Article category
- Page Path
- HOME > Article category > Article category
Original Article
- Effect of direct-acting antivirals for hepatitis C virus-related hepatocellular carcinoma recurrence and death after curative treatment
- Young-Hwan Ahn, Heirim Lee, Ji Eun Han, Hyo Jung Cho, Jae Youn Cheong, Bumhee Park, Soon Sun Kim
- J Liver Cancer. 2022;22(2):125-135. Published online June 28, 2022
- DOI: https://doi.org/10.17998/jlc.2022.05.24
- 3,019 Views
- 80 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
There has been a long-standing debate about the association of directacting antiviral (DAA) therapy and hepatocellular carcinoma (HCC) recurrence. This study aimed to investigate the association between DAA therapy and HCC recurrence after curative therapy.
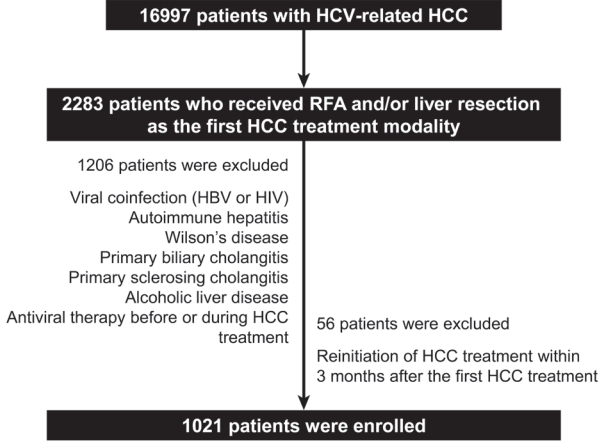
Methods
We retrospectively enrolled 1,021 patients with HCV-related (hepatitis C virus) HCC who underwent radiofrequency ablation (RFA), liver resection, or both as the first treatment modality from January 2007 to December 2016 and without a history of HCV therapy before HCC treatment from a nationwide database. The effect of HCV treatment on HCC recurrence and all-cause mortality was also investigated.
Results
Among the 1,021 patients, 77 (7.5%) were treated with DAA, 14 (1.4%) were treated with interferon-based therapy, and 930 (91.1%) did not receive HCV therapy. DAA therapy was an independent prognostic factor for lower HCC recurrence rate (hazard ratio [HR], 0.04; 95% confidence interval [CI], 0.006-0.289; P=0.001 for landmarks at 6 months after HCC treatment and HR, 0.05; 95% CI, 0.007-0.354; P=0.003 for landmarks at 1 year). Furthermore, DAA therapy was associated with lower all-cause mortality (HR, 0.049; 95% CI, 0.007-0.349; P=0.003 for landmarks at 6 months and HR, 0.063; 95% CI, 0.009-0.451; P=0.006 for landmarks at 1 year).
Conclusions
DAA therapy after curative HCC treatment can decrease HCC recurrence and all-cause mortality compared to interferon-based therapy or no antiviral therapy. Therefore, clinicians should consider administering DAA therapy after curative HCC treatment in patients with HCV-related HCC. -
Citations
Citations to this article as recorded by- Comparison of Surgical Resection and Radiofrequency Ablation in Elderly Patients with Hepatocellular Carcinoma
Jun Il Kim, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park, Jeong-Ju Yoo
Digestive Diseases and Sciences.2024; 69(3): 1055. CrossRef - Analyzing risk factors and developing a stratification system for hepatocellular carcinoma recurrence after interferon-free direct-acting antiviral therapy in chronic hepatitis C patients
Chih-Hsuan Luan, Pin-Shuo Su, Chi-Jen Chu, Chung-Chi Lin, Chien-Wei Su, Jiing-Chyuan Luo, I-Cheng Lee, Chen-Ta Chi, Shou-Dong Lee, Yuan-Jen Wang, Fa-Yauh Lee, Yi-Hsiang Huang, Ming-Chih Hou
Journal of the Chinese Medical Association.2024; 87(4): 357. CrossRef - Addition of Kidney Dysfunction Type to MELD-Na for the Prediction of Survival in Cirrhotic Patients Awaiting Liver Transplantation in Comparison with MELD 3.0 with Albumin
Kyeong-Min Yeom, Jong-In Chang, Jeong-Ju Yoo, Ji Eun Moon, Dong Hyun Sinn, Young Seok Kim, Sang Gyune Kim
Diagnostics.2023; 14(1): 39. CrossRef - Is direct-acting antiviral treatment beneficial or harmful for patients with hepatitis C virus-related hepatocellular carcinoma?
Hye Won Lee
Journal of Liver Cancer.2022; 22(2): 91. CrossRef
- Comparison of Surgical Resection and Radiofrequency Ablation in Elderly Patients with Hepatocellular Carcinoma

Case Report
- Fibrolamellar hepatocellular carcinoma that was successfully treated with surgical resection: a case report
- Seong Kyun Na
- J Liver Cancer. 2022;22(2):178-182. Published online June 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.06.10

- 2,094 Views
- 65 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
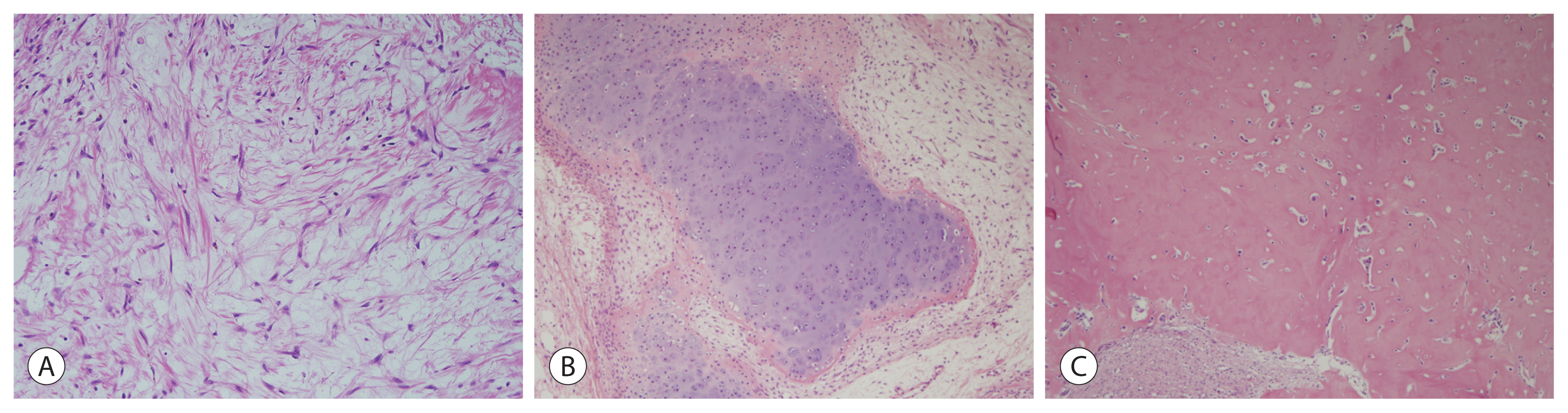
PDF - Fibrolamellar hepatocellular carcinoma (FLHCC) is a rare malignant hepatic cancer with characteristics that differ from those of typical hepatocellular carcinoma (HCC). Unlike conventional HCC, FLHCC is common in young patients without any underlying liver disease and is known to be associated with a unique gene mutation. This cancer type is rare in Asia, with only a few cases being reported in Korea. We report a case of FLHCC in a young woman that successfully underwent surgical resection. The efficacy of alternative treatments, such as transarterial chemoembolization or systemic chemotherapies, has not yet been established. To conclude, early diagnosis and appropriate surgical resection are important for the treatment of FLHCC.
-
Citations
Citations to this article as recorded by- Fibrolamellar Hepatocellular Carcinoma (FLHCC) in a Young Patient Presenting With Nausea and Vomiting After a Greasy Meal
Mohamed Ismail , Sahiba Singh, Menna-Allah Elaskandrany , David s Kim, Yazan Abboud, Michael Bebawy, Abena Oduro, Ritik mahaveer Goyal, Omar Mohamed , Weizheng Wang
Cureus.2024;[Epub] CrossRef
- Fibrolamellar Hepatocellular Carcinoma (FLHCC) in a Young Patient Presenting With Nausea and Vomiting After a Greasy Meal

Notice of Retraction and Replacement
- Yoon et al. Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
- Jeong-Hoon Lee
- J Liver Cancer. 2022;22(2):207-207. Published online June 8, 2022
- DOI: https://doi.org/10.17998/jlc.21.1.58.e1
- Retracts: J Liver Cancer 2021;21(1):58
- 3,103 Views
- 66 Downloads
- 1 Citation

Original Article
- The dual role of transforming growth factor-beta signatures in human B viral multistep hepatocarcinogenesis: early and late responsive genes
- Jeong Eun Yoo, Ji Hae Nahm, Young-Joo Kim, Youngsic Jeon, Young Nyun Park
- J Liver Cancer. 2022;22(2):115-124. Published online May 20, 2022
- DOI: https://doi.org/10.17998/jlc.2022.04.20
- 2,474 Views
- 100 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Transforming growth factor-beta (TGF-β) has a dichotomous role, functioning as a tumor suppressor and tumor promoter. TGF-β signatures, explored in mouse hepatocytes, have been reported to predict the clinical outcomes of hepatocellular carcinoma (HCC) patients; HCCs exhibiting early TGF-β signatures showed a better prognosis than those with late TGF-β signatures. The expression status of early and late TGF-β signatures remains unclear in defined lesions of human B-viral multistep hepatocarcinogenesis.
Methods
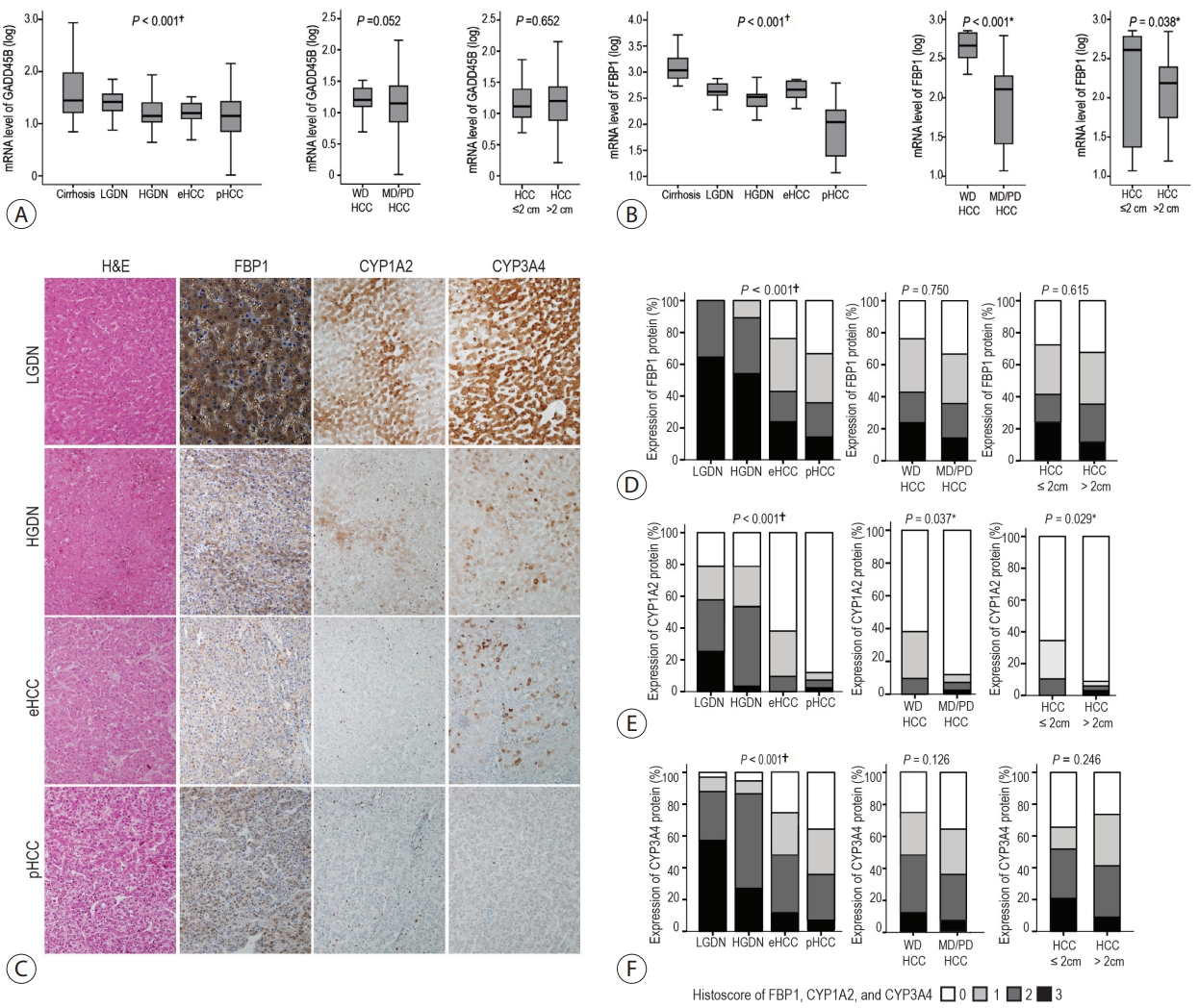
The expression of TGF-β signatures, early and late responsive signatures of TGF-β were investigated and analyzed for their correlation in cirrhosis, low-grade dysplastic nodules (DNs), high-grade DNs, early HCCs and progressed HCCs (pHCCs) by real-time PCR and immunohistochemistry.
Results
The expression levels of TGF-β signaling genes (TGFB1, TGFBR1, TGFBR2 and SMAD4) gradually increased with the progression of hepatocarcinogenesis, peaking in pHCCs. The expression of early responsive genes of TGF-β (GADD45B, FBP1, CYP1A2 and CYP3A4) gradually decreased, and that of the late TGF-β signatures (TWIST and SNAI1) significantly increased according to the progression of multistep hepatocarcinogenesis. Furthermore, mRNA levels of TWIST and SNAI1 were well correlated with those of stemness markers, with upregulation of TGF-β signaling, whereas FBP1 expression was inversely correlated with that of stemness markers.
Conclusions
The enrichment of the late responsive signatures of TGF-β with induction of stemness is considered to be involved in the progression of the late stage of multistep hepatocarcinogenesis, whereas the early responsive signatures of TGF-β are suggested to have tumor-suppressive roles in precancerous lesions of the early stage of multistep hepatocarcinogenesis.

Review Articles
- Combination of interventional oncology local therapies and immunotherapy for the treatment of hepatocellular carcinoma
- Dong-Hyun Kim
- J Liver Cancer. 2022;22(2):93-102. Published online April 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.28
- 5,304 Views
- 166 Downloads
- 7 Citations
-
 Abstract
Abstract
 PDF
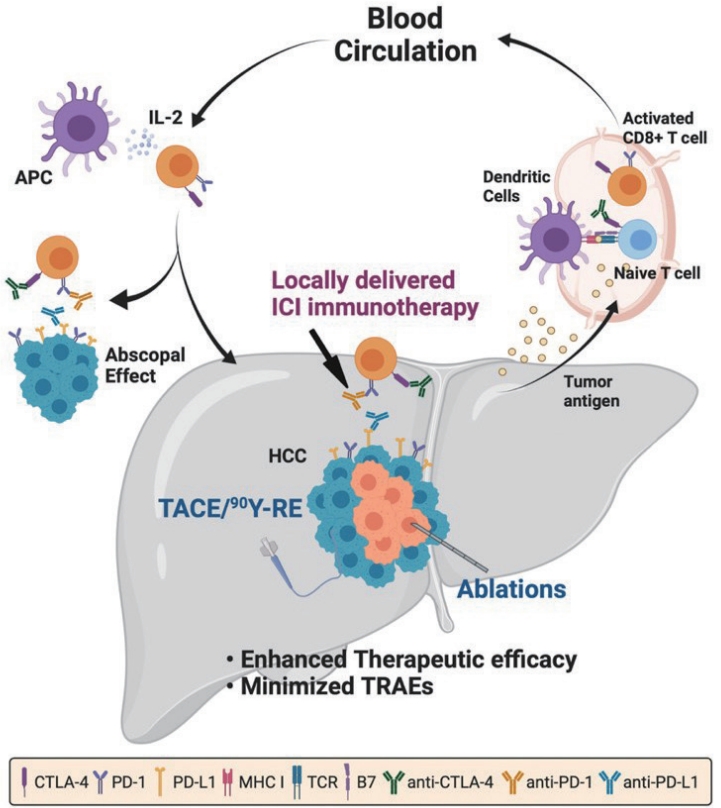
PDF - Interventional oncology (IO) local therapies of hepatocellular carcinoma (HCC) can activate anti-cancer immunity and it is potentially leading to an anti-cancer immunity throughout the body. For the development of an effective HCC treatment regime, great emphasis has been dedicated to different IO local therapy mediated immune modulation and possible combinations with immune checkpoint inhibitor immunotherapy. In this review paper, we summarize the status of combination of IO local therapy and immunotherapy, as well as the prospective role of therapeutic carriers and locally administered immunotherapy in advanced HCC.
-
Citations
Citations to this article as recorded by- Reduced-Dose or Discontinuation of Bevacizumab Might Be Considered after Variceal Bleeding in Patients with Hepatocellular Carcinoma Receiving Atezolizumab/Bevacizumab: Case Reports
Kyeong-Min Yeom, Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Medicina.2024; 60(1): 157. CrossRef - CT-guided high dose rate brachytherapy can induce multiple systemic proteins of proliferation and angiogenesis predicting outcome in HCC
Lukas Salvermoser, Shraga Nahum Goldberg, Marianna Alunni-Fabbroni, Philipp Maximilian Kazmierczak, Moritz Nikolaus Gröper, Jan Niklas Schäfer, Elif Öcal, Tanja Burkard, Stefanie Corradini, Najib Ben Khaled, Agnese Petrera, Moritz Wildgruber, Jens Ricke,
Translational Oncology.2024; 43: 101919. CrossRef - Complications of immunotherapy in advanced hepatocellular carcinoma
Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Journal of Liver Cancer.2024; 24(1): 9. CrossRef - Syngeneic N1-S1 Orthotopic Hepatocellular Carcinoma in Sprague Dawley Rat for the Development of Interventional Oncology-Based Immunotherapy: Survival Assay and Tumor Immune Microenvironment
Bongseo Choi, Jason Pe, Bo Yu, Dong-Hyun Kim
Cancers.2023; 15(3): 913. CrossRef - Preclinical Development and Validation of Translational Temperature Sensitive Iodized Oil Emulsion Mediated Transcatheter Arterial Chemo‐Immuno‐Embolization for the Treatment of Hepatocellular Carcinoma
Heegon Kim, Bongseo Choi, Samdeep K. Mouli, Hyunjun Choi, Kathleen R. Harris, Laura M. Kulik, Robert J. Lewandowski, Dong‐Hyun Kim
Advanced Healthcare Materials.2023;[Epub] CrossRef - The Current Evidence of Intensity-Modulated Radiotherapy for Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Won Il Jang, Sunmi Jo, Ji Eun Moon, Sun Hyun Bae, Hee Chul Park
Cancers.2023; 15(20): 4914. CrossRef - Inducing the Abscopal Effect in Liver Cancer Treatment: The Impact of Microwave Ablation Power Levels and PD-1 Antibody Therapy
Changli Liao, Guiyuan Zhang, Ruotong Huang, Linyuan Zeng, Bin Chen, Haitao Dai, Keyu Tang, Run Lin, Yonghui Huang
Pharmaceuticals.2023; 16(12): 1672. CrossRef
- Reduced-Dose or Discontinuation of Bevacizumab Might Be Considered after Variceal Bleeding in Patients with Hepatocellular Carcinoma Receiving Atezolizumab/Bevacizumab: Case Reports

- A clinical and pathological update on hepatocellular carcinoma
- Salvatore Lorenzo Renne, Luca Di Tommaso
- J Liver Cancer. 2022;22(1):14-22. Published online March 31, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.18

- 7,890 Views
- 501 Downloads
- 11 Citations
-
 Abstract
Abstract
 PDF
PDF - It is estimated that more than 1 million individuals will be affected annually by hepatocellular carcinoma (HCC) by 2025. HCC can be broadly grouped into two major molecular subgroups, each of which is characterized by specific morphological and phenotypic features that mirror the genetic background. The use of these tissue biomarkers in the daily practice of pathologists promises to better allocate patients with HCC with adequate treatments. In turn, this will likely boost the attitude of clinicians toward obtaining a pre-treatment biopsy.
-
Citations
Citations to this article as recorded by- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Jeong-Ju Yoo, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, Dong Ah Park
Current Oncology.2024; 31(1): 324. CrossRef - Comparison of Surgical Resection and Radiofrequency Ablation in Elderly Patients with Hepatocellular Carcinoma
Jun Il Kim, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park, Jeong-Ju Yoo
Digestive Diseases and Sciences.2024; 69(3): 1055. CrossRef - Identification of gallbladder cancer by direct near-infrared measurement of raw bile combined with two-trace two-dimensional correlation analysis
Eunjin Jang, Woosuk Sohng, Dongho Choi, Hoeil Chung
The Analyst.2023; 148(2): 374. CrossRef - Measurement of Heavy Metal and Antioxidant-Oxidant Levels in Tissues Obtained From Three Different Localizations of Explant Hepatectomy of Patients With Hepatocellular Carcinoma
Cemalettin Koc, Sami Akbulut, Kemal Baris Sarici, Muhammed Mehdi Uremis, Ufuk Gunay Dogan, Zeynep Kucukakcali, Ibrahim Umar Garzali, Ertugrul Karabulut, Yusuf Turkoz, Sezai Yilmaz
Transplantation Proceedings.2023; 55(5): 1262. CrossRef - Adding MRI as a Surveillance Test for Hepatocellular Carcinoma in Patients with Liver Cirrhosis Can Improve Prognosis
Su Jong Yu, Jeong-Ju Yoo, Dong Ho Lee, Su Jin Kim, Eun Ju Cho, Se Hyung Kim, Jeong-Hoon Lee, Yoon Jun Kim, Jeong Min Lee, Jae Young Lee, Jung-Hwan Yoon
Biomedicines.2023; 11(2): 382. CrossRef - Development of a sorafenib-loaded solid self-nanoemulsifying drug delivery system: Formulation optimization and characterization of enhanced properties
Chaemin Lim, Dayoon Lee, Mikyung Kim, Subin Lee, Yuseon Shin, Jacob D. Ramsey, Han-Gon Choi, Eun Seong Lee, Yu Seok Youn, Kyung Taek Oh
Journal of Drug Delivery Science and Technology.2023; 82: 104374. CrossRef - Validation of MELD 3.0 scoring system in East Asian patients with cirrhosis awaiting liver transplantation
Jeong-Ju Yoo, Jong-In Chang, Ji Eun Moon, Dong Hyun Sinn, Sang Gyune Kim, Young Seok Kim
Liver Transplantation.2023; 29(10): 1029. CrossRef - Higher Number of Tumor-Infiltrating PD-L1+ Cells Is Related to Better Response to Multikinase Inhibitors in Hepatocellular Carcinoma
Ji Won Han, Ji Hoon Kim, Dong Hyun Kim, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon, Jaegyoon Ahn, Hyun Yang, Pil Soo Sung
Diagnostics.2023; 13(8): 1453. CrossRef - Risk of dyslipidemia in chronic hepatitis B patients taking tenofovir alafenamide: a systematic review and meta-analysis
Eui Gwon Hwang, Eun-Ae Jung, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Hepatology International.2023; 17(4): 860. CrossRef - Recent application of artificial intelligence on histopathologic image-based prediction of gene mutation in solid cancers
Mohammad Rizwan Alam, Kyung Jin Seo, Jamshid Abdul-Ghafar, Kwangil Yim, Sung Hak Lee, Hyun-Jong Jang, Chan Kwon Jung, Yosep Chong
Briefings in Bioinformatics.2023;[Epub] CrossRef - Role of pelitinib in the regulation of migration and invasion of hepatocellular carcinoma cells via inhibition of Twist1
Sewoong Lee, Eunjeong Kang, Unju Lee, Sayeon Cho
BMC Cancer.2023;[Epub] CrossRef
- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis

Editorial
- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
- Won Hyeok Choe
- J Liver Cancer. 2022;22(1):1-3. Published online March 31, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.15
- 2,729 Views
- 90 Downloads
- 1 Citation
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Nomogram for predicting overall survival in patients with large (>5 cm) hepatocellular carcinoma based on real-world practice
Nalee Kim, Jeong Il Yu, Hee Chul Park, Jung Yong Hong, Ho Yeong Lim, Myung Ji Goh, Yong-Han Paik
Journal of Liver Cancer.2023; 23(2): 350. CrossRef
- Nomogram for predicting overall survival in patients with large (>5 cm) hepatocellular carcinoma based on real-world practice

Case Reports
- Long-term survival after CCRT and HAIC followed by ALPPS for hepatocellular carcinoma with portal vein invasion: a case report
- In-Jung Kim, Sung Hwan Yoo, Jung Il Lee, Kwan Sik Lee, Hyun Woong Lee, Jin Hong Lim
- J Liver Cancer. 2022;22(1):84-90. Published online March 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.07
- 2,816 Views
- 71 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - There are various methods for treating advanced hepatocellular carcinoma with portal vein invasion, such as systemic chemotherapy, transarterial chemoembolization, transarterial radioembolization, and concurrent chemoradiotherapy. These methods have similar clinical efficacy but are designed with a palliative aim. Herein, we report a case that experienced complete remission through “associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)” after concurrent chemoradiotherapy and hepatic artery infusion chemotherapy. In this patient, concurrent chemoradiotherapy and hepatic artery infusion chemotherapy induced substantial tumor shrinkage, and hypertrophy of the nontumor liver was sufficiently induced by portal vein ligation (stage 1 surgery) followed by curative resection (stage 2 surgery). Using this approach, long-term survival with no evidence of recurrence was achieved at 16 months. Therefore, the optimal use of ALPPS requires sufficient consideration in cases of significant hepatocellular carcinoma shrinkage for curative purposes.
-
Citations
Citations to this article as recorded by- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?

- Concurrent transarterial radioembolization and combination atezolizumab/ bevacizumab treatment of infiltrative hepatocellular carcinoma with portal vein tumor thrombosis: a case report
- Min Kyung Park, Su Jong Yu
- J Liver Cancer. 2022;22(1):69-74. Published online March 21, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.09
- 3,305 Views
- 107 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
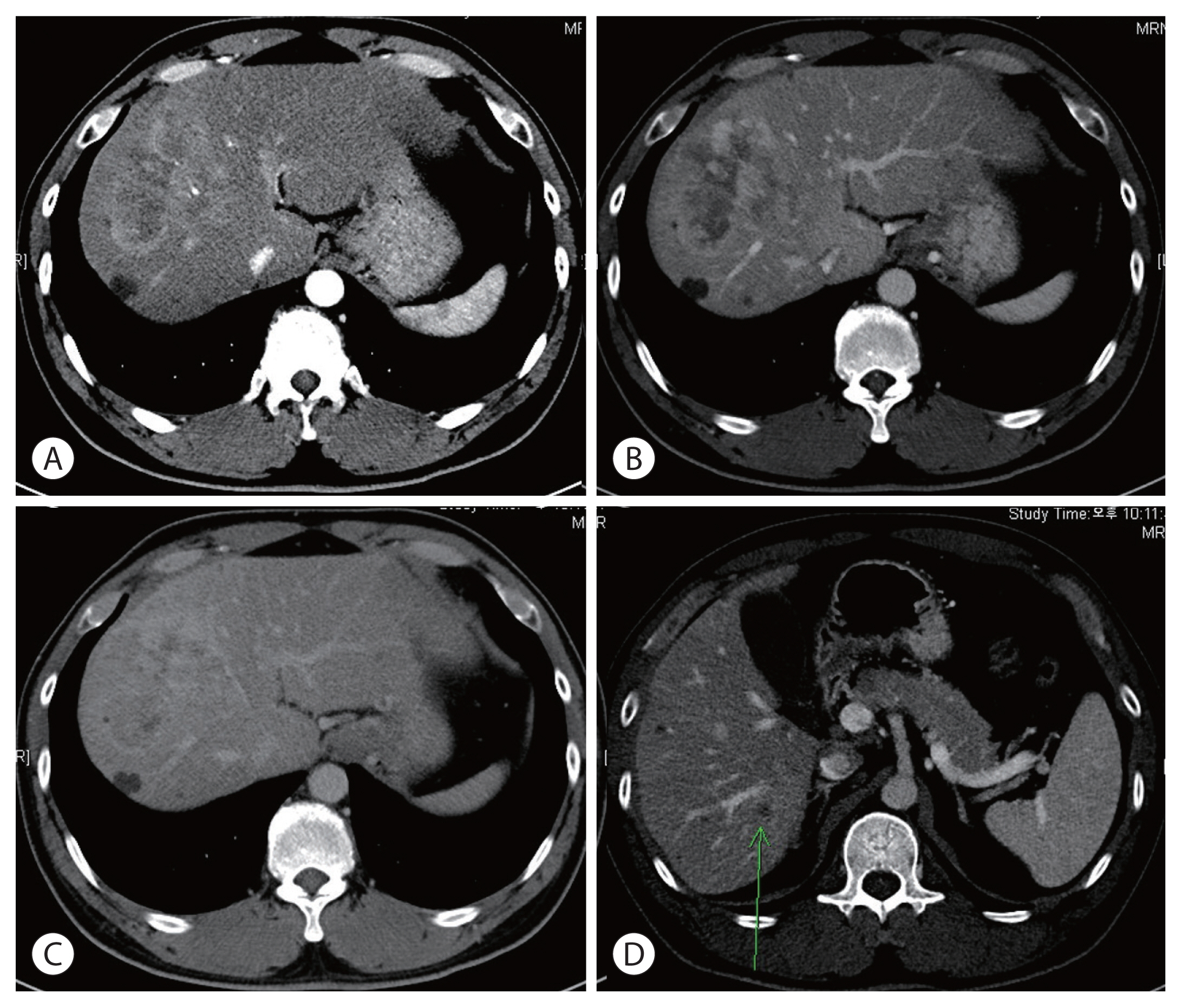
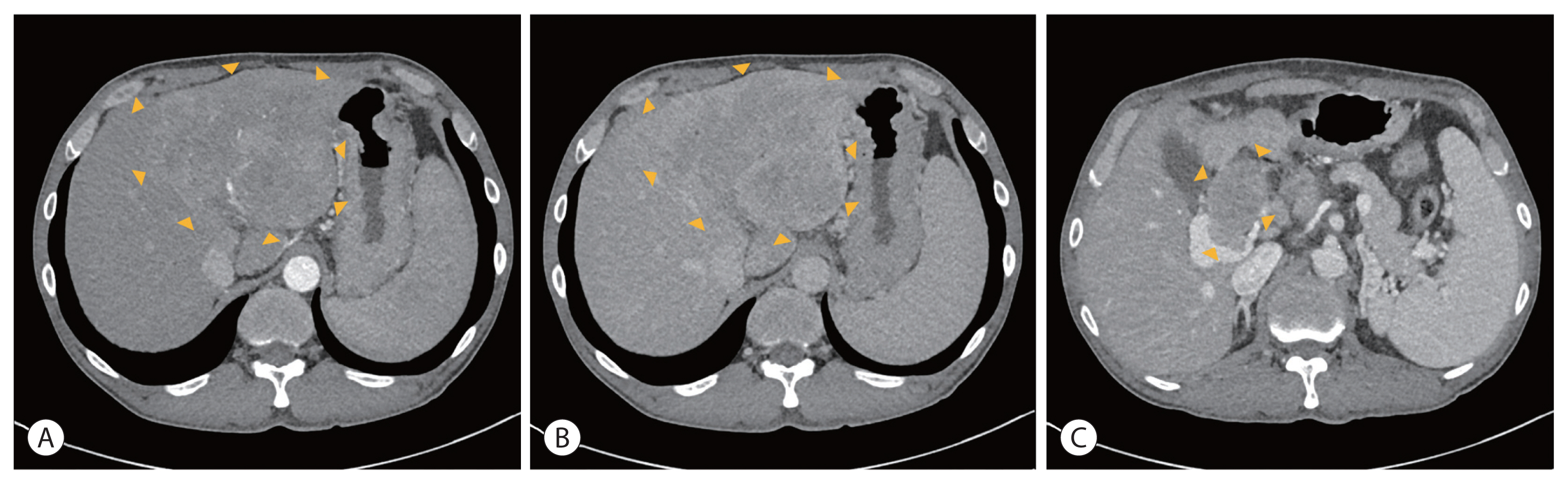
PDF - Treatment options for advanced hepatocellular carcinoma (HCC) have been rapidly evolving. Herein, we describe a patient with advanced HCC and portal vein tumor thrombosis (PVTT) who responded decisively to a multidisciplinary approach. The patient had an ill-defined infiltrative HCC (diffuse subtype), with several intrahepatic metastasis and tumor invasion of left portal vein. Concurrent use of transarterial radioembolization (TARE) and systemic therapeutics (atezolizumab + bevacizumab) ultimately proved successful. There was marked reduction in tumor volume after TARE and an additional three cycles of atezolizumab plus bevacizumab. This concurrent treatment was well tolerated, without adverse events during immunotherapy. The impressive results achieved suggest that concurrent TARE and combination atezolizumab/bevacizumab is a promising treatment approach for advanced HCC with PVTT.
-
Citations
Citations to this article as recorded by- Biologics, Immunotherapies, and Cytotoxic Chemotherapy for Hepatocellular Carcinoma following Current Recommendations by the BCLC: A Review of Agents
Rajangad S. Gurtatta, Sydney E. Whalen, Charles E. Ray
Seminars in Interventional Radiology.2024; 41(01): 084. CrossRef - Combining immunotherapy with transarterial radioembolization
ZeynepCeren Balaban Genc, Efe Soydemır, SevalAy Ersoy, Tunc Ones
Indian Journal of Nuclear Medicine.2023; 38(2): 145. CrossRef - The New Era of Systemic Treatment for Hepatocellular Carcinoma: From the First Line to the Optimal Sequence
Maria Cerreto, Ferdinando Cardone, Lucia Cerrito, Leonardo Stella, Francesco Santopaolo, Maria Pallozzi, Antonio Gasbarrini, Francesca Romana Ponziani
Current Oncology.2023; 30(10): 8774. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Biologics, Immunotherapies, and Cytotoxic Chemotherapy for Hepatocellular Carcinoma following Current Recommendations by the BCLC: A Review of Agents

Original Article
- Diagnostic performance of serum exosomal miRNA-720 in hepatocellular carcinoma
- Jeong Won Jang, Ji Min Kim, Hye Seon Kim, Jin Seoub Kim, Ji Won Han, Soon Kyu Lee, Heechul Nam, Pil Soo Sung, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon
- J Liver Cancer. 2022;22(1):30-39. Published online March 21, 2022
- DOI: https://doi.org/10.17998/jlc.2022.02.25

- 3,891 Views
- 132 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Hepatocellular carcinoma (HCC) is associated with poor prognosis, largely due to late detection. Highly accurate biomarkers are urgently needed to detect early-stage HCC. Our study aims to explore the diagnostic performance of serum exosomal microRNA (miR)-720 in HCC.
Methods
Exosomal miRNA was measured via quantitative real-time PCR. A correlation analysis of exosomal miR-720 and tumor or clinico-demographic data of patients with HCC was performed. The receiver operating characteristic (ROC) curve was used to assess the diagnostic capacity of serum exosomal miR-720 for HCC, in comparison with α-fetoprotein (AFP) and prothrombin induced by vitamin K absence or antagonist-II (PIVKA-II).
Results
MiR-720 was chosen as a potential HCC marker via miR microarray based on significant differential expression between tumor and non-tumor samples. Serum exosomal miR-720 was significantly upregulated in patients with HCC (n=114) versus other liver diseases (control, n=30), with a higher area under the ROC curve (AUC=0.931) than the other markers. Particularly, serum exosomal miR-720 showed superior performance in diagnosing small HCC (< 5 cm; AUC=0.930) compared with AFP (AUC=0.802) or PIVKA-II (AUC=0.718). Exosomal miR-720 levels showed marginal correlation with tumor size. The proportion of elevated miR-720 also increased with intrahepatic tumor stage progression. Unlike AFP or PIVKA-II showing a significant correlation with aminotransferase levels, the exosomal miR-720 level was not affected by aminotransferase levels.
Conclusions
Serum exosomal miR-720 is an excellent biomarker for the diagnosis of HCC, with better performance than AFP or PIVKA-II. Its diagnostic utility is maintained even in small HCC and is unaffected by aminotransferase levels.

Case Report
- Multidisciplinary treatment with immune checkpoint inhibitors for advanced stage hepatocellular carcinoma
- Ahlim Lee, Jaejun Lee, Hyun Yang, Soo-Yoon Sung, Chang Ho Jeon, Su Ho Kim, Moon Hyung Choi, Young Joon Lee, Ho Jong Chun, Si Hyun Bae
- J Liver Cancer. 2022;22(1):75-83. Published online March 18, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.04
- 4,031 Views
- 94 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is a cytotoxic chemotherapy-resistant tumor and most HCCs arise in a background of liver cirrhosis of various causes. Although the IMBrave150 trial showed remarkable advancements in the treatment of unresectable HCC with atezolizumab plus bevacizumab (AteBeva), therapeutic outcomes were unsatisfactory in more than half of the patients. Accordingly, many ongoing trials combine conventional modalities with new drugs such as immune checkpoint inhibitors for better treatment outcomes, and they are expected to benefit patients with limited responses to conventional treatment. Here, two patients with advanced stage HCC with preserved liver function and good performance status showed partial response after treatment with combination or sequential therapy of AteBeva, hepatic arterial infusion chemotherapy, radiation therapy, and transarterial chemoembolization. These findings indicate the efficacy of multidisciplinary treatment against advanced HCC. Additional studies are required to establish optimal treatment strategies.
-
Citations
Citations to this article as recorded by- Complications of immunotherapy in advanced hepatocellular carcinoma
Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Journal of Liver Cancer.2024; 24(1): 9. CrossRef - Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Complications of immunotherapy in advanced hepatocellular carcinoma

Original Article
- The effects of immune checkpoint modulators on the clinical course of patients with resectable hepatocellular carcinoma
- Jihyun An, Hyo Jeong Kang, Eunsil Yu, Han Chu Lee, Ju Hyun Shim
- J Liver Cancer. 2022;22(1):40-50. Published online March 17, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.06

- 3,370 Views
- 113 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Immune checkpoint proteins regulating T-cell mediated anti-tumor immunity have been reported to affect clinical outcomes in multiple malignancies. This study aimed to investigate the prognostic effect of histological expression of immune checkpoint proteins in patients with resected hepatocellular carcinoma (HCC).
Methods
A total of 221 patients with HCC who underwent curative resection were included. Expression of programmed-cell death ligand-1 (PD-L1) in tumor cells (tPD-L1) and tumor infiltrating mononuclear cells (TIMCs) (iPD-L1), programmed-cell death-1 in TIMCs (iPD-1), and cytotoxic T lymphocyte antigen-4 in TIMCs (iCTLA-4) were measured immunohistochemically.
Results
Histo-positivity for iCTLA-4, iPD-1, iPD-L1, and tPD-L1 was 32.1%, 42.5%, 35.3%, and 14.9%, respectively. Multivariate logistic analyses revealed that male sex and tumor >5 cm were variables related to iCTLA-4 positivity (odds ratio [OR], 0.46 and 1.94, respectively; P<0.05). Poor differentiation was related to PD-L1 expression in both tumor cells and TIMCs (OR, 2.88 and 3.46, respectively; P<0.05). Microvascular invasion was significantly associated only with iPD-L1 (OR, 2.24; P<0.05). In time-dependent outcome analyses, expression of immune checkpoint proteins in TIMCs (i.e., iCTLA-4, iPD-1, and iPD-L1) was significantly related to longer overall survival and non-cancer-related survival (all P<0.05), but not to time-to-recurrence or cancer-specific deaths. Concurrent activation of the PD-1:PD-L1 and CTLA-4 pathways predicted improved outcomes in terms of overall survival and non-cancer related survival (P=0.06 and P=0.03, respectively).
Conclusions
Immune checkpoint proteins upregulated in TIMCs in HCC tissues have individual and additive effects in prolonging the survival of patients, specifically in terms of survival not related to cancer recurrence.

Review Articles
- Recent updates on the classification of hepatoblastoma according to the International Pediatric Liver Tumors Consensus
- Se Un Jeong, Hyo Jeong Kang
- J Liver Cancer. 2022;22(1):23-29. Published online March 17, 2022
- DOI: https://doi.org/10.17998/jlc.2022.02.24
- 5,545 Views
- 477 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Hepatoblastoma is the most common pediatric liver malignancy and usually occurs within the first 3 years of life. In recent years, the overall incidence of hepatoblastoma has exhibited the greatest increase among all pediatric malignancies worldwide. The diagnosis of hepatoblastoma may be challenging due to the lack of a current consensus classification system. The International Pediatric Liver Tumors Consensus introduced guidelines and a consensus classification for the diagnosis of hepatoblastoma as either epithelial or mixed epithelial and mesenchymal and in the updated 5th edition of the World Health Organization Classification of Digestive System Tumors.
-
Citations
Citations to this article as recorded by- Adult hepatoblastoma: making the challenging distinction from hepatocellular carcinoma
Allison Kaye L. Pagarigan, Paulo Giovanni L. Mendoza
Journal of Liver Cancer.2023; 23(1): 219. CrossRef - Advances in Histological and Molecular Classification of Hepatocellular Carcinoma
Joon Hyuk Choi, Swan N. Thung
Biomedicines.2023; 11(9): 2582. CrossRef
- Adult hepatoblastoma: making the challenging distinction from hepatocellular carcinoma

- Radioembolization for hepatocellular carcinoma: what clinicians need to know
- Jin Woo Choi, Hyo-Cheol Kim
- J Liver Cancer. 2022;22(1):4-13. Published online February 23, 2022
- DOI: https://doi.org/10.17998/jlc.2022.01.16

- 7,731 Views
- 430 Downloads
- 8 Citations
-
 Abstract
Abstract
 PDF
PDF - Transarterial radioembolization (TARE) with yttrium 90 (90Y) has been used in the management of hepatocellular carcinoma (HCC) for more than 10 years in Korea. There are two types of 90Y radioactive microspheres available, namely, glass and resin microspheres, with comparable clinical outcomes. In general, TARE outperforms transarterial chemoembolization regarding post-embolization syndrome, time to progression, tumor downsizing for liver transplantation, and hospitalization stay. Although TARE is commonly recommended for patients with unresectable large HCCs, it can be an alternative to or performed in combination with ablation, surgical resection, and systemic treatment. This review aimed to address 90Y radioactive microspheres, patient selection, clinical outcomes, simulation tests, radioembolization procedures, follow-up imaging, and complications.
-
Citations
Citations to this article as recorded by- Unlocking Precision in Radioembolization: Navigating the Future of Holmium-166 Radioembolization Mapping and Lung Shunt Study by Implementing Scout Dosimetry
Peiman Habibollahi, Armeen Mahvash, Nima Kokabi, Nariman Nezami
CardioVascular and Interventional Radiology.2024; 47(4): 451. CrossRef - Feasibility of Liver Transplantation after 90Y Radioembolization: Lessons from a Radiation Protection Incident
Marine Soret, Jacques-Antoine Maisonobe, Philippe Maksud, Stéphane Payen, Manon Allaire, Eric Savier, Charles Roux, Charlotte Lussey-Lepoutre, Aurélie Kas
Health Physics.2024;[Epub] CrossRef - Liver-Directed Locoregional Therapies for Neuroendocrine Liver Metastases: Recent Advances and Management
Cody R. Criss, Mina S. Makary
Current Oncology.2024; 31(4): 2076. CrossRef - Transarterial chemoembolization as an alternative to radioembolization is associated with earlier tumor recurrence than in radioembolization-eligible patients
Sung Won Chung, Heejin Cho, Hyunjae Shin, Jeayeon Park, Ju Yeon Kim, Ji Hoon Hong, Moon Haeng Hur, Min Kyung Park, Yun Bin Lee, Su Jong Yu, Myungsu Lee, Yoon Jun Kim, Jin Chul Paeng, Jung-Hwan Yoon, Jin Wook Chung, Jeong-Hoon Lee, Hyo-Cheol Kim
Frontiers in Oncology.2023;[Epub] CrossRef - The evolution of immune checkpoint inhibitor combinations in advanced hepatocellular carcinoma – A systematic review
Brandon M. Meyers, Jennifer J. Knox, David M. Liu, Deanna McLeod, Ravi Ramjeesingh, Vincent C. Tam, Howard J. Lim
Cancer Treatment Reviews.2023; 118: 102584. CrossRef - Recent Advances in Image-Guided Locoregional Therapies for Primary Liver Tumors
Cody R. Criss, Mina S. Makary
Biology.2023; 12(7): 999. CrossRef - Multidisciplinary consensus recommendations for management of hepatocellular carcinoma in Middle East and North Africa region
Imam Waked, Sherif Alsammany, Sayed Hammad Tirmazy, Kakil Rasul, Jafar Bani‐Issa, Wael Abdel‐Razek, Ashraf Omar, Amr Shafik, Salem Eid, Amr Abdelaal, Ahmed Hosni, Gamal Esmat
Liver International.2023; 43(10): 2062. CrossRef - Impact of Low Skeletal Muscle Mass on Long-Term Outcomes in Hepatocellular Carcinoma Treated with Trans-Arterial Radioembolization: A Retrospective Multi-Center Study
Heechul Nam, Hyun Yang, Ho Soo Chun, Han Ah Lee, Joon Yeul Nam, Jeong Won Jang, Yeon Seok Seo, Do Young Kim, Yoon Jun Kim, Si Hyun Bae
Cancers.2023; 15(21): 5195. CrossRef
- Unlocking Precision in Radioembolization: Navigating the Future of Holmium-166 Radioembolization Mapping and Lung Shunt Study by Implementing Scout Dosimetry

Case Report
- Sorafenib combined with radiation therapy for advanced hepatocellular carcinoma with portal and hepatic vein invasion extending to the inferior vena cava: a complete response case according to modified RECIST criteria
- Yuri Cho, Bo Hyun Kim, Tae Hyun Kim, Young Hwan Koh, Joong-Won Park
- J Liver Cancer. 2022;22(1):63-68. Published online February 14, 2022
- DOI: https://doi.org/10.17998/jlc.2022.01.18

- 2,790 Views
- 91 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
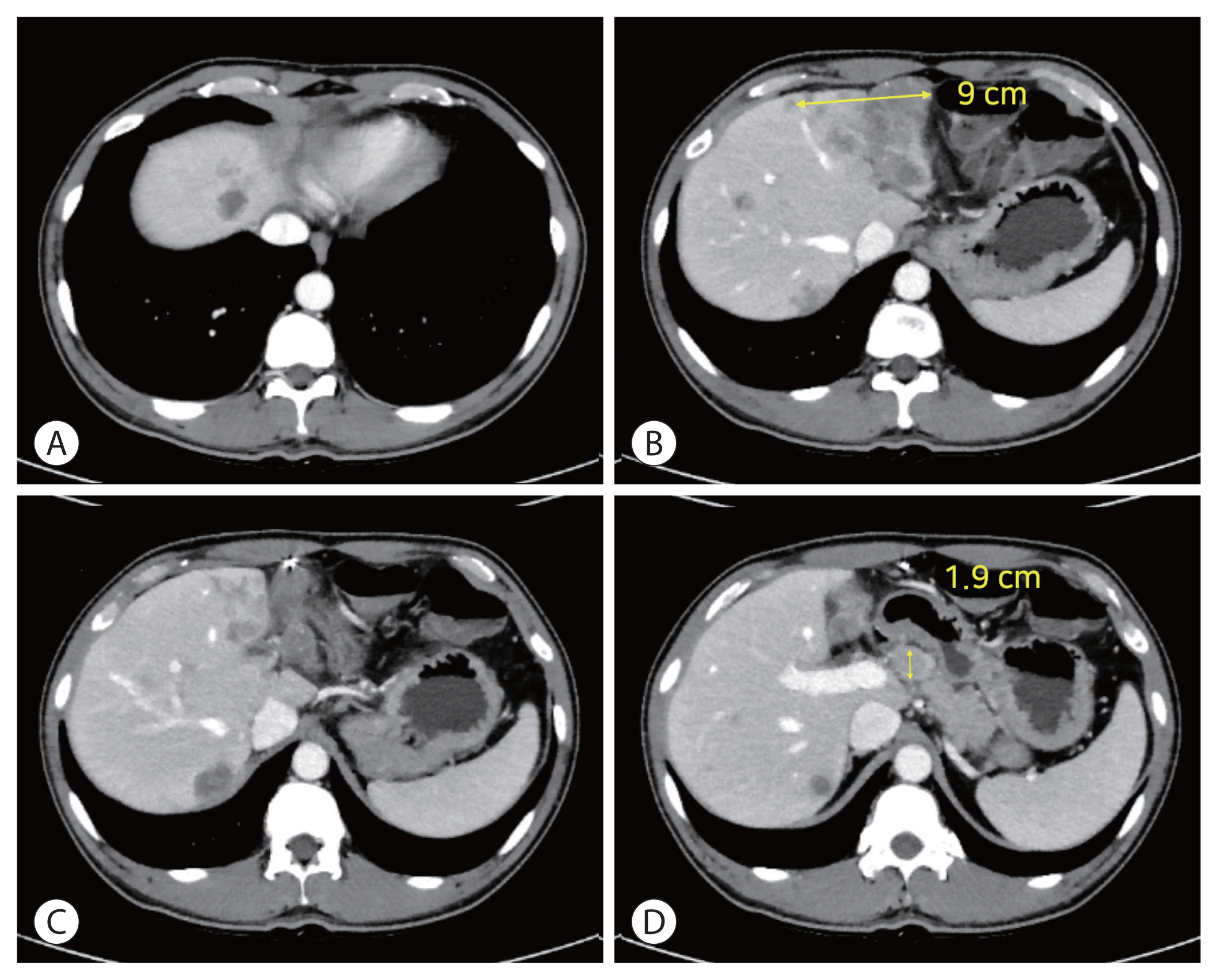
PDF - The prognosis of patients with advanced hepatocellular carcinoma (HCC) with tumor thrombus extending to the inferior vena cava (IVC) is extremely poor. Herein, we present a rare case of advanced HCC that was treated with sorafenib and radiotherapy, leading to complete remission. This patient had a 9 cm infiltrative HCC occupying almost the entire left lobe with a tumor thrombus extending through the hepatic vein, IVC, and left portal vein. The patient received 400 mg sorafenib twice daily. One year after the start of sorafenib, intensity-modulated radiation therapy for viable HCC and tumor thrombus was performed with a dose of 5,500 cGy. Twenty-seven months after the starting date of sorafenib, there was no intratumoral arterial enhancement, which suggested a complete response according to the modified RECIST criteria. This case suggests that the combination of sorafenib and radiotherapy might provide clinical benefits in patients with advanced HCC with IVC tumor thrombus.
-
Citations
Citations to this article as recorded by- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter