Search
- Page Path
- HOME > Search
Original Articles
- Additional nodules detected using EOB-MRI in patients with resectable single hepatocellular carcinoma: an implication for active treatment strategy
- Na Reum Kim, Seoung Yoon Rho, Jonathan Navarro, Chansik An, Dai Hoon Han, Jin Sub Choi, Myeong-Jin Kim, Gi Hong Choi
- J Liver Cancer. 2024;24(1):92-101. Published online February 14, 2024
- DOI: https://doi.org/10.17998/jlc.2024.01.25
- 727 Views
- 41 Downloads
-
 Abstract
Abstract
 PDF
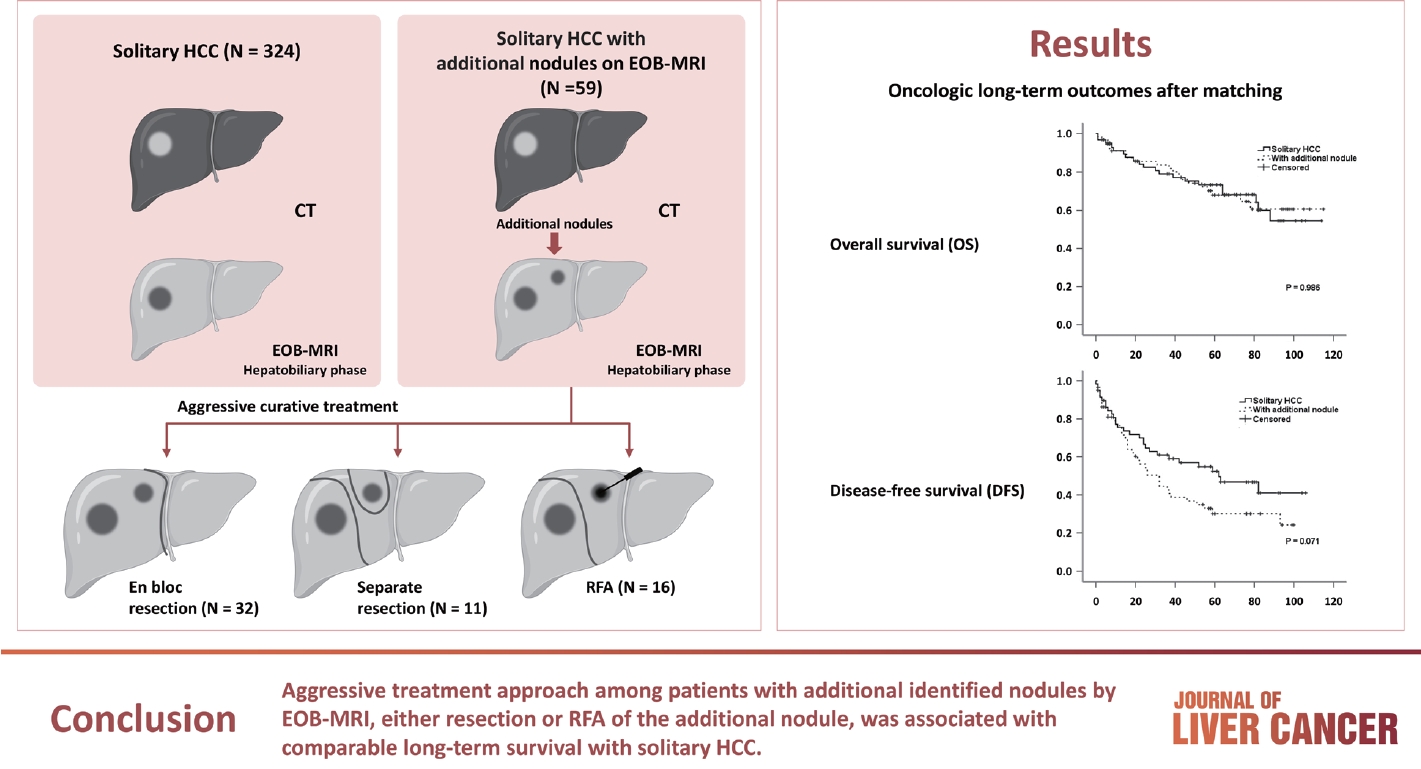
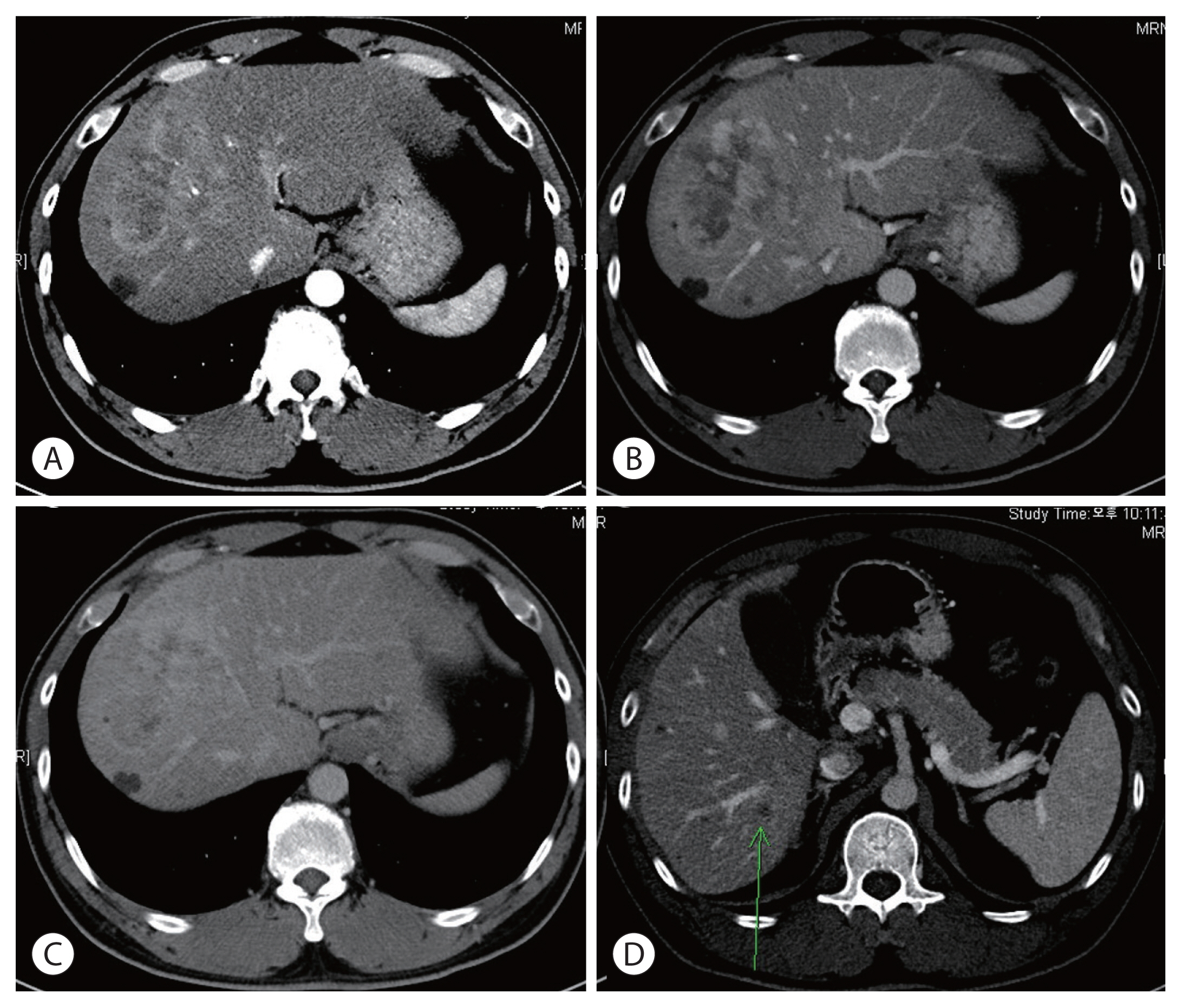
PDF - Background/Aim
Gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging (EOBMRI) further enhances the identification of additional hepatic nodules compared with computed tomography (CT) alone; however, the optimal treatment for such additional nodules remains unclear. We investigated the long-term oncological effect of aggressive treatment strategies for additional lesions identified using EOB-MRI in patients with hepatocellular carcinoma (HCC).
Methods
Data from 522 patients diagnosed with solitary HCC using CT between January 2008 and December 2012 were retrospectively reviewed. Propensity score-matched (PSM) analysis was used to compare the oncologic outcomes between patients with solitary HCC and those with additional nodules on EOB-MRI after aggressive treatment (resection or radiofrequency ablation [RFA]).
Results
Among the 383 patients included, 59 had additional nodules identified using EOB-MRI. Compared with patients with solitary HCC, those with additional nodules on EOB-MRI had elevated total bilirubin, aspartate transaminase, and alanine transaminase; had a lower platelet count, higher MELD score, and highly associated with liver cirrhosis (P<0.05). Regarding long-term outcomes, 59 patients with solitary HCC and those with additional nodules after PSM were compared. Disease-free survival (DFS) and overall survival (OS) were comparable between the two groups (DFS, 60.4 vs. 44.3 months, P=0.071; OS, 82.8 vs. 84.8 months, P=0.986).
Conclusion
The aggressive treatment approach, either resection or RFA, for patients with additional nodules identified on EOBMRI was associated with long-term survival comparable with that for solitary HCC. However, further studies are required to confirm these findings.

- Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study
- Kazuya Kariyama, Kazuhiro Nouso, Atsushi Hiraoka, Hidenori Toyoda, Toshifumi Tada, Kunihiko Tsuji, Toru Ishikawa, Takeshi Hatanaka, Ei Itobayashi, Koichi Takaguchi, Akemi Tsutsui, Atsushi Naganuma, Satoshi Yasuda, Satoru Kakizaki, Akiko Wakuta, Shohei Shiota, Masatoshi Kudo, Takashi Kumada
- J Liver Cancer. 2024;24(1):71-80. Published online November 6, 2023
- DOI: https://doi.org/10.17998/jlc.2023.09.11
- 927 Views
- 93 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
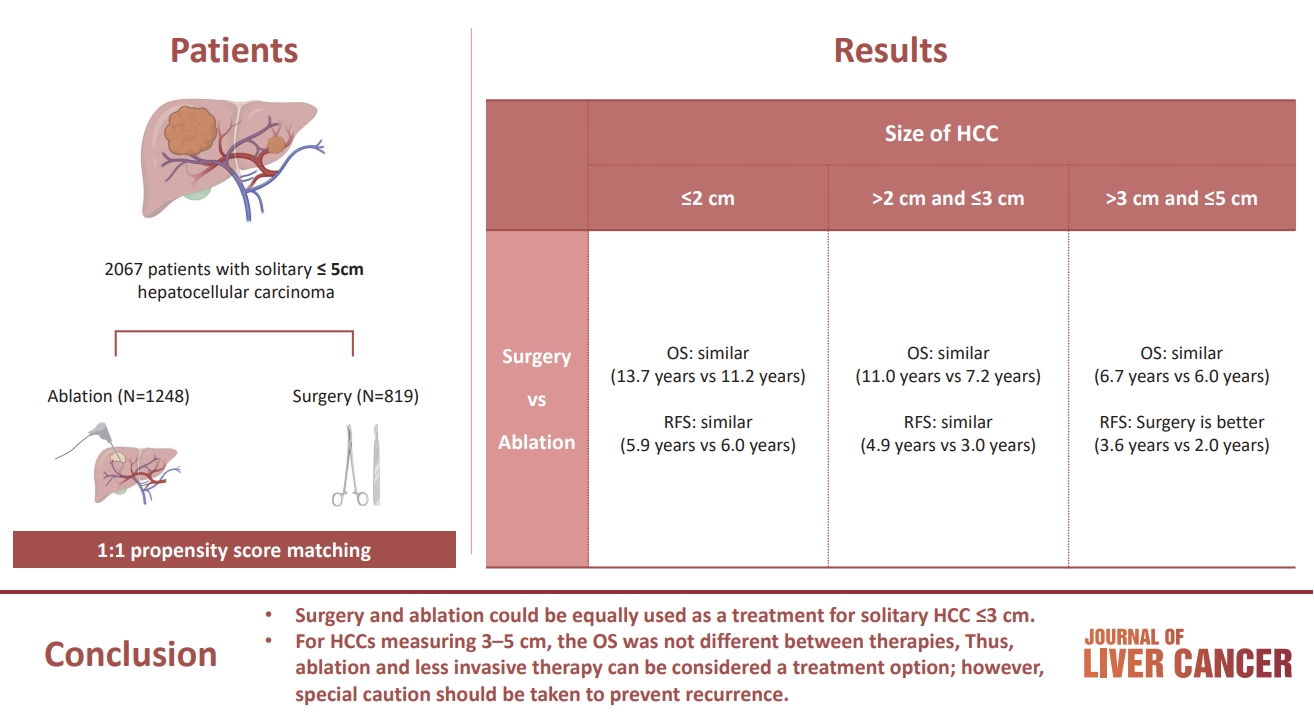
PDF - Background/Aim
The aim of this study was to compare the therapeutic efficacy of ablation and surgery in solitary hepatocellular carcinoma (HCC) measuring ≤5 cm with a large HCC cohort database.
Methods
The study included consecutive 2,067 patients with solitary HCC who were treated with either ablation (n=1,248) or surgery (n=819). Th e patients were divided into three groups based on the tumor size and compared the outcomes of the two therapies using propensity score matching.
Results
No significant difference in recurrence-free survival (RFS) or overall survival (OS) was found between surgery and ablation groups for tumors measuring ≤2 cm or >2 cm but ≤3 cm. For tumors measuring >3 cm but ≤5 cm, RFS was significantly better with surgery than with ablation (3.6 and 2.0 years, respectively, P=0.0297). However, no significant difference in OS was found between surgery and ablation in this group (6.7 and 6.0 years, respectively, P=0.668).
Conclusion
The study suggests that surgery and ablation can be equally used as a treatment for solitary HCC no more than 3 cm in diameter. For HCCs measuring 3-5 cm, the OS was not different between therapies; thus, ablation and less invasive therapy can be considered a treatment option; however, special caution should be taken to prevent recurrence. -
Citations
Citations to this article as recorded by- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
Kazuhiro Nouso, Kazuya Kariyama
Journal of Liver Cancer.2024; 24(1): 5. CrossRef - Radiofrequency for hepatocellular carcinoma larger than 3 cm: potential for applications in daily practice
Ji Hoon Kim, Pil Soo Sung
Journal of Liver Cancer.2024; 24(1): 1. CrossRef - Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
Jongman Kim
Journal of Liver Cancer.2024; 24(1): 3. CrossRef
- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”

Review Article
- Management of early-stage hepatocellular carcinoma: challenges and strategies for optimal outcomes
- Jae Hyun Yoon, Sung Kyu Choi
- J Liver Cancer. 2023;23(2):300-315. Published online September 21, 2023
- DOI: https://doi.org/10.17998/jlc.2023.08.27
- 2,164 Views
- 144 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
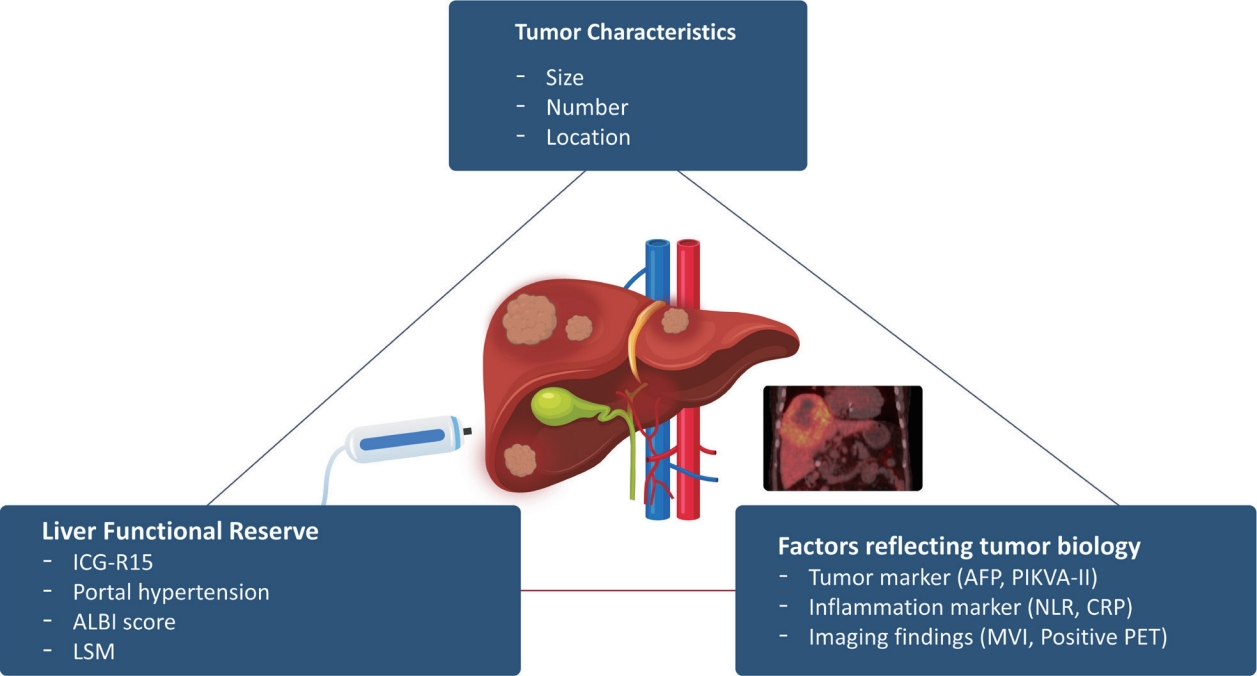
PDF - Although hepatocellular carcinoma (HCC) is associated with a poor prognosis, management of early-stage HCC is often successful with highly efficacious treatment modalities such as liver transplantation, surgical resection, and radiofrequency ablation. However, unfavorable clinical outcomes have been observed under certain circumstances, even after efficient treatment. Factors that predict unsuitable results after treatment include tumor markers, inflammatory markers, imaging findings reflecting tumor biology, specific outcome indicators for each treatment modality, liver functional reserve, and the technical feasibility of the treatment modalities. Various strategies may overcome these challenges, including the application of reinforced treatment indication criteria with predictive markers reflecting tumor biology, compensation for technical issues with up-to-date technologies, modification of treatment modalities, downstaging with locoregional therapies (such as transarterial chemotherapy or radiotherapy), and recently introduced combination immunotherapies. In this review, we discuss the challenges to achieving optimal outcomes in the management of early-stage HCC and suggest strategies to overcome these obstacles.
-
Citations
Citations to this article as recorded by- Diosgenin potentiates the anticancer effect of doxorubicin and volasertib via regulating polo-like kinase 1 and triggering apoptosis in hepatocellular carcinoma cells
Eman H. Yousef, Mohamed E. El-Mesery, Maha R. Habeeb, Laila A. Eissa
Naunyn-Schmiedeberg's Archives of Pharmacology.2024;[Epub] CrossRef - Comparison of Surgical Resection and Radiofrequency Ablation in Elderly Patients with Hepatocellular Carcinoma
Jun Il Kim, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park, Jeong-Ju Yoo
Digestive Diseases and Sciences.2024; 69(3): 1055. CrossRef - Radiofrequency for hepatocellular carcinoma larger than 3 cm: potential for applications in daily practice
Ji Hoon Kim, Pil Soo Sung
Journal of Liver Cancer.2024; 24(1): 1. CrossRef - Efficacy of Transarterial Chemoembolization (TACE) for Early-Stage Hepatocellular Carcinoma
Moonhyung Lee, Hyun Phil Shin
Medicina.2023; 59(12): 2174. CrossRef
- Diosgenin potentiates the anticancer effect of doxorubicin and volasertib via regulating polo-like kinase 1 and triggering apoptosis in hepatocellular carcinoma cells

Original Article
- Clinical outcome of surgical resection for multifocal T2-T3 hepatocellular carcinoma up to 3 nodules: a comparative analysis with a single nodule
- Sehyeon Yu, Hye-Sung Jo, Young-Dong Yu, Yoo jin Choi, Dong-Sik Kim
- J Liver Cancer. 2023;23(2):377-388. Published online September 15, 2023
- DOI: https://doi.org/10.17998/jlc.2023.08.24

- 631 Views
- 35 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
s: Although the Barcelona Clinic Liver Cancer staging system seems to underestimate the impact of curative-intent surgical resection for multifocal hepatocellular carcinoma (HCC), recent studies have indicated favorable results for the surgical resection of multiple HCC. This study aimed to assess clinical outcomes and feasibility of surgical resection for multifocal HCC with up to three nodules compared with single tumor cases.
Methods
Patients who underwent surgical resection for HCC with up to three nodules between 2009 and 2020 were included, and those with the American Joint Committee on Cancer (AJCC) 8th edition, T1 and T4 stages were excluded to reduce differences in disease distribution and severity. Finally, 81 and 52 patients were included in the single and multiple treatment groups, respectively. Short- and long-term outcomes including recurrence-free survival (RFS) and overall survival (OS), were evaluated.
Results
All patients were classified as Child-Pugh class A. RFS and OS were not significantly different between the two groups (P=0.176 and P=0.966, respectively). Multivariate analysis revealed that transfusion and intrahepatic metastasis were significantly associated with recurrence (P=0.046 and P=0.005, respectively). Additionally, intrahepatic metastasis was significantly associated with OS (hazard ratio, 1.989; 95% confidence interval, 1.040-3.802; P=0.038).
Conclusions
Since there was no significant difference in survival between the single and multiple groups among patients with AJCC 8th stage T2 and T3, surgical resection with curative intent could be considered with acceptable long-term survival for selected patients with multiple HCC of up to three nodules.

Case Reports
- Parenchymal-sparing hepatectomy for multiple bilobar colorectal liver metastases in a Jehovah’s witness: a case report
- Shehan Ratnayake, Duminda Subasinghe, Vihara Dassanayake, Sivasuriya Sivaganesh
- J Liver Cancer. 2023;23(1):202-205. Published online February 15, 2023
- DOI: https://doi.org/10.17998/jlc.2023.01.27
- 1,472 Views
- 68 Downloads
-
 Abstract
Abstract
 PDF
PDF - Parenchymal-sparing hepatectomy (PSH), though technically challenging, is emerging as a choice of treatment for colorectal liver metastases (CRLM). PSH in Jehovah’s witness (JW) patients, for whom transfusion is not an option, involves complex surgical and medicolegal issues. A 52-year-old JW male with synchronous, multiple, bilobar liver metastases from a rectal adenocarcinoma was referred following neoadjuvant chemotherapy. At surgery, 10 metastatic deposits were observed and confirmed by intraoperative ultrasonography. Parenchymal-sparing non-anatomical resections were performed using a cavitron ultrasonic aspirator with the application of intermittent Pringle maneuvres. Histology confirmed multiple CRLMs with tumor-free resection margins. PSH is increasingly employed for CRLMs to preserve residual liver volume and minimize morbidity without compromising oncological outcomes. It is technically challenging, especially in the presence of bilobar, multi-segmental disease. This case illustrates the feasibility of performing complex hepatic surgery in special patient groups by meticulous planning and preparation involving multiple specialties and the patient.

- Long-term survival after CCRT and HAIC followed by ALPPS for hepatocellular carcinoma with portal vein invasion: a case report
- In-Jung Kim, Sung Hwan Yoo, Jung Il Lee, Kwan Sik Lee, Hyun Woong Lee, Jin Hong Lim
- J Liver Cancer. 2022;22(1):84-90. Published online March 22, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.07
- 2,786 Views
- 70 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - There are various methods for treating advanced hepatocellular carcinoma with portal vein invasion, such as systemic chemotherapy, transarterial chemoembolization, transarterial radioembolization, and concurrent chemoradiotherapy. These methods have similar clinical efficacy but are designed with a palliative aim. Herein, we report a case that experienced complete remission through “associating liver partition and portal vein ligation for staged hepatectomy (ALPPS)” after concurrent chemoradiotherapy and hepatic artery infusion chemotherapy. In this patient, concurrent chemoradiotherapy and hepatic artery infusion chemotherapy induced substantial tumor shrinkage, and hypertrophy of the nontumor liver was sufficiently induced by portal vein ligation (stage 1 surgery) followed by curative resection (stage 2 surgery). Using this approach, long-term survival with no evidence of recurrence was achieved at 16 months. Therefore, the optimal use of ALPPS requires sufficient consideration in cases of significant hepatocellular carcinoma shrinkage for curative purposes.
-
Citations
Citations to this article as recorded by- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?

- Two Cases of Early Recurred Hepatocellular Carcinoma after Surgical Resection Which Showed Different Outcomes
- Young Youn Cho, Jeong-Hoon Lee, Nam Joon Yi, Kwang Woong Lee, Kyung Suk Suh, Yoon Joon Kim, Jung-Hwna Yoon
- J Liver Cancer. 2015;15(2):126-131. Published online September 30, 2015
- DOI: https://doi.org/10.17998/jlc.15.2.126
- 784 Views
- 6 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) has poor prognosis, even after curative resection. Early
recurrence after curative treatment is a major cause of the poor prognosis. Pathologic factors
such as vessel invasion, satellite nodule, size of tumor and pathologic grade are prognostic
factors predicting early recurrence and poor prognosis. We share our experience of two
case
s which both showed early recurrence after curative hepatic resection, but eventually demonstrated different prognosis. Since the most common cause of death after potentially curative treatment is tumor recurrence, suppression of tumor recurrence might be linked to survival gain. Currently, there is no adjuvant therapy for HCC endorsed by international guidelines. However, recent studies have shown that antiviral treatment for hepatitis B virusrelated HCC and immunotherapy using autologous cytokine-induced killer cell reduced HCC recurrence. Further study is needed to select patients who will benefit from adjuvant treatments.

- A Case of Hepatocellular Carcinoma with Portal Vein Tumor Thrombi which was Performed Hepatectomy after Down-staging by Proton Therapy
- Hee-Jung Wang, Bong-Wan Kim, Wei-Kwang Xu
- Journal of the Korean Liver Cancer Study Group. 2011;11(1):56-59. Published online February 28, 2011
- 600 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - A case of hepatocellular carcinoma (HCC) with portal vein tumor thrombi (PVTT) which was performed hepatectomy after down-staging by proton therapy is reviewed. Generally, the recommended therapeutic strategy for this kind of HCC is radiation therapy, systemic or infusion anticancer chemotherapy. However, the response of HCC and its PVTT of this 56 year-old male patient was relatively good after 22 times of proton therapy, and we performed right hemihepatectomy on the concept of clinical trial under the informed consent of patient and his families. He is still alive without recurrence 15 months after hepatectomy. We suggest that hemihepatectomy with removal of PVTT could be an alternative strategy in the PVTT accompanied HCC cases who show good responses after the above generally recommended therapies.

- A Case of Hepatocellular Carcinoma Presenting Early Intrahepatic Recurrence Following Hepatic Resection
- Jaejun Shim, Byung-Ho Kim, Young Hwangbo, Sang Wook Lee, Young Ju Lee, Seung Hyung Ha, Jae Young Jang, Seok Ho Dong, Hyo Jong Kim, Young Woon Chang, Rin Chang, Sang Mok Lee
- Journal of the Korean Liver Cancer Study Group. 2009;9(1):33-36. Published online June 30, 2009
- 504 Views
- 0 Download
-
 Abstract
Abstract
 PDF
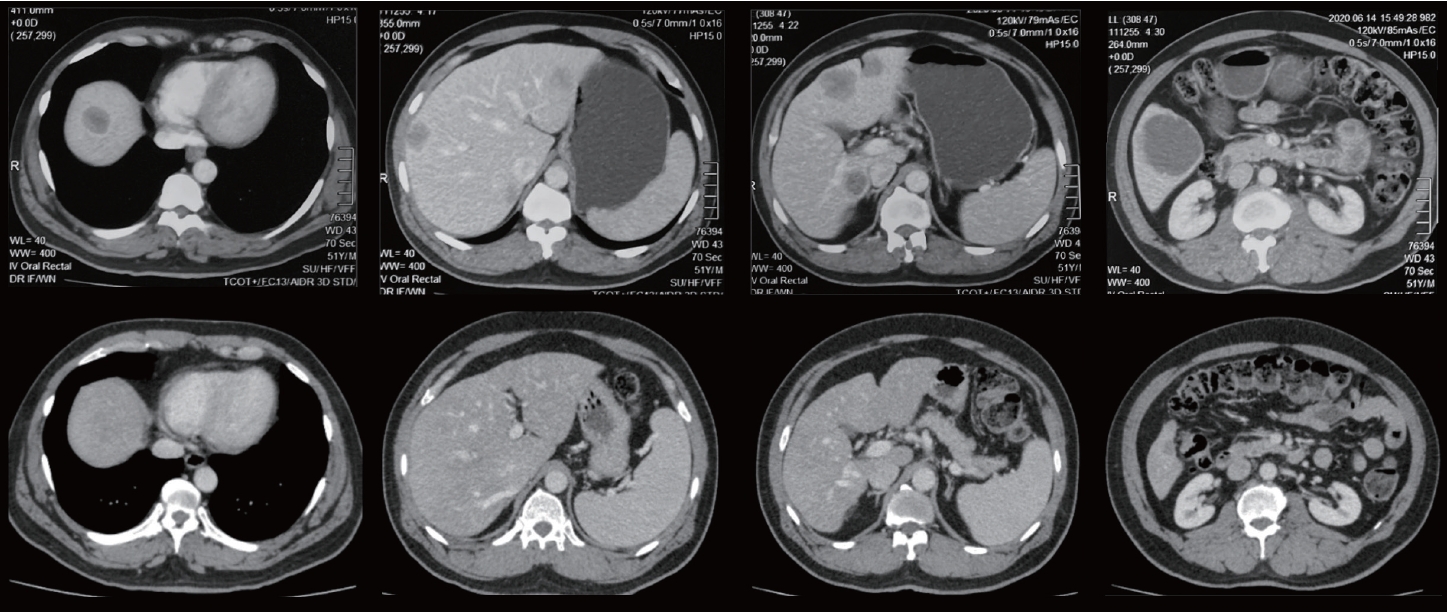
PDF - Long term results of hepatic resection for hepatocellular carcinoma (HCC) are not satisfactory due to a high incidence of postoperative recurrence. To improve the prognosis in patients who underwent hepatic resection, identification of risk factors for recurrence and development of effective preventive strategies are required. A single nodular mass was found in the right hepatic lobe of 53-year old male with B viral cirrhosis by surveillance ultrasonography. Dynamic abdominal CT showed a 3 cm-sized hypervascular mass in the right posteroinferior segment (S6). AFP was 359 ng/mL. Child-Pugh classification was A, and ICG R15 was 18.8%. After preoperative transarterial chemoembolization (TACE), right hepatic wedge resection was performed. Resection margin was free of tumor. Microinvasions in the surrounding vessels, lymphatics, bile ducts were not found and microsatellite nodules were absent in the resected specimen. Although there were no risk factors that associated with high postoperative recurrence, multifocal intrahepatic recurrence in the right lobe and left medial lobe occurred at 7 months after hepatic resection. He underwent two sessions of TACE.

Review Article
- Current Experience of Metastasectomy of HCC - When and for Whom?
- Sang Jae Park
- Journal of the Korean Liver Cancer Study Group. 2008;8(1):8-11. Published online June 30, 2008
- 503 Views
- 8 Downloads
-
 Abstract
Abstract
 PDF
PDF - Intrahepatic (IH) metastasis is more frequent but extrahepatic (EH) metastasis results in worse prognosis and proper treatment on IH and EH metastasis is essential for improving the long-term survival. The purpose of this report is to review the current experience of EH metastasectomy and also to review the results of re-hepatectomy on IH metastasis after hepatectomy of HCC. EH metastasis can occur in lung, lymph nodes, bone, adrenal gland and brain in frequency. Indications of EH metastatectomy of HCC are 1) cured or controlled IH lesion, 2) acceptable operation risk, 3) complete removal of EH lesions seems possible. After lung metastasectomy, 5-year survival rates in previous reports are 23-67% according to the indications. The poor prognosis factors after lung metastasectomy are short disease-free interval between hepatectomy and lung resection, high alpha-fetoprotein. In selected patients with EH metastasis of HCC, long-term survival can be achieved by proper and aggressive surgery. The 5-year recurrence rate after hepatectomy of HCC ranges 60-100% and more than half of them is IH recurrence. IH recurrence can be classified to IH metastasis and multicentric occurrence (MO) by mode of recurrence, and MO is known to be related to HCV infection, long disease-free interval and better survival. Though it is impossible to discriminate IH metastasis and MO, re-hepatectomy should be considered in patients with single nodule recurrence and with more than 1-year of disease-free survival after hepatectomy of HCC.

Case Report
- Poorly Differentiated Hepatocellular Carcinoma with Intraluminal Metastasis to the Bile Duct
- Jae Gil Lee, Yong Il Kim, Soon Hee Sung
- Journal of the Korean Liver Cancer Study Group. 2008;8(1):64-68. Published online June 30, 2008
- 460 Views
- 0 Download
-
 Abstract
Abstract
 PDF
PDF - Stem cells of the liver are differentiated to both hepatocytes and cholangiole. So bidirectional malignant transformation may be occurred. Hepatocellular carcinoma with bile-duct tumor thrombi is clinically rare and cause the obstructive jaundice. We experienced the poorly differentiated hepatocellular carcinoma showed the bidirectional differentiation. And she had metastatic foci in right intrahepatic duct with tumor thrombi to the common bile duct. A 72-year-old female patient was admitted to hospital by pruritus, general weakness and dark urine for 15 days. She was diagnosed liver cirrhosis due to chronic HBV 15 years ago. She showed icteric sclerae. The laboratory findings were followed; total bilirubin/direct bilirubin was 9.7/7.3 mg/dL, SGOT/SGPT was 59/115 IU/L, alkaline phosphatase 681 IU/L, alpha-fetoprotein was 16.9 ng/mL and CA19-9 was 76.2 U/mL. ICG-R15 was 11.8%. The hilar cholangiocarcinoma type IIIa with liver abscess was diagnosed by CT scan and MRI scan. She underwent Rt. hepatectomy with resection of CBD, Roux-en-Y hepaticojejunostomy. After pathologic examination, the poorly differentiated hepatacellular carcinoma with bile duct metastasis was confirmed. Metastasis to right lower lung was detected at 1 years after 1st operation. So, she underwent wedge resection of RLL. She remains without any problems 6 months after 2nd operation.

Review Articles
- How to Prevent Post Operative Hepatic Failure after Hepatic Resection
- Jinsub Choi
- Journal of the Korean Liver Cancer Study Group. 2005;5(1):7-11. Published online June 30, 2005
- 489 Views
- 1 Download

- Interventional Management of Recurrent Hepatocellular Carcinomas after Hepatomy
- Dong Il Choi
- Journal of the Korean Liver Cancer Study Group. 2003;3(1):10-20. Published online July 31, 2003
- 813 Views
- 0 Download

Case Reports
- A Case of Percutaneous Radiofrequency Ablation of Recurrent Hepatocellular Carcinomas after Hepatectomy
- Min Ju Kim, Dong Il Choi, Hyo Keun Lim, Won Jae Lee
- Journal of the Korean Liver Cancer Study Group. 2003;3(1):48-52. Published online July 31, 2003
- 496 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - A 43-year-old man who had hepatic segmentectomy due to hepatocellular carcinoma was found to have a recurrent hepatocelllular carcinoma in the remnant liver along the resection margin. The patient has been performed radiofrequency ablation three times for recurrent hepatocellular carcinomas through 27 months after initial hepatectomy. We report a case of recurrent hepatocellular carcinomas after hepatectomy that were susccessfully treated radiofrequency ablation.

- Sarcomatoid Hepatocellular Carcinoma
- Jin Sub Choi, Kyung Sik Kim, Yong Nyun Park, Woo Jung Lee, Jae Yoon Chon, Jong Tae Lee, Byong Ro Kim
- Journal of the Korean Liver Cancer Study Group. 2002;2(1):76-79. Published online July 31, 2002
- 589 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - A 64-year-old male was admitted due to liver mass. He had radical prostatectomy owing to prostate cancer 5 years ago. At that time, the liver mass was found on the right posterior superior segment and had enlarged to 7 cm in diameter at Nov. 2001. The transhepatic chemoembolization with adriamycin 50 mg and gelform was performed but the viable portions of tumor were remained. Total bilirubin was 0.7 mg/dL, Albumin 2.9 g/dL, AST/ALT 24/18 IU/L and AFP 60.31 ng/mL. The ICG R15 was 6.2%. The right lobectomy of liver was done and the pathologic results were sarcomatoid hepatocellular carcinoma. The level of AFP was decreased 2 month after operation but the patient was dead 4 month after operation because of the metastasis to the right psoas muscle and suspected peritoneal seeding.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter