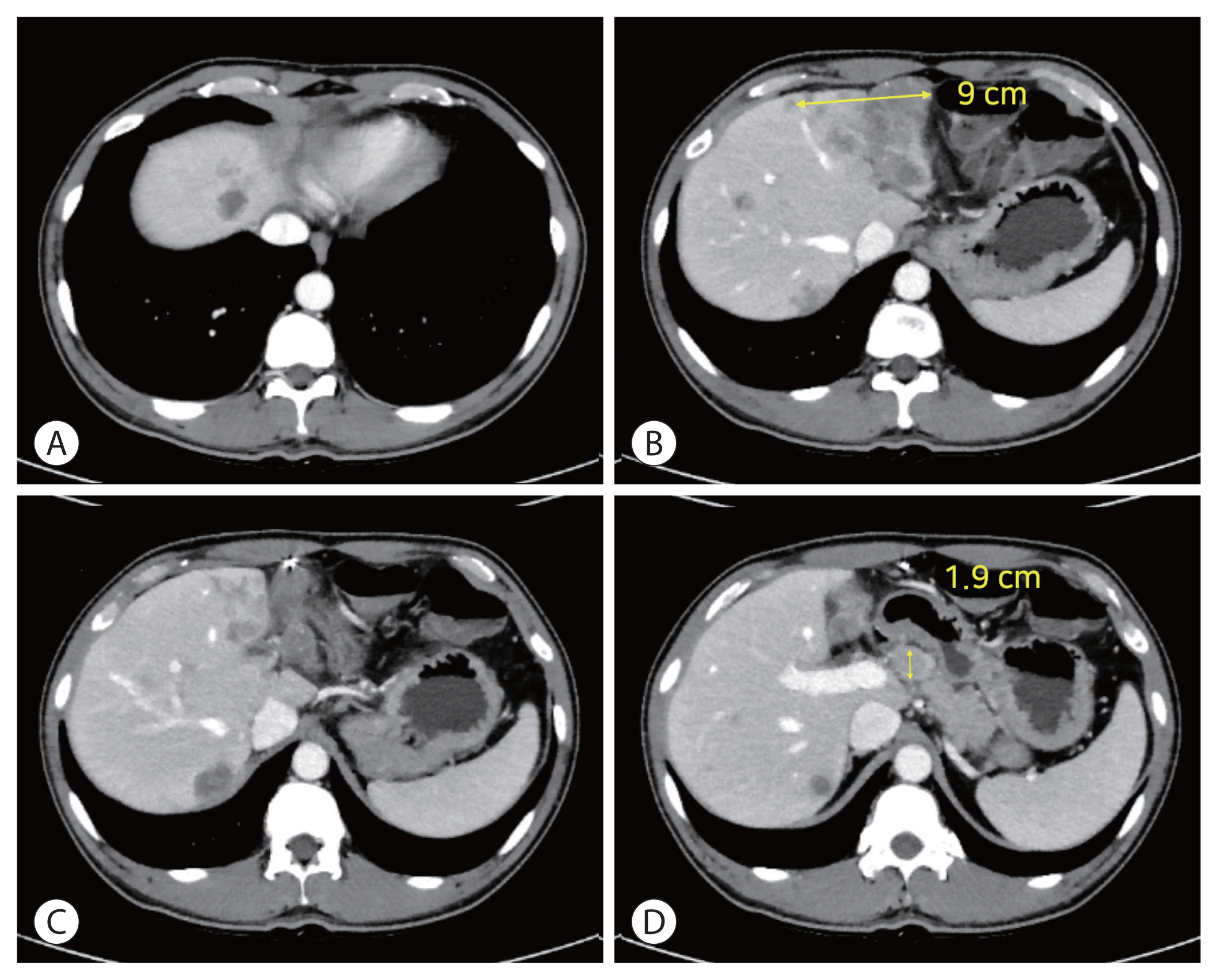
PDF - The prognosis of patients with advanced hepatocellular carcinoma (HCC) with tumor thrombus extending to the inferior vena cava (IVC) is extremely poor. Herein, we present a rare case of advanced HCC that was treated with sorafenib and radiotherapy, leading to complete remission. This patient had a 9 cm infiltrative HCC occupying almost the entire left lobe with a tumor thrombus extending through the hepatic vein, IVC, and left portal vein. The patient received 400 mg sorafenib twice daily. One year after the start of sorafenib, intensity-modulated radiation therapy for viable HCC and tumor thrombus was performed with a dose of 5,500 cGy. Twenty-seven months after the starting date of sorafenib, there was no intratumoral arterial enhancement, which suggested a complete response according to the modified RECIST criteria. This case suggests that the combination of sorafenib and radiotherapy might provide clinical benefits in patients with advanced HCC with IVC tumor thrombus.
-
Citations
Citations to this article as recorded by- The Treatment of Hepatocellular Carcinoma with Major Vascular Invasion
Tomoko Tadokoro, Joji Tani, Asahiro Morishita, Koji Fujita, Tsutomu Masaki, Hideki Kobara
Cancers.2024; 16(14): 2534. CrossRef - Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- The Treatment of Hepatocellular Carcinoma with Major Vascular Invasion

- Complete response to local therapy for advanced hepatocellular carcinoma with lung metastasis: a case report
- Daeun Kim, Seiyeon Park, Won Sohn, Hyun Pyo Hong, Byung Ik Kim
- J Liver Cancer. 2022;22(1):51-56. Published online January 27, 2022
- DOI: https://doi.org/10.17998/jlc.2021.12.28
- 3,491 Views
- 104 Downloads
-
 Abstract
Abstract
 PDF
PDF - The concept of oligometastasis is widely accepted for various types of solid tumors; accordingly, better outcomes can be anticipated with aggressive local interventions. The treatment of advanced hepatocellular carcinoma (HCC) with extrahepatic metastasis is systemic therapy. However, treatment responses to systemic therapy are poor. Recently, a small number of metastatic cancers (oligometastasis) have been controlled by local therapy rather than systemic therapy. Our study reports a case of a 66-year-old male patient with advanced HCC with lung metastasis, which was treated with local therapy. There were less than four metastases in the lungs, which were treated with wedge resection, radiofrequency, and radiation therapy. He repeatedly underwent local therapy for lung oligometastasis and locoregional therapy for intrahepatic HCC rather than systemic therapy; control by local therapy was possible as his liver function was preserved with Child-Turcotte-Pugh class A.

- A case report of advanced hepatocellular carcinoma treated with hepatic arterial infusion chemotherapy and sorafenib combination therapy followed by metastasectomy of lung and muscle metastases
- Sang Yi Moon, Sang Young Han, Yang-Hyun Baek
- J Liver Cancer. 2022;22(1):57-62. Published online January 6, 2022
- DOI: https://doi.org/10.17998/jlc.2021.12.20
- 3,816 Views
- 92 Downloads
-
 Abstract
Abstract
 PDF
PDF - Currently, various tyrosine kinase inhibitors and immune checkpoint inhibitors have been suggested in the treatment guidelines for advanced hepatocellular carcinoma (HCC). However, sorafenib was the only systemic drug approved 10 years ago. In 2010, a woman diagnosed with HCC rupture and multiple lung metastases visited our hospital. At the time of visiting our hospital, she had undergone transarterial chemoembolization at another hospital to control bleeding due to HCC rupture. We treated her with hepatic arterial infusion chemotherapy and sorafenib combination therapy to increase the control of intrahepatic tumors in consideration of the modest efficacy of sorafenib. The intrahepatic tumor was almost controlled. Metastasectomy was performed to control lung oligometastasis. Subsequently, additional muscle metastasis was confirmed, and metastasectomy was performed. Although this is a very rare case, it shows that a multidisciplinary approach can improve the prognosis of patients with HCC.

- Primary multifocal cystic signet ring neuroendocrine tumor of liver: a case report
- Nalini Bansal, Brahmananda Satapathy
- J Liver Cancer. 2021;21(2):187-193. Published online September 30, 2021
- DOI: https://doi.org/10.17998/jlc.2021.09.17

- 3,455 Views
- 78 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Primary signet ring neuroendocrine tumors of the liver are extremely rare tumors. Morphologically, they mimic signet ring cell adenocarcinomas; however, the absence of mucin by special stains and the expression of neuroendocrine markers help to diagnose these tumors. We herein report a case of a 47-year-old female who presented with multiple solid and cystic lesions in both liver lobes, which were initially suggested to be biliary cystadenocarcinoma on imaging. Liver biopsy of the lesion revealed the presence of a signet ring neoplasm with diffuse expression of synaptophysin and pan-cytokeratin. The case was subsequently diagnosed as a primary hepatic signet ring neuroendocrine tumor. The patient was offered 3 cycles of chemotherapy and is well preserved after 14 months of diagnosis. Although this is an extremely rare entity, its possibility should be considered in the differential diagnosis of neoplasms characterized by signet ring cell morphology.
-
Citations
Citations to this article as recorded by- Gastric Neuroendocrine Tumor With Cystic Hepatic Metastases Mimicking Hepatic Echinococcosis: A Case Report
Rahul Gupta, Deepak Gusain, Nalini Bansal, Rahul Varshney, Arvind Singh
Cureus.2024;[Epub] CrossRef - HER-2-positive primary neuroendocrine neoplasms of the breast with signet ring feature: A case report and review of literature
Yunjin Li, Yi Cao, Xiaoying Wu, Ruijie Liu, Kuansong Wang
Frontiers in Oncology.2022;[Epub] CrossRef
- Gastric Neuroendocrine Tumor With Cystic Hepatic Metastases Mimicking Hepatic Echinococcosis: A Case Report

- Complete response in hepatocellular carcinoma with lymph node metastasis by combination therapy of atezolizumab and bevacizumab: a case report
- Sang Youn Hwang, Sun Mi Lee, Jeong Woo Lim, Gi Jung Jeon, Hye Won Lee
- J Liver Cancer. 2021;21(2):177-180. Published online September 30, 2021
- DOI: https://doi.org/10.17998/jlc.2021.09.10
- 3,392 Views
- 85 Downloads
-
 Abstract
Abstract
 PDF
PDF - Sorafenib is the oldest first line systemic treatment in patients with advanced hepatocellular carcinoma (HCC) and has been used exclusively for nearly 10 years. The superiority of administering a combination of atezolizumab plus bevacizumab (AteBeva) compared to sorafenib as first line systemic treatment for unresectable HCC was recently proven during the IMbrave150 Phase III randomized trial. While clinicians can expect improved responses and treatment outcomes due to the good results of the IMbrave 150 trial, they must also consider that atezolizumab can cause various immune-related adverse events (IrAEs). Based on the above suggestions, we herein present a case of HCC with lymph node metastasis who achieved complete remission following treatment with AteBeva and developed an IrAE (adrenal insufficiency). Further study of real-life data regarding combination therapy with AteBeva is needed to manage patients with advanced HCC.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter