Search
- Page Path
- HOME > Search
Review Article
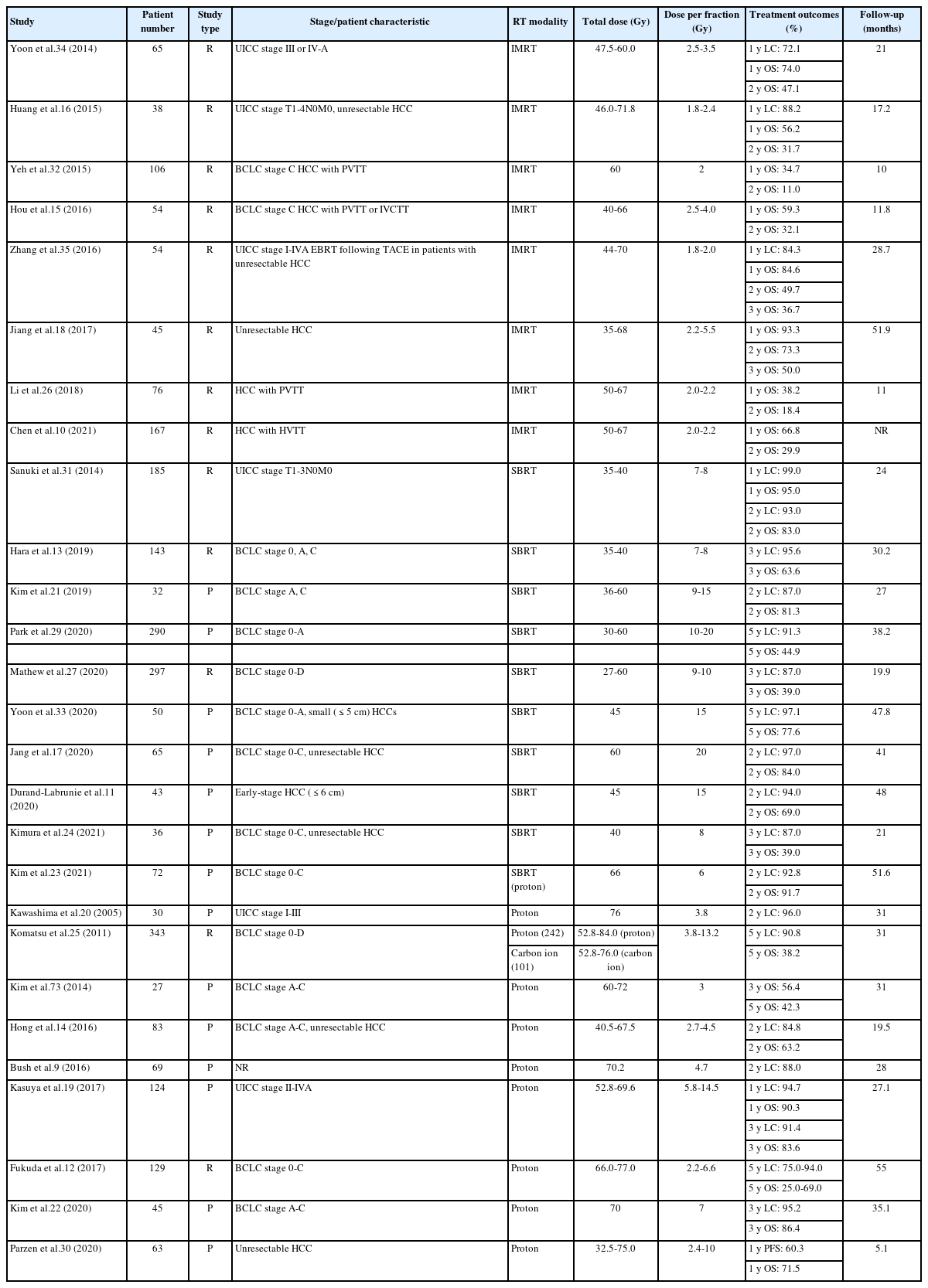
- Current perspectives on radiotherapy in hepatocellular carcinoma management: a comprehensive review
- Dowook Kim, Jun-Sang Kim
- J Liver Cancer. 2024;24(1):33-46. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.26
- 502 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
PDF - This review examines the transformative role of external beam radiotherapy (EBRT) in managing hepatocellular carcinoma (HCC), spotlighting the progression from traditional EBRT techniques to advanced modalities like intensity-modulated radiotherapy (RT), stereotactic body RT (SBRT), and innovative particle therapy, including proton beam therapy and carbon ion RT. These advancements have significantly improved the precision and efficacy of RT, marking a paradigm shift in the multimodal management of HCC, particularly in addressing complex cases and enhancing local tumor control. The review underscores the synergistic potential of integrating RT with other treatments like transarterial chemoembolization, systemic therapies such as sorafenib, and emerging immunotherapies, illustrating enhanced survival and disease control outcomes. The efficacy of RT is addressed for challenging conditions, including advanced HCC with macrovascular invasion, and RT modalities, like SBRT, are compared against traditional treatments like radiofrequency ablation for early-stage HCC. Additionally, the review accentuates the encouraging outcomes of particle therapy in enhancing local control and survival rates, minimizing treatment-related toxicity, and advocating for continued research and clinical trials. In conclusion, the integration of RT into multimodal HCC treatment strategies, coupled with the emergence of particle therapy, is crucial for advancing oncologic management, emphasizing the need for relentless innovation and personalized treatment approaches.

Letter to the Editor
- Letter regarding “Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab”
- Sun Hyun Bae, Hee Chul Park
- J Liver Cancer. 2023;23(2):402-404. Published online September 8, 2023
- DOI: https://doi.org/10.17998/jlc.2023.08.18
- 670 Views
- 32 Downloads

Original Articles
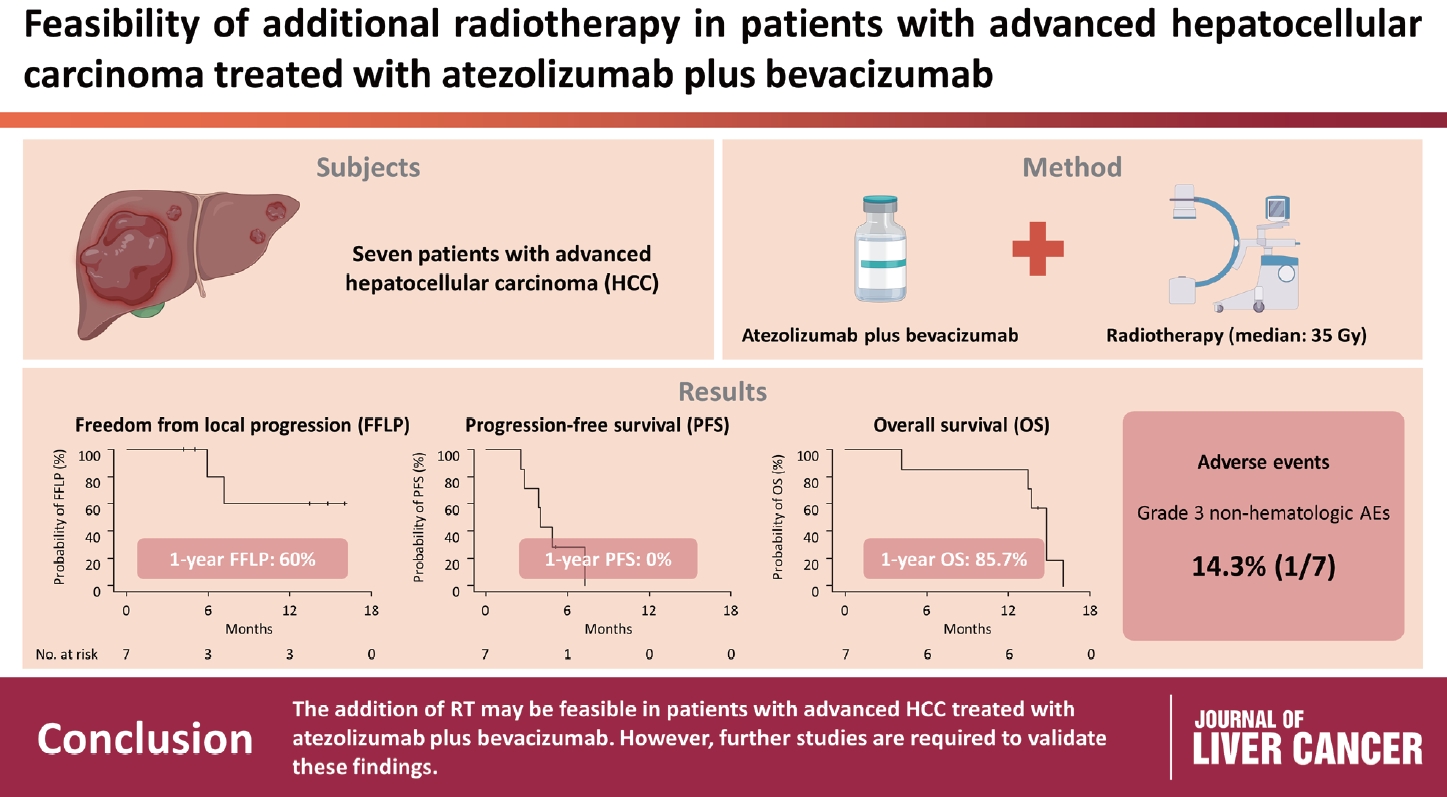
- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
- Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
- J Liver Cancer. 2023;23(2):330-340. Published online May 16, 2023
- DOI: https://doi.org/10.17998/jlc.2023.04.14
- 1,757 Views
- 112 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Radiotherapy (RT) is an effective local treatment for hepatocellular carcinoma (HCC). However, whether additional RT is safe and effective in patients with advanced HCC receiving atezolizumab plus bevacizumab remains unclear. This retrospective cohort study aimed to evaluate the feasibility of additional RT in these patients.
Methods
Between March and October 2021, we retrospectively analyzed seven patients with advanced HCC who received RT during treatment with atezolizumab plus bevacizumab. The median prescribed RT dose was 35 Gy (range, 33–66). Freedom from local progression (FFLP), progression-free survival (PFS), and overall survival (OS) after RT were analyzed.
Results
The median follow-up duration after RT was 14.2 months (range, 10.0–18.6). Of the seven patients, disease progression was noted in six (85.7%), the sites of disease progression were local in two (28.6%), intrahepatic in four (57.1%), and extrahepatic in four (57.1%). The median time of FFLP was not reached, and PFS and OS times were 4.0 (95% confidence interval [CI], 3.6–4.5) and 14.8% (95% CI, 12.5–17.2) months, respectively. The 1-year FFLP, PFS, and OS rates were 60% (95% CI, 43.8–76.2), 0%, and 85.7% (95% CI, 75.9–95.5), respectively. Grade 3 or higher hematologic adverse events (AEs) were not observed, but grade 3 nonhematologic AEs unrelated to RT were observed in one patient.
Conclusions
The addition of RT may be feasible in patients with advanced HCC treated with atezolizumab plus bevacizumab. However, further studies are required to validate these findings. -
Citations
Citations to this article as recorded by- Letter regarding “Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab”
Sun Hyun Bae, Hee Chul Park
Journal of Liver Cancer.2023; 23(2): 402. CrossRef
- Letter regarding “Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab”

- Subclassification of advanced-stage hepatocellular carcinoma with macrovascular invasion: combined transarterial chemoembolization and radiotherapy as an alternative first-line treatment
- Sujin Jin, Won-Mook Choi, Ju Hyun Shim, Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jinhong Jung, Sang Min Yoon, Jonggi Choi
- J Liver Cancer. 2023;23(1):177-188. Published online March 23, 2023
- DOI: https://doi.org/10.17998/jlc.2023.03.04

- 1,485 Views
- 88 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
The Barcelona Clinic Liver Cancer (BCLC) guidelines recommend systemic therapy as the only first-line treatment for patients with BCLC stage C hepatocellular carcinoma (HCC) despite its heterogeneity of disease extent. We aimed to identify patients who might benefit from combined transarterial chemoembolization (TACE) and radiation therapy (RT) by subclassifying BCLC stage C.
Methods
A total of 1,419 treatment-naïve BCLC stage C patients with macrovascular invasion (MVI) who were treated with combined TACE and RT (n=1,115) or systemic treatment (n=304) were analyzed. The primary outcome was overall survival (OS). Factors associated with OS were identified and assigned points by the Cox model. The patients were subclassified into three groups based on these points.
Results
The mean age was 55.4 years, and 87.8% were male. The median OS was 8.3 months. Multivariate analysis revealed a significant association of Child-Pugh B, infiltrative-type tumor or tumor size ≥10 cm, main or bilateral portal vein invasion, and extrahepatic metastasis with poor OS. The sub-classification was categorized into low (point ≤1), intermediate (point=2), and high (point ≥3) risks based on the sum of points (range, 0–4). The OS in the low, intermediate, and high-risk groups was 22.6, 8.2, and 3.8 months, respectively. In the low and intermediate-risk groups, patients treated with combined TACE and RT exhibited significantly longer OS (24.2 and 9.5 months, respectively) than those who received systemic treatment (6.4 and 5.1 months, respectively; P<0.0001).
Conclusions
Combined TACE and RT may be considered as a first-line treatment option for HCC patients with MVI when classified into low- and intermediate-risk groups. -
Citations
Citations to this article as recorded by- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
Journal of Liver Cancer.2024; 24(1): 102. CrossRef - Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
Journal of Liver Cancer.2024; 24(1): 81. CrossRef - How to optimize the treatment strategy for advanced-stage hepatocellular carcinoma with macrovascular invasion
Beom Kyung Kim
Journal of Liver Cancer.2023; 23(1): 121. CrossRef
- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis

Case Reports
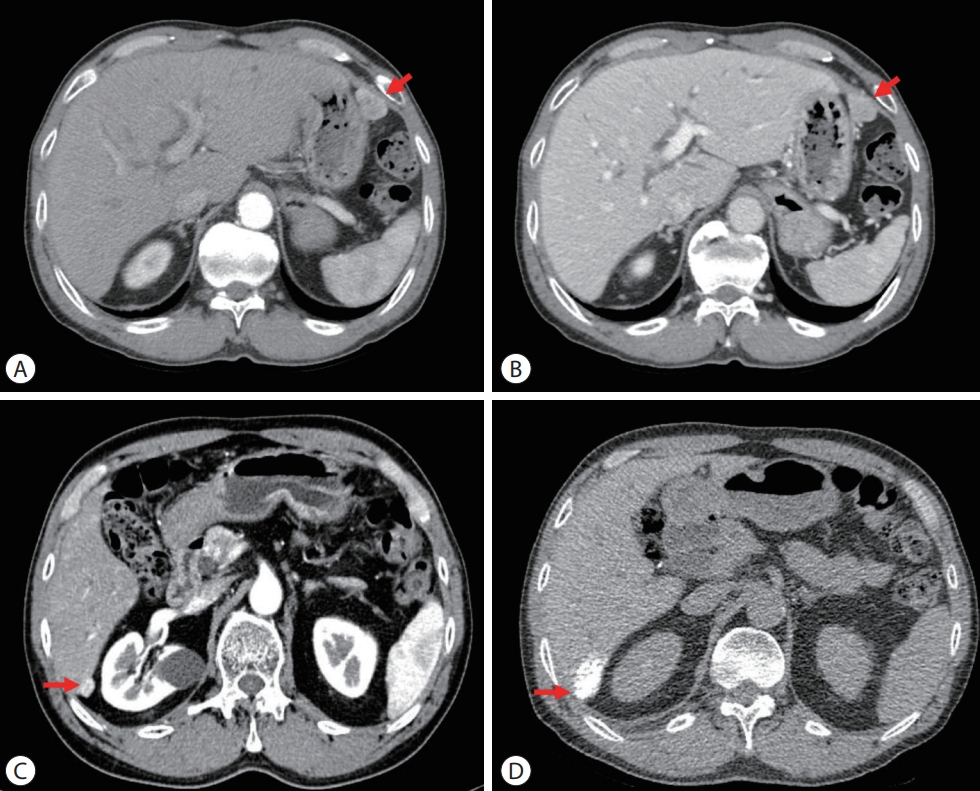
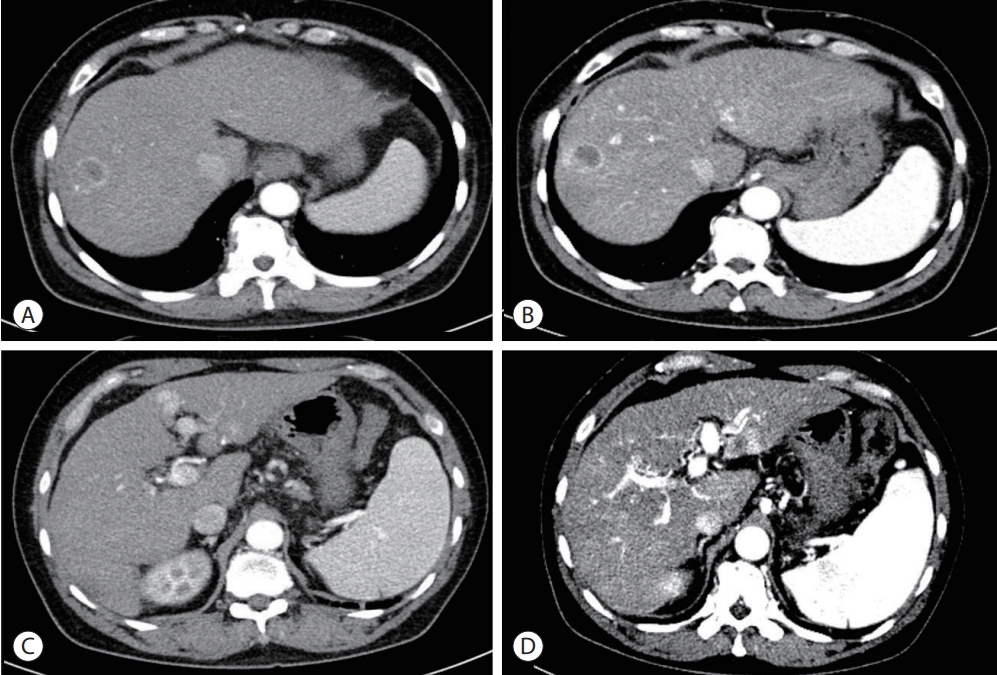
- Favorable response of hepatocellular carcinoma with portal vein tumor thrombosis after radiotherapy combined with atezolizumab plus bevacizumab
- Yong Tae Kim, Jina Kim, Jinsil Seong
- J Liver Cancer. 2023;23(1):225-229. Published online March 16, 2023
- DOI: https://doi.org/10.17998/jlc.2023.02.27

- 1,071 Views
- 69 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Recently, the superiority of atezolizumab plus bevacizumab (AteBeva) over sorafenib was proven in the IMbrave150 trial, and AteBeva became the first-line systemic treatment for untreated, unresectable hepatocellular carcinoma (HCC). While the results are encouraging, more than half of patients with advanced HCC are still being treated in a palliative setting. Radiotherapy (RT) is known to induce immunogenic effects that may enhance the therapeutic efficacy of immune checkpoint inhibitors. Herein, we report the case of a patient with advanced HCC with massive portal vein tumor thrombosis treated with a combination of RT and AteBeva, who showed near complete response in tumor thrombosis and favorable response to HCC. Although this is a rare case, it shows the importance of reducing the tumor burden via RT to combination immunotherapy in patients with advanced HCC.
-
Citations
Citations to this article as recorded by- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Carbon Ion Radiotherapy in the Treatment of Hepatocellular Carcinoma
Hwa Kyung Byun, Changhwan Kim, Jinsil Seong
Clinical and Molecular Hepatology.2023; 29(4): 945. CrossRef
- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab

- A case of nearly complete response in hepatocellular carcinoma with disseminated lung metastasis by combination therapy of nivolumab and ipilimumab after treatment failure of atezolizumab plus bevacizumab
- Hyung Jun Kim, Sang Youn Hwang, Jung Woo Im, Ki Jeong Jeon, Wan Jeon
- J Liver Cancer. 2023;23(1):213-218. Published online March 9, 2023
- DOI: https://doi.org/10.17998/jlc.2023.02.23

- 950 Views
- 65 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Recently, the efficacy of immuno-oncologic agents for advanced hepatocellular carcinoma (HCC) has been proven in several trials. In particular, atezolizumab with bevacizumab (AteBeva), as a first-line therapy for advanced HCC, has shown tremendous advances in the IMBrave150 study. However, second or third-line therapy after treatment failure with AteBeva has not been firmly established. Moreover, clinicians have continued their attempts at multidisciplinary treatment that includes other systemic therapy and radiotherapy (RT). Here, we report a case that showed a near complete response (CR) of lung metastasis to nivolumab with ipilimumab therapy after achieving a near CR of intrahepatic tumor using sorafenib and RT in a patient with advanced HCC who had experienced treatment failure of AteBeva.
-
Citations
Citations to this article as recorded by- Systemic Therapy for Advanced Hepatocellular Carcinoma: ASCO Guideline Update
John D. Gordan, Erin B. Kennedy, Ghassan K. Abou-Alfa, Eliza Beal, Richard S. Finn, Terence P. Gade, Laura Goff, Shilpi Gupta, Jennifer Guy, Hang T. Hoang, Renuka Iyer, Ishmael Jaiyesimi, Minaxi Jhawer, Asha Karippot, Ahmed O. Kaseb, R. Kate Kelley, Jerem
Journal of Clinical Oncology.2024;[Epub] CrossRef
- Systemic Therapy for Advanced Hepatocellular Carcinoma: ASCO Guideline Update

- A case of successful surgical treatment for peritoneal seeding of hepatocellular carcinoma after radiotherapy and atezolizumab plus bevacizumab combination treatment
- Yuri Cho, Bo Hyun Kim, Tae Hyun Kim, Young Hwan Koh, Joong-Won Park
- J Liver Cancer. 2023;23(1):206-212. Published online February 24, 2023
- DOI: https://doi.org/10.17998/jlc.2023.02.09
- 1,449 Views
- 58 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Peritoneal seeding of hepatocellular carcinoma (HCC) is incurable and has poor prognosis. A 68-year-old man underwent surgical resection for a 3.5 cm single nodular HCC at the tip of segment 3 and transarterial chemoembolization for a 1.5 cm-sized recurrent HCC at the tip of segment 6. 3 months later, an increasing 1 cm pelvic nodule on the rectovesical pouch warranted radiotherapy. Although it stabilized, a new 2.7 cm-sized peritoneal nodule in the right upper quadrant (RUQ) omentum appeared 3.5 years after radiotherapy. Hence, omental mass and small bowel mesentery mass excision were performed. 3 years later, recurrent peritoneal metastases in the RUQ omentum and rectovesical pouch progressed. 33 cycles of atezolizumab and bevacizumab treatment elicited stable disease response. Finally, laparoscopic left pelvic peritonectomy was performed without tumor recurrence. Herein, we present a case of HCC with peritoneal seeding that was successfully treated with surgery after radiotherapy and systemic therapy, leading to complete remission.
-
Citations
Citations to this article as recorded by- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef
- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab

Original Article
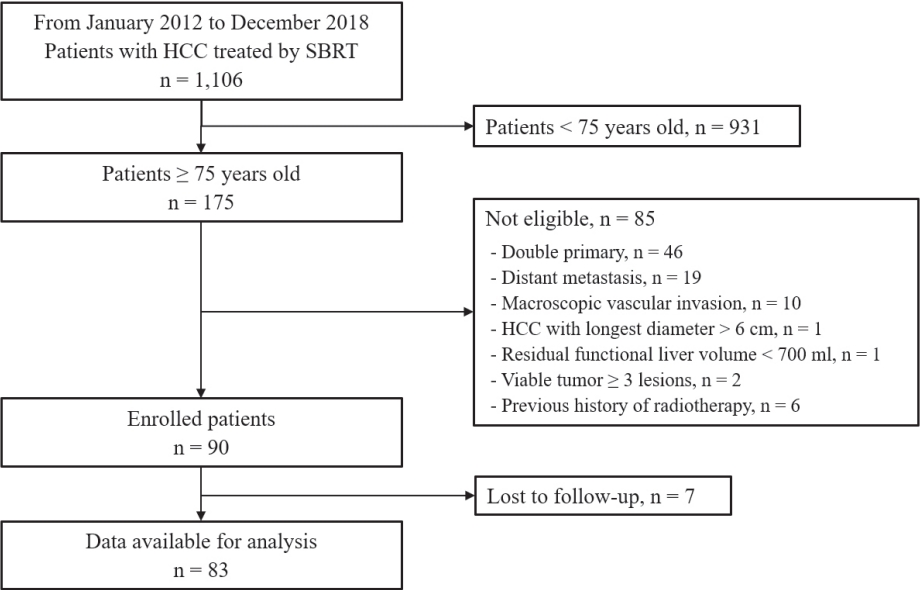
- Stereotactic body radiation therapy for elderly patients with small hepatocellular carcinoma: a retrospective observational study
- Jeong Yun Jang, Jinhong Jung, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jin-hong Park, Sang Min Yoon
- J Liver Cancer. 2022;22(2):136-145. Published online September 16, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.18
- 2,956 Views
- 73 Downloads
- 5 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
We aimed to investigate the efficacy and safety of stereotactic body radiation therapy (SBRT) in elderly patients with small hepatocellular carcinomas (HCC).
Methods
Eighty-three patients (89 lesions) with HCC who underwent SBRT between January 2012 and December 2018 were reviewed in this retrospective observational study. The key inclusion criteria were as follows: 1) age ≥75 years, 2) contraindications for hepatic resection or percutaneous ablative therapies, 3) no macroscopic vascular invasion, and 4) no extrahepatic metastasis.
Results
The patients were 75-90 years of age, and 49 (59.0%) of them were male. Most patients (94.0%) had an Eastern Cooperative Oncology Group performance status of 0 or 1. Seventy-four patients (89.2%) had Child-Pugh class A hepatic function before SBRT. The median tumor size was 1.6 cm (range, 0.7-3.5). The overall median follow-up period was 34.8 months (range, 7.3-99.3). The 5-year local tumor control rate was 90.1%. The 3-year and 5-year overall survival rate was 57.1% and 40.7%, respectively. Acute toxicity grade ≥3 was observed in three patients (3.6%) with elevated serum hepatic enzymes; however, no patient experienced a worsening of the Child-Pugh score to ≥2 after SBRT. None of the patients developed late toxicity (grade ≥3).
Conclusions
SBRT is a safe treatment option with a high local control rate in elderly patients with small HCC who are not eligible for other curative treatments. -
Citations
Citations to this article as recorded by- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis
Jeong-Ju Yoo, Sujin Koo, Gi Hong Choi, Min Woo Lee, Seungeun Ryoo, Jungeun Park, Dong Ah Park
Current Oncology.2024; 31(1): 324. CrossRef - Radiotherapy trend in elderly hepatocellular carcinoma: retrospective analysis of patients diagnosed between 2005 and 2017
Bong Kyung Bae, Jeong Il Yu, Hee Chul Park, Myung Ji Goh, Yong-Han Paik
Radiation Oncology Journal.2023; 41(2): 98. CrossRef - Loco-regional therapies competing with radiofrequency ablation in potential indications for hepatocellular carcinoma: a network meta-analysis
Ha Il Kim, Jihyun An, Seungbong Han, Ju Hyun Shim
Clinical and Molecular Hepatology.2023; 29(4): 1013. CrossRef - Has the growing evidence of radiotherapy for hepatocellular carcinoma increased the use of radiotherapy in elderly patients?
Tae Hyun Kim
Radiation Oncology Journal.2023; 41(3): 141. CrossRef - Chronic Liver Disease in the Older Patient—Evaluation and Management
Daniel Anthony DiLeo, Tolga Gidener, Ayse Aytaman
Current Gastroenterology Reports.2023; 25(12): 390. CrossRef
- Radiofrequency Ablation versus Surgical Resection in Elderly Hepatocellular Carcinoma: A Systematic Review and Meta-Analysis

Case Reports
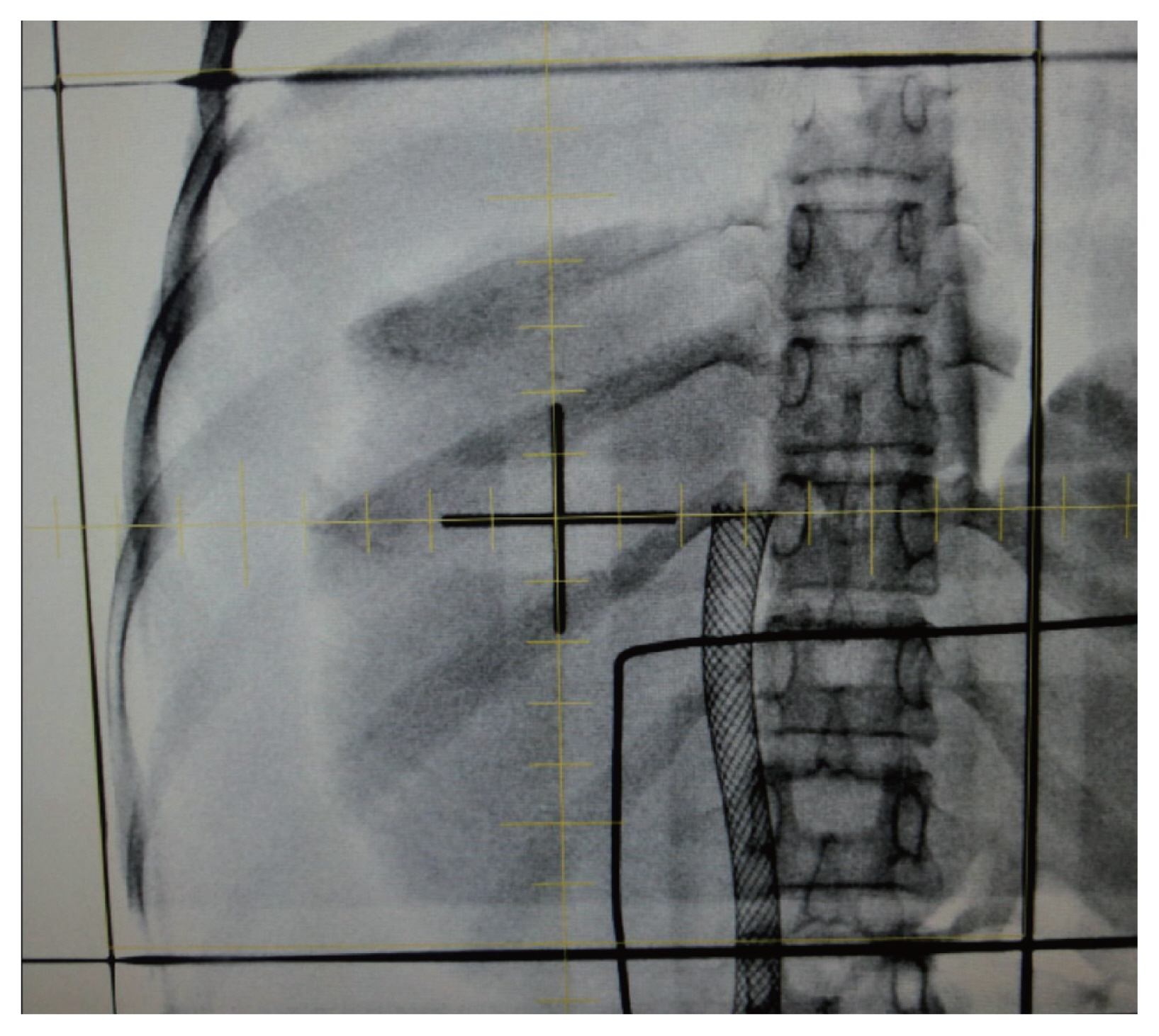
- Novel management of expected post-radiotherapy complications in hepatocellular carcinoma patients: a case report
- Sung Hoon Chang, Tae Suk Kim, Yong Hwan Jeon, Nuri Hyun Jung, Dae Hee Choi
- J Liver Cancer. 2022;22(2):183-187. Published online August 24, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.03
- 1,658 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
PDF - In recent years, radiotherapy (RT) has been used to treat hepatocellular carcinoma (HCC) at each stage. This clinical trend has developed with the increasing improvement of RT techniques, which show clinical results comparable to those of other treatment modalities. Intensity-modulated radiotherapy uses a high radiation dose to improve treatment effectiveness. However, the associated radiation toxicity can damage adjacent organs. Radiation-induced gastric damage with gastric ulcers is a complication of RT. This report presents a novel management strategy for preventing post-RT gastric ulcers. We present the case of a 53-year-old male patient diagnosed with HCC, who experienced gastric ulcer after RT. Before the second round of RT, the patient was administered a gas-foaming agent, which was effective in preventing RT complications.

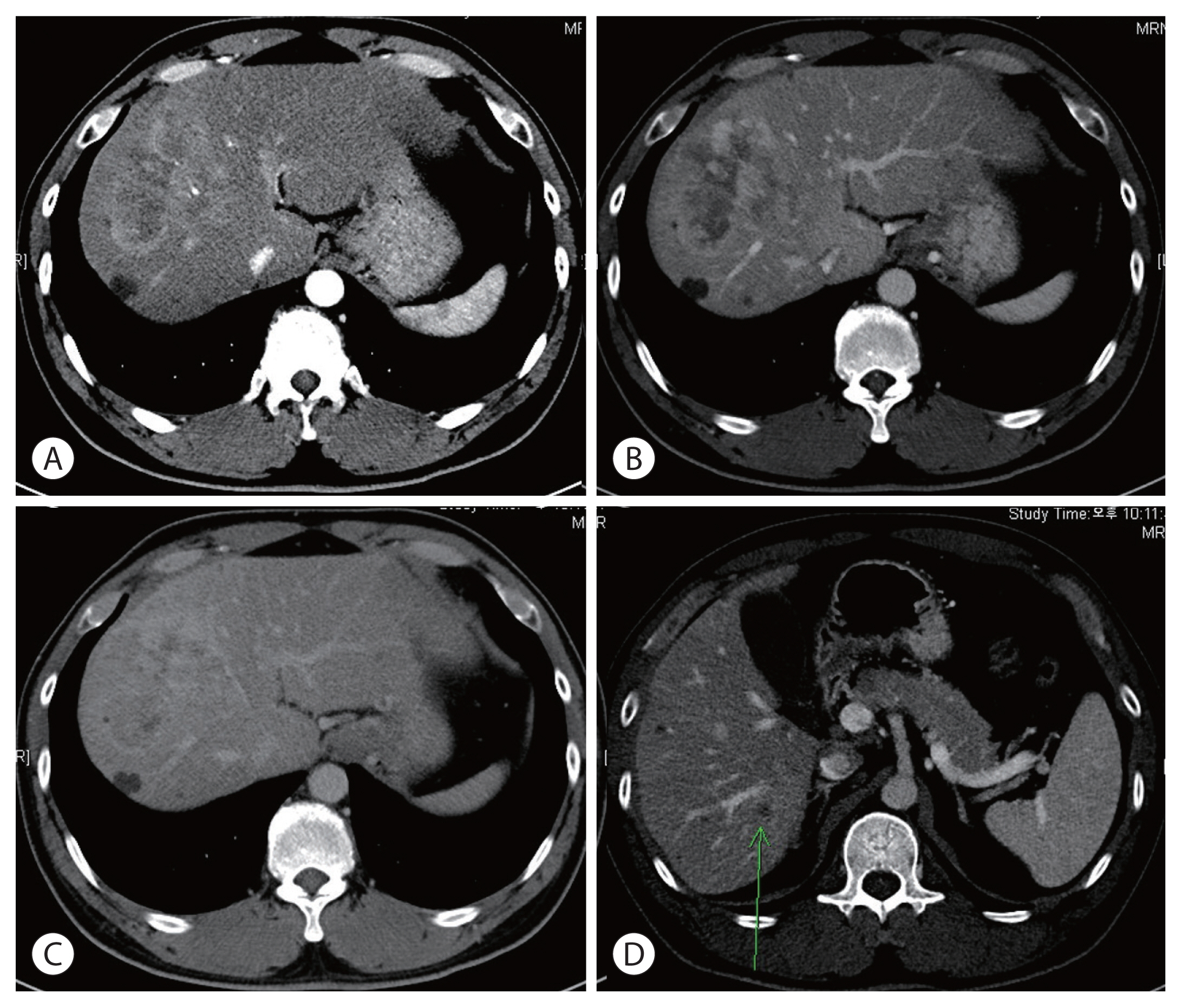
- Long-term survival after CCRT and HAIC followed by ALPPS for hepatocellular carcinoma with portal vein invasion: a case report
- In-Jung Kim, Sung Hwan Yoo, Jung Il Lee, Kwan Sik Lee, Hyun Woong Lee, Jin Hong Lim
- J Liver Cancer. 2022;22(1):84-90. Published online March 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.07
- 2,786 Views
- 70 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - There are various methods for treating advanced hepatocellular carcinoma with portal vein invasion, such as systemic chemotherapy, transarterial chemoembolization, transarterial radioembolization, and concurrent chemoradiotherapy. These methods have similar clinical efficacy but are designed with a palliative aim. Herein, we report a case that experienced complete remission through “associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)” after concurrent chemoradiotherapy and hepatic artery infusion chemotherapy. In this patient, concurrent chemoradiotherapy and hepatic artery infusion chemotherapy induced substantial tumor shrinkage, and hypertrophy of the nontumor liver was sufficiently induced by portal vein ligation (stage 1 surgery) followed by curative resection (stage 2 surgery). Using this approach, long-term survival with no evidence of recurrence was achieved at 16 months. Therefore, the optimal use of ALPPS requires sufficient consideration in cases of significant hepatocellular carcinoma shrinkage for curative purposes.
-
Citations
Citations to this article as recorded by- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?

- Sorafenib combined with radiation therapy for advanced hepatocellular carcinoma with portal and hepatic vein invasion extending to the inferior vena cava: a complete response case according to modified RECIST criteria
- Yuri Cho, Bo Hyun Kim, Tae Hyun Kim, Young Hwan Koh, Joong-Won Park
- J Liver Cancer. 2022;22(1):63-68. Published online February 14, 2022
- DOI: https://doi.org/10.17998/jlc.2022.01.18

- 2,751 Views
- 90 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - The prognosis of patients with advanced hepatocellular carcinoma (HCC) with tumor thrombus extending to the inferior vena cava (IVC) is extremely poor. Herein, we present a rare case of advanced HCC that was treated with sorafenib and radiotherapy, leading to complete remission. This patient had a 9 cm infiltrative HCC occupying almost the entire left lobe with a tumor thrombus extending through the hepatic vein, IVC, and left portal vein. The patient received 400 mg sorafenib twice daily. One year after the start of sorafenib, intensity-modulated radiation therapy for viable HCC and tumor thrombus was performed with a dose of 5,500 cGy. Twenty-seven months after the starting date of sorafenib, there was no intratumoral arterial enhancement, which suggested a complete response according to the modified RECIST criteria. This case suggests that the combination of sorafenib and radiotherapy might provide clinical benefits in patients with advanced HCC with IVC tumor thrombus.
-
Citations
Citations to this article as recorded by- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab

- Curative liver transplantation after lung resection for advanced hepatocellular carcinoma with lung metastasis and inferior vena cava tumor thrombosis: a case report
- Dong Jin Joo, Do Young Kim, Jinsil Seong, Hyun Jeong Kim, Jae Geun Lee, Dai Hoon Han, Gi Hong Choi, Myoung Soo Kim, Jin Sub Choi, Soon Il Kim
- J Liver Cancer. 2021;21(2):181-186. Published online September 30, 2021
- DOI: https://doi.org/10.17998/jlc.2021.09.08

- 3,613 Views
- 91 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) with distant metastasis is an absolute contraindication for liver transplantation (LT). However, it is still unclear whether LT is feasible or acceptable in such patients, albeit after being treated with a multidisciplinary approach and after any metastatic lesion is ruled out. We report one such successful treatment with living donor LT (LDLT) after completely controlling far-advanced HCC with inferior vena cava tumor thrombosis and multiple lung metastases. The patient has been doing well without HCC recurrence for eight years since LDLT. The current patient could be an anecdotal case, but provides a case for expanding LDLT indications in the context of advanced HCC and suchlike.
-
Citations
Citations to this article as recorded by- Inferior Vena Cava Thrombectomy and Stenting as Bridge to Liver Transplantation After Radiotherapy-Induced Thrombosis
Raphael PH Meier, Shani Kamberi, Josue Alvarez-Casas, Barton F. Lane, Chandra S. Bhati, Saad Malik, William Twaddell, Kirti Shetty, Adam Fang, Hyun S. Kim, Daniel G. Maluf
Progress in Transplantation.2023;[Epub] CrossRef
- Inferior Vena Cava Thrombectomy and Stenting as Bridge to Liver Transplantation After Radiotherapy-Induced Thrombosis

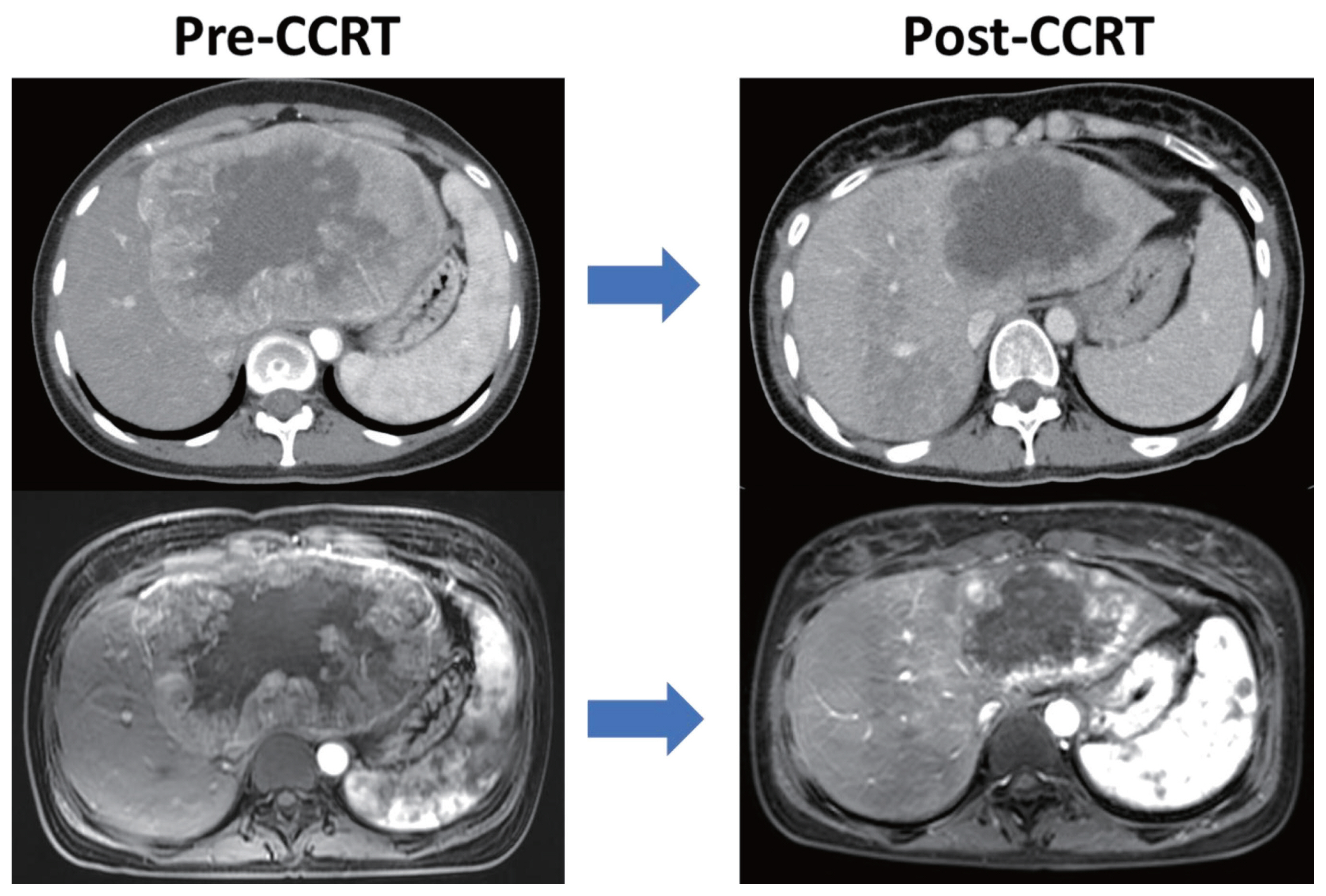
- Long-term survival after multimodal treatment involving radiotherapy for huge hepatocellular carcinoma with oligometastasis: a case report
- Byung Min Lee, Jinsil Seong
- J Liver Cancer. 2021;21(2):163-168. Published online September 2, 2021
- DOI: https://doi.org/10.17998/jlc.2021.08.06
- 2,560 Views
- 75 Downloads
-
 Abstract
Abstract
 PDF
PDF - The clinical efficacy of local ablative treatment for oligometastasis is widely accepted in most cancers. However, due to limited data, this has not been the case for hepatocellular carcinoma (HCC). Here, we report a case of pulmonary oligometastasis of a huge HCC that was treated by multimodality with liver-directed concurrent chemoradiotherapy (CCRT) plus subsequent resection of the primary lesion and local ablative radiotherapy (RT) for subsequent lung oligometastatic lesions. In this patient, liver-directed CCRT induced significant tumor shrinkage with compensatory hypertrophy of the non-tumor liver, followed by curative resection. Surgical resection of the first and second pulmonary metastatic lesions as well as local ablative RT of the third lesion achieved complete tumor regression, which led to long-term survival of 6 years. Therefore, the active use of local ablative RT requires full consideration in cases of oligometastatic HCC.

Review Article
- Differences in radiotherapy application according to regional disease characteristics of hepatocellular carcinoma
- Chai Hong Rim
- J Liver Cancer. 2021;21(2):113-123. Published online August 11, 2021
- DOI: https://doi.org/10.17998/jlc.2021.05.26
- 5,316 Views
- 101 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - There are differences in opinion regarding the application of external beam radiotherapy in the treatment of hepatocellular carcinoma. Some major guidelines state that external beam radiotherapy is yet to attain a sufficient level of evidence. However, caution should be exercised when attempting to understand the clinical need for external beam radiotherapy solely based on the level of evidence. Previously, external beam radiotherapy had low applicability in the treatment of hepatocellular carcinoma before computed tomography-based planning was popularized. Modern external beam radiotherapy can selectively target tumor cells while sparing normal liver tissues. Recent technologies such as stereotactic body radiotherapy have enabled more precise treatment. The characteristics of hepatocellular carcinoma differ significantly according to the regional etiology. The main cause of hepatocellular carcinoma is the hepatitis B virus. It is commonly diagnosed as a locally advanced tumor but with relatively preserved hepatic function. The majority of these hepatocellular carcinoma cases are found in the East Asian population. Hepatocellular carcinoma caused by hepatitis C virus or other benign hepatitis tends to be diagnosed as a less locally aggressive tumor but with deteriorated liver function. The Western world and Japan tend to have patients with such causes. External beam radiotherapy has been more commonly performed for the former, although the use of external beam radiotherapy in the latter might have more concerns with regard to hepatic toxicity. This review discusses the above subjects along with perspectives regarding external beam radiotherapy in recent guidelines.
-
Citations
Citations to this article as recorded by- Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma: Meta-Analysis and International Stereotactic Radiosurgery Society Practice Guidelines
Sun Hyun Bae, Seok-Joo Chun, Joo-Hyun Chung, Eunji Kim, Jin-Kyu Kang, Won Il Jang, Ji Eun Moon, Isaure Roquette, Xavier Mirabel, Tomoki Kimura, Masayuki Ueno, Ting-Shi Su, Alison C. Tree, Matthias Guckenberger, Simon S. Lo, Marta Scorsetti, Ben J. Slotman
International Journal of Radiation Oncology*Biology*Physics.2024; 118(2): 337. CrossRef - Will the collaboration of surgery and external radiotherapy open new avenues for hepatocellular carcinoma with portal vein thrombosis?
Jung Wan Choe, Hye Yoon Lee, Chai Hong Rim
World Journal of Gastroenterology.2022; 28(7): 704. CrossRef
- Stereotactic Body Radiation Therapy for Hepatocellular Carcinoma: Meta-Analysis and International Stereotactic Radiosurgery Society Practice Guidelines

Case Report
- Advanced Stage Hepatocellular Carcinoma Successfully Treated with Liver-directed Concurrent Chemoradiotherapy and Sequential Transarterial Radio-embolization
- Minho Noh, Beom Kyung Kim, Seung Up Kim
- J Liver Cancer. 2021;21(1):97-103. Published online March 31, 2021
- DOI: https://doi.org/10.17998/jlc.21.1.97

- 3,035 Views
- 73 Downloads
-
 Abstract
Abstract
 PDF
PDF - Optimal treatment strategies for patients with advanced hepatocellular carcinoma (HCC) is yet to be determined. Herein, we present a case of advanced HCC with tumor invasion into the right anterior portal vein and right hepatic vein where complete response (CR) was achieved via a multidisciplinary approach. This patient had a 10.5 cm-sized HCC invading segment VI, without extrahepatic spread. Liver function was classified as Child-Pugh class A, and the performance status was good. Transarterial radio-embolization (TARE) was performed 6 weeks after the completion of liver-directed concurrent chemoradiotherapy, and CR was confirmed 3 months post-TARE. Adoptive cell therapies were performed as adjuvant therapy and CR was maintained for over 15 months, until the local recurrence of a 2 cm-sized HCC was found. Therefore, in selected cases with preserved liver function, combination therapies, including LRTs and systemic therapy, can be a useful therapeutic option for advanced HCC.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter