Search
- Page Path
- HOME > Search
Original Article
- Subclassification of advanced-stage hepatocellular carcinoma with macrovascular invasion: combined transarterial chemoembolization and radiotherapy as an alternative first-line treatment
- Sujin Jin, Won-Mook Choi, Ju Hyun Shim, Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jinhong Jung, Sang Min Yoon, Jonggi Choi
- J Liver Cancer. 2023;23(1):177-188. Published online March 23, 2023
- DOI: https://doi.org/10.17998/jlc.2023.03.04

- 1,921 Views
- 96 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
The Barcelona Clinic Liver Cancer (BCLC) guidelines recommend systemic therapy as the only first-line treatment for patients with BCLC stage C hepatocellular carcinoma (HCC) despite its heterogeneity of disease extent. We aimed to identify patients who might benefit from combined transarterial chemoembolization (TACE) and radiation therapy (RT) by subclassifying BCLC stage C.
Methods
A total of 1,419 treatment-naïve BCLC stage C patients with macrovascular invasion (MVI) who were treated with combined TACE and RT (n=1,115) or systemic treatment (n=304) were analyzed. The primary outcome was overall survival (OS). Factors associated with OS were identified and assigned points by the Cox model. The patients were subclassified into three groups based on these points.
Results
The mean age was 55.4 years, and 87.8% were male. The median OS was 8.3 months. Multivariate analysis revealed a significant association of Child-Pugh B, infiltrative-type tumor or tumor size ≥10 cm, main or bilateral portal vein invasion, and extrahepatic metastasis with poor OS. The sub-classification was categorized into low (point ≤1), intermediate (point=2), and high (point ≥3) risks based on the sum of points (range, 0–4). The OS in the low, intermediate, and high-risk groups was 22.6, 8.2, and 3.8 months, respectively. In the low and intermediate-risk groups, patients treated with combined TACE and RT exhibited significantly longer OS (24.2 and 9.5 months, respectively) than those who received systemic treatment (6.4 and 5.1 months, respectively; P<0.0001).
Conclusions
Combined TACE and RT may be considered as a first-line treatment option for HCC patients with MVI when classified into low- and intermediate-risk groups. -
Citations
Citations to this article as recorded by- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
Journal of Liver Cancer.2024; 24(1): 102. CrossRef - Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
Journal of Liver Cancer.2024; 24(1): 81. CrossRef - How to optimize the treatment strategy for advanced-stage hepatocellular carcinoma with macrovascular invasion
Beom Kyung Kim
Journal of Liver Cancer.2023; 23(1): 121. CrossRef
- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis

Case Report
- A Case of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis Treated by Hepatic Arterial Infusion Chemotherapy and Radiotherapy
- Jin Yong Lee, Jeong-Ju Yoo, Seong Joon Chun, Sun Hyun Bae, Jae Myeong Lee, Sang Gyune Kim, Young Seok Kim
- J Liver Cancer. 2020;20(1):78-83. Published online March 31, 2020
- DOI: https://doi.org/10.17998/jlc.20.1.78
- 5,079 Views
- 99 Downloads
-
 Abstract
Abstract
 PDF
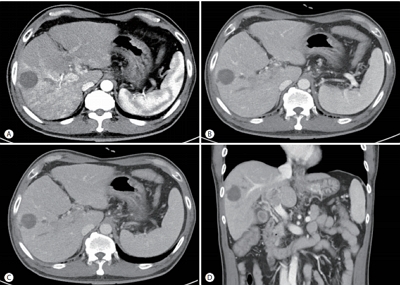
PDF - Sorafenib is the standard treatment for advanced hepatocellular carcinoma (HCC) with portal vein thrombosis (PVT). Additionally, hepatic arterial infusion chemotherapy has been used as a treatment option for advanced HCC. Here, we report a case of sustained partial response in a patient with advanced HCC with PVT after hepatic arterial infusion chemotherapy and radiation therapy.

Original Articles
- An Analysis for Survival Predictors for Patients with Hepatocellular Carcinoma Who Failed to Sorafenib Treatment in Pre-regorafenib Era
- Chan Uk Lee, Young-Sun Lee, Ji Hoon Kim, Minjin Lee, Sehwa Kim, Young Kul Jung, Yeon Seok Seo, Hyung Joon Yim, Jong Eun Yeon, Kwan Soo Byun
- J Liver Cancer. 2019;19(2):117-127. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.117

- 4,432 Views
- 67 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
Sorafenib is the standard treatment for patients with advanced hepatocellular carcinoma (HCC). We aimed to investigate the prognosis predictors and the role of second-line cytotoxic systemic chemotherapy (CSC) in patients with advanced HCC after sorafenib discontinuation in the pre-regorafenib era.
Methods
From 2007 to 2015 in the pre-regorafenib era, the medical records of 166 HCC patients, who had permanently discontinued sorafenib, were retrospectively reviewed. For further analysis of survival factors after sorafenib treatment failure, we compared the survival of patients who had maintained liver function after second-line treatment with the best supportive care (BSC) group and selective BSC (SBSC) group.
Results
After discontinuation of sorafenib, median overall survival (OS) was 2.8 (1.9-3.7) months. The OS in patients who discontinued sorafenib due to adverse effect, progression, and poor clinical condition were 5.5 (2.4-8.6), 5.5 (2.2-8.9), and 0.9 (0.5-1.3) months, respectively (P<0.001). The independent predictive factors of survival after sorafenib failure were serum level of bilirubin and albumin, α-fetoprotein, discontinuation cause, and second-line CSC. In comparison with survival between second-line CSC and BSC group, the CSC group showed better survival outcome compared to the BSC group (10.6 vs. 1.6 months, P<0.001) and SBSC group (10.6 vs. 4.2 months, P=0.023).
Conclusions
The survival after sorafenib failure in patients who discontinued sorafenib due to progression and adverse effects was significantly better than in those who discontinued treatment due to clinical deterioration. In the pre-regorafenib era, patients who received second-line CSC showed better survival than those who received only supportive care after sorafenib failure.

- High-dose versus Low-dose 5-Fluorouracil and Cisplatin Based Hepatic Arterial Infusion Chemotherapy for Advanced Hepatocellular Carcinoma
- Chae-June Lim, Ji-Yun Hong, Yang-Seok Ko, Min-Woo Chung, Chung-Hwan Jun, Sung-Kyu Choi, Sung-Bum Cho
- J Liver Cancer. 2019;19(1):38-45. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.38
- 4,696 Views
- 176 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Backgrounds/Aims
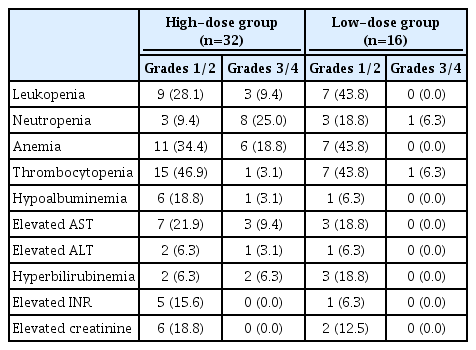
Hepatic arterial infusion chemotherapy (HAIC) has been reported as an effective treatment for advanced hepatocellular carcinoma. The aim of this study is to compare the effect and safety between a high-dose regimen (750 mg/m2 5-fluorouracil [FU] and 25 mg/m2 cisplatin on day 1-4) and a low-dose regimen (500 mg/m2 5-FU on day 1-3 with 60 mg/m2 cisplatin on day 2).
Methods
A total of 48 patients undergoing HAIC were retrospectively analyzed. Thirty-two patients were treated with the high-dose and 16 patients with the low-dose regimen.
Results
Complete response (CR), partial response (PR), stable disease (SD), and progressive disease were noted in one (3.1%), 15 (46.9%), three (9.4%), and 13 patients (40.6%) in the highdose group, and 0 (0%), one (6.3%), eight (50%), and seven patients (43.8%) in the low-dose group (p=0.002). The disease control rate (CR, PR, and SD) did not differ between groups (59.4% vs. 56.3%, p=1.000), but the objective response rate (CR and PR) was significantly higher in the high-dose group (50.0% vs. 6.3%, p=0.003). The median progression free survival did not differ between groups (4.0 vs. 6.0, p=0.734), but overall survival was significantly longer in the high-dose group (not reached vs. 16.0, p=0.028). Fourteen (43.8%) patients in the highdose group and two patients (12.5%) in the low-dose group experienced grade 3-4 toxicities (p=0.050).
Conclusions
High dose HAIC may achieve better tumor response and may improve overall survival compared to a low-dose regimen. However, the high-dose regimen should be administered cautiously because of the higher incidence of adverse events. -
Citations
Citations to this article as recorded by- A programmed cell death-related gene signature to predict prognosis and therapeutic responses in liver hepatocellular carcinoma
Xinyu Gu, Jie Pan, Yanle Li, Liushun Feng
Discover Oncology.2024;[Epub] CrossRef - Development of a novel chromatographic method for concurrent determination of 5-fluorouracil and cisplatin: Validation, greenness evaluation, and application on drug-eluting film
Souha H. Youssef, Franklin Afinjuomo, Yunmei Song, Sanjay Garg
Microchemical Journal.2021; 168: 106510. CrossRef
- A programmed cell death-related gene signature to predict prognosis and therapeutic responses in liver hepatocellular carcinoma

Case Reports
- A Case of Complete Response with Biliary Stenosis after Hepatic Arterial Injection and Stereotactic Body Radiotherapy to Hepatoecllular Carcinoma with Portal Vein Thrombosis
- Rim, Chai Hong , Im, Hyung Joon , Jung, Young Geol , Chung, Hwan Hoon , Seo, Sang Joon , Yoon, Won Sup
- J Liver Cancer. 2018;18(1):75-79. Published online March 31, 2018
- DOI: https://doi.org/10.17998/jlc.18.1.75
- 2,090 Views
- 40 Downloads
-
 Abstract
Abstract
 PDF
PDF - Curative treatment of hepatocellular carcinoma (HCC) with portal vein invasion is difficult to achieve, and the prognosis is dismal. Combining external beam radiotherapy (EBRT) with hepatic arterial infusion chemotherapy (HAIC) has shown favorable local therapeutic effects for patients with HCC exhibiting portal vein invasion. Stereotactic body radiotherapy (SBRT) is a recently developed EBRT modality that shows excellent tumor control. The combination of SBRT and HAIC for HCC with portal vein invasion has not been well-studied. We report a patient with HCC and portal vein invasion who achieved 15 months of survival with complete response status after combination SBRT and HAIC. The patient later experienced grade 3 biliary stricture and died of liver abscesses of unknown etiologies that subsequently appeared.

- A Case of Hepatocellular Carcinoma with Pulmonary Metastasis Who Showed Complete Response by Cytotoxic Chemotherapy after Sorafenib Failure
- Hwa-Sun Park, Jae Young Jang, Min Young Baek, Yong Kwon Kim, Hyun Jin Youn, Su Young Back, Soung Won Jeong, Sae Hwan Lee, Sang Gyune Kim, Sang Woo Cha, Young Seok Kim, Young Deok Cho, Hong Soo Kim, Boo Sung Kim
- J Liver Cancer. 2017;17(1):72-76. Published online March 31, 2017
- DOI: https://doi.org/10.17998/jlc.17.1.72
- 2,224 Views
- 26 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is the 2nd most common cause of cancer related death in Korea and well-known malignancy with poor prognosis. Sorafenib is the first-line molecular targeted agent in patients with extra-hepatic spread of HCC. However, complete response is extremely rare in patients treated with sorafenib and the disease control rate is only 43%. We report a 53-year-old man with advanced HCC with pulmonary metastasis who showed complete response by cytotoxic chemotherapy with doxorubicin and cisplatin with relatively tolerable adverse effects after failure of treatment with sorafenib.

- A Case of Management for Hepatocellular Carcinoma with Lung Metastasis
- Han Jo Jeon, Tae Hyung Kim, Soon Ho Um, Yeon Seok Seo, Hyun Seo Kim, Ki Joon Lim, Seung Woon Park, Han Ah Lee, Dong-Sik Kim
- J Liver Cancer. 2016;16(2):129-133. Published online September 30, 2016
- DOI: https://doi.org/10.17998/jlc.16.2.129
- 1,165 Views
- 17 Downloads
-
 Abstract
Abstract
 PDF
PDF - Liver cancer is the 2nd most common cause of cancer related death in Korea. Especially, patients who present extrahepatic spread of hepatocellular carcinoma (HCC) have a shorter life expectancy (50% survival at 1 year and less than 4 months of median overall survival). Molecular target agent like sorafenib was usually mentioned as a treatment for them, but that was still not firmly established. We present a 75 year-old who had expanding nodular type of HCC. The mass was removed by resection and radiofrequency ablation. However, lung metastasis were revealed shortly after surgery. That lesions were treated with lenvatinib and systemic chemotherapy.

- A Case of Complete Remission in Patient with Extrahepatic Metastasis after Curative Resection of Hepatocellular Carcinoma by Radiotherapy, Lung Resection and Systemic Chemotherapy
- Yeong Jin Kim, Hye won Lee, Ji Hoon Lee, Jin Sil Sung, Do Young Kim
- J Liver Cancer. 2016;16(1):63-66. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.63
- 991 Views
- 8 Downloads
-
 Abstract
Abstract
 PDF
PDF - Surgical resection is mainstay treatment of hepatocellular carcinoma (HCC). However, its prognosis is poor, because of the high incidence of HCC recurrence (cumulative 5-year HCC recurrence rate of 70-80%). The most common site of HCC recurrence is the remnant liver, and extrahepatic recurrence occurs in 6.7-13.5% of patients. Because the tumor characteristics in extrahepatic recurrence are usually multiple and aggressive, the optimal treatment modality has not yet been determined. We report a case of complete remission and long term survival over 60 months in patient with extrahepatic metastasis after curative resection of HCC by aggressive treatment, which include lung resection for lung metastasis, radiotherapy for mediastinal lymph node metastasis, and systemic chemotherapy.

Review Article
- Treatments Other than Sorafenib for Patients with Advanced Hepatocellular Carcinoma
- Do Seon Song, Si Hyun Bae
- J Liver Cancer. 2016;16(1):1-6. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.1
- 1,249 Views
- 19 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Sorafenib is the standard treatment for advanced hepatocellular carcinoma according to the Barcelona Clinic Liver Cancer staging system. However, because of its unsatisfactory efficacy, adverse effects, and high cost, the use of sorafenib is limited, and other treatment modalities are required. Recent studies reported that treatment modalities other than sorafenib, such as hepatic arterial infusion chemotherapy and transarterial radioembolization, showed comparable or better response rates and survival rates than sorafenib. In this review, treatment modalities that could be used as alternatives to sorafenib will be discussed. (J Liver Cancer 2016;16:1-6)
-
Citations
Citations to this article as recorded by- Phase I Radiation Dose-Escalation Study to Investigate the Dose-Limiting Toxicity of Concurrent Intra-Arterial Chemotherapy for Unresectable Hepatocellular Carcinoma
Yeona Cho, Jun Won Kim, Ja Kyung Kim, Kwan Sik Lee, Jung Il Lee, Hyun Woong Lee, Kwang-Hun Lee, Seung-Moon Joo, Jin Hong Lim, Ik Jae Lee
Cancers.2020; 12(6): 1612. CrossRef
- Phase I Radiation Dose-Escalation Study to Investigate the Dose-Limiting Toxicity of Concurrent Intra-Arterial Chemotherapy for Unresectable Hepatocellular Carcinoma

Original Article
- Comparative Study between Metronomic Chemotherapy and Transarterial Chemoembolization in Patients with Child-Pugh Class B Advanced Hepatocellular Carcinoma
- Hyun Yang, Myeong Jun Song, Hee Chul Nam, Hae Lim Lee, Sung Won Lee, Do Seon Song, Jeong Won Jang, Si Hyun Bae, Jong Yong Choi, Seung Kew Yoon
- J Liver Cancer. 2015;15(2):92-99. Published online September 30, 2015
- DOI: https://doi.org/10.17998/jlc.15.2.92
- 1,398 Views
- 9 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
Metronomic (MET) chemotherapy is a treatment characterized by frequent infusion of low doses of chemotherapeutic agent without extended break. The aim of this study is to evaluate the efficacy of MET chemotherapy compared with transarterial chemoembolization (TACE) in patients with child B class advanced hepatocellular carcinoma (HCC).
Methods
Seventy-three patients with child B class advanced HCC were analyzed between April, 2007 and August, 2013 according to two treatment groups: (i) MET chemotherapy group (n=43, Epirubicin 35 mg/body surface area [BSA] every 4 weeks, and cisplatin 15 mg/BSA and 5-fluorouracil 50 mg/BSA weekly for 3 weeks) via an implantable port system with 1 week break. (ii) TACE group (n=30, Adriamycin 20-50 mg) every 4 weeks. Primary endpoint was overall survival (OS).
Results
The median survival times in the MET and TACE groups were 4.5 months and 3.1 months, respectively. The overall survival rate showed significantly better in the MET treatment group than in the TACE group (P=0.039). When the factors affecting patient OS were analyzed, MET chemotherapy (P=0.038, hazard ratio {HR} 0.538 [95% confidence interval {CI} 0.299-0.967]) was independently associated with OS. Larger maximal tumor size, extrahepatic metastasis and advanced stage also were significant factors for OS (P=0.009, HR 1.064 [95% CI 1.014-16.064]; P=0.014, HR 2.120 [95% CI 1.164-3.861]; P=0.019, HR 2.046 [95% CI 1.125-3.720], respectively).
Conclusions
MET chemotherapy showed survival benefit than TACE in patients with child class B advanced HCC. Therefore, MET chemotherapy may be considered as a treatment option for advanced HCC with poor liver function. (J Liver Cancer 2015;15:92-99) -
Citations
Citations to this article as recorded by- A comparative study of sorafenib and metronomic chemotherapy for Barcelona Clinic Liver Cancer-stage C hepatocellular carcinoma with poor liver function
Hyun Yang, Hyun Young Woo, Soon Kyu Lee, Ji Won Han, Bohyun Jang, Hee Chul Nam, Hae Lim Lee, Sung Won Lee, Do Seon Song, Myeong Jun Song, Jung Suk Oh, Ho Jong Chun, Jeong Won Jang, Angelo Lozada, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon
Clinical and Molecular Hepatology.2017; 23(2): 128. CrossRef
- A comparative study of sorafenib and metronomic chemotherapy for Barcelona Clinic Liver Cancer-stage C hepatocellular carcinoma with poor liver function

Case Report
- A Case of Partial Response of Hepatocellular Carcinoma Induced by Concurrent Chemoradiation and Hepatic Arterial Infusion Chemotherapy after Trans-Arterial Chemoembolization
- Myung Eun Song, Sangheun Lee, Mi Na Kim, Dong-Jun Lee, Beom Kyung Kim, Seung Up Kim, Jun Yong Park, Sang Hoon Ahn, Chae Yoon Chon, Kwang-Hyub Han, Jinsil Seong, Do Young Kim
- Journal of the Korean Liver Cancer Study Group. 2013;13(2):152-157. Published online September 30, 2013
- DOI: https://doi.org/10.17998/jlc.13.2.152
- 1,003 Views
- 7 Downloads
-
 Abstract
Abstract
 PDF
PDF - A 63-year-old man patient was referred for treatment of infiltrative hepatocellular carcinoma with hilar invasion after transarterial chemoembolization. Serum alkaline phosphatase and bilirubin were elevated, liver dynamic CT showed infiltrative type mass in left hepatic lobe and right hepatic dome with hilar invasion and left intrahepatic duct dilatation. Also CT showed obliteration of left portal vein and metastasis of lymph node around common bile duct. He was diagnosed as hepatocellular carcinoma (UICC stage IV-A, BCLC stage C). With the percutaneous transhepatic biliary drainage and the concurrent chemoradiation therapy and the 4th cycle of hepatic arterial infusion chemotherapy for infiltrative mass, viable tumor was decreased in resectable size at eight months from initial diagnosis.

Review Articles
- Systemic Cytotoxic Therapy in Advanced HCC
- Seung Tae Kim, Yeul Hong Kim
- Journal of the Korean Liver Cancer Study Group. 2013;13(1):18-21. Published online February 28, 2013
- DOI: https://doi.org/10.17998/jlc.13.1.18
- 1,241 Views
- 6 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is an aggressive tumor that occurs in chronic liver disease and cirrhosis. Surgical therapy including transplantation or local ablation may offer the prospect of cure. However, most patients were diagnosed with unresectable, advanced disease. For these patients, providing liver function and performance status permit, systemic therapies are often used with palliative intent. Although recently molecular targeted therapies have been employed with some success, cytotoxic chemotherapy had been used in general. Efficacy with conventional cytotoxic chemotherapy is modest at best, and the duration of benefit is limited. Although few randomized trials have been conducted, no single regimen has emerged as superior to any other, and no drug or regimen has been unequivovally shown to improve survival.

- Hepatic Artery Infusion Chemotherapy for Advanced Hepatocellular Carcinoma
- Myeong Jun Song, Si Hyun Bae
- Journal of the Korean Liver Cancer Study Group. 2012;12(1):5-9. Published online February 28, 2012
- 694 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. Surgery, percutaneous ablation and liver transplantation are the only curative treatment modality for HCC. However, a majority of patients have unresectable disease at diagnosis. Despite radical treatment, high risk of tumor recurrence is the most common problem. Therefore, there is a need for effective treatment options for patients with advanced or recurrent HCC. For patients with advanced stage of HCC according to the Barcelona Clinic Liver Cancer staging system, the multikinase inhibitor sorafenib is the current standard of care. However, hepatic arterial infusion chemotherapy (HAIC) have been applied to advanced stage HCC with a view to improve the therapeutic indexes in Asia. HAIC provides direct drug delivery into tumor bed and a greater first‐pass effect; also systemic side effects can be potentially minimized. However, the sample size of researches on HAIC was small and large randomized trials are still lacking. In this article, we describe the treatment efficacy of HAIC for advanced stage HCC and discuss future therapeutic possibilities.

Case Reports
- A Case of Advanced Hepatocellular Carcinoma which was Supervening with Renal Cell Cancer Cured by Repeated Transarterial Chemoembolization and Sorafenib after Resection
- Bun Kim, Jae Hoon Min, Seung Up Kim, Jun Yong Park, Kwang Hoon Lee, Do Youn Lee, Jin Sub Choi, Young Deuk Choi, Nam Hoon Cho, Young Nyun Park, Sang Hoon Ahn, Kwang Hyub Han, Chae Yoon Chon, Do Young Kim
- Journal of the Korean Liver Cancer Study Group. 2012;12(1):51-57. Published online February 28, 2012
- 494 Views
- 2 Downloads
-
 Abstract
Abstract
 PDF
PDF - Advanced hepatocellular carcinoma (HCC) is difficult to treat and the survival is poor. Here, we present a patient diagnosed as advanced HCC (stage IIIa) which was supervening with early renal cell cancer (stage I). The patient was treated with pre-operational transarterial chemoembolization (TACE) and surgical resection (right hepatectomy, right nephrectomy, and cholecystectomy). Sorafenib were taken continually after surgery. Multiple recurred HCC nodules in remnant liver were detected 2 months later after surgery. Combined treatment modalities including 4 sessions of TACE, and 12 cycles of 5-flurouracil (FU)/carboplatin based hepatic arterial infusional chemotherapy (HAIC) induced complete response. After the diagnosis of advanced HCC, the patient survived 36 months and experienced disease-free status for 19 months.

- A Case of Liver Transplantation after Combination of Sorafenib and Hepatic Arterial Infusion Chemotherapy in the Advanced Hepatocellular Carcinoma Patient with Portal Vein Thrombosis
- Do Seon Song, Myeong Jun Song, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon, Ho Jong Chun, Dong Goo Kim
- Journal of the Korean Liver Cancer Study Group. 2012;12(1):62-66. Published online February 28, 2012
- 667 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is the third most common malignancy in Korea where chronic hepatitis B virus is prevalent. More than 60-70% of HCC cases are diagnosed at an advanced stage that are not eligible for curative therapy such as surgical resection, liver transplantation, radiofrequency ablation, and percutaneous ethanol injection. According to Barcellona Clinic Liver Cancer (BCLC) staging and treatment, standard treatment of advanced HCC is sorafenib. And there are some reports that hepatic arterial infusion chemotherapy (HAIC) could be a beneficial therapeutic option for patients with advanced HCC. We report a case of advanced HCC with portal vein thrombosis that received liver transplantation after combination treatment of HAIC and sorafenib.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter