Search
- Page Path
- HOME > Search
Review Article
- Advancing Korean nationwide registry for hepatocellular carcinoma: a systematic sampling approach utilizing the Korea Central Cancer Registry database
- Bo Hyun Kim, E Hwa Yun, Jeong-Hoon Lee, Geun Hong, Jun Yong Park, Ju Hyun Shim, Eunyang Kim, Hyun-Joo Kong, Kyu-Won Jung, Young-Suk Lim
- J Liver Cancer. 2024;24(1):57-61. Published online March 26, 2024
- DOI: https://doi.org/10.17998/jlc.2024.03.03
- 1,022 Views
- 38 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
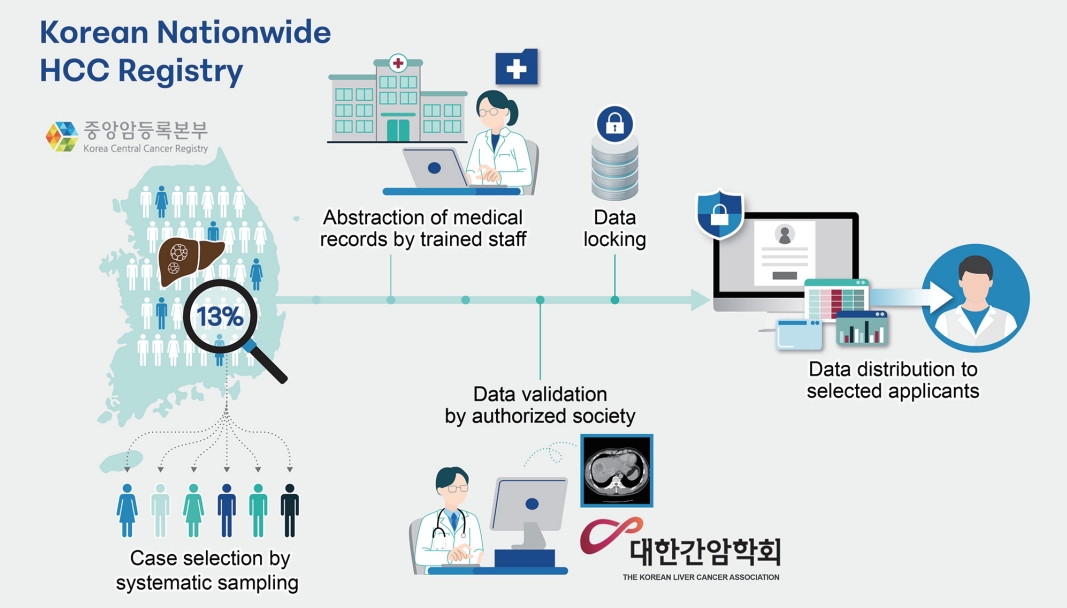
Supplementary Material - Hepatocellular carcinoma (HCC) presents a substantial public health challenge in South Korea as evidenced by 10,565 new cases annually (incidence rate of 30 per 100,000 individuals), in 2020. Cancer registries play a crucial role in gathering data on incidence, disease attributes, etiology, treatment modalities, outcomes, and informing health policies. The effectiveness of a registry depends on the completeness and accuracy of data. Established in 1999 by the Ministry of Health and Welfare, the Korea Central Cancer Registry (KCCR) is a comprehensive, legally mandated, nationwide registry that captures nearly all incidence and survival data for major cancers, including HCC, in Korea. However, detailed information on cancer staging, specific characteristics, and treatments is lacking. To address this gap, the KCCR, in partnership with the Korean Liver Cancer Association (KLCA), has implemented a systematic approach to collect detailed data on HCC since 2010. This involved random sampling of 10-15% of all new HCC cases diagnosed since 2003. The registry process encompassed four stages: random case selection, meticulous data extraction by trained personnel, expert validation, anonymization of personal data, and data dissemination for research purposes. This random sampling strategy mitigates the biases associated with voluntary reporting and aligns with stringent privacy regulations. This innovative approach positions the KCCR and KLCA as foundations for advancing cancer control and shaping health policies in South Korea.
-
Citations
Citations to this article as recorded by- Association of modifiable metabolic risk factors and lifestyle with all-cause mortality in patients with hepatocellular carcinoma
Hwi Young Kim, Hye Ah Lee, Pompilia Radu, Jean-François Dufour
Scientific Reports.2024;[Epub] CrossRef
- Association of modifiable metabolic risk factors and lifestyle with all-cause mortality in patients with hepatocellular carcinoma

Original Articles
- Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
- Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
- J Liver Cancer. 2024;24(1):81-91. Published online January 19, 2024
- DOI: https://doi.org/10.17998/jlc.2023.12.25
- 2,107 Views
- 167 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
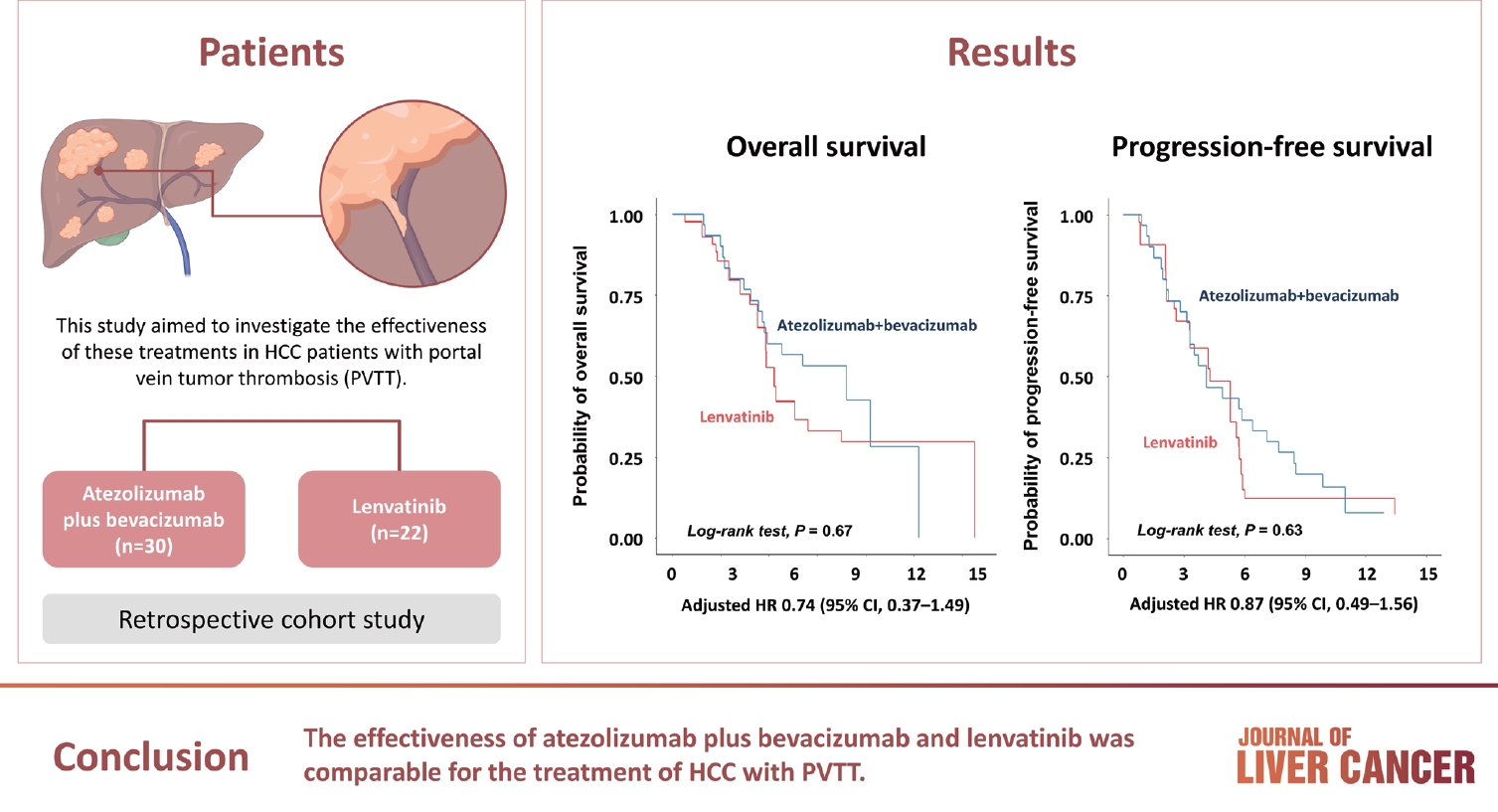
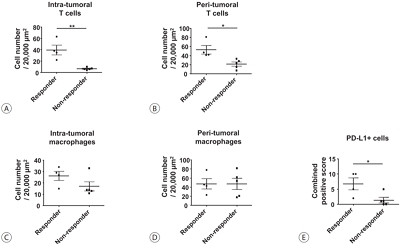
Atezolizumab plus bevacizumab and lenvatinib are currently available as first-line therapy for the treatment of unresectable hepatocellular carcinoma (HCC). However, comparative efficacy studies are still limited. This study aimed to investigate the effectiveness of these treatments in HCC patients with portal vein tumor thrombosis (PVTT).
Methods
We retrospectively included patients who received either atezolizumab plus bevacizumab or lenvatinib as first-line systemic therapy for HCC with PVTT. Primary endpoint was overall survival (OS), and secondary endpoints included progressionfree survival (PFS) and disease control rate (DCR) determined by response evaluation criteria in solid tumors, version 1.1.
Results
A total of 52 patients were included: 30 received atezolizumab plus bevacizumab and 22 received lenvatinib. The median follow-up duration was 6.4 months (interquartile range, 3.9-9.8). The median OS was 10.8 months (95% confidence interval [CI], 5.7 to not estimated) with atezolizumab plus bevacizumab and 5.8 months (95% CI, 4.8 to not estimated) with lenvatinib (P=0.26 by log-rank test). There was no statistically significant difference in OS (adjusted hazard ratio [aHR], 0.71; 95% CI, 0.34-1.49; P=0.37). The median PFS was similar (P=0.63 by log-rank test), with 4.1 months (95% CI, 3.3-7.7) for atezolizumab plus bevacizumab and 4.3 months (95% CI, 2.6-5.8) for lenvatinib (aHR, 0.93; 95% CI, 0.51-1.69; P=0.80). HRs were similar after inverse probability treatment weighting. The DCRs were 23.3% and 18.2% in patients receiving atezolizumab plus bevacizumab and lenvatinib, respectively (P=0.74).
Conclusion
The effectiveness of atezolizumab plus bevacizumab and lenvatinib was comparable for the treatment of HCC with PVTT.

- Use of doxorubicin-eluting bead transarterial chemoembolization for unresectable hepatocellular carcinoma with portal vein invasion: a prospective study
- Su Jong Yu, Yun Bin Lee, Eun Ju Cho, Jeong-Hoon Lee, Hyo-Cheol Kim, Jin Wook Chung, Jung-Hwan Yoon, Yoon Jun Kim
- J Liver Cancer. 2023;23(1):166-176. Published online March 3, 2023
- DOI: https://doi.org/10.17998/jlc.2023.02.08
- 2,793 Views
- 117 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
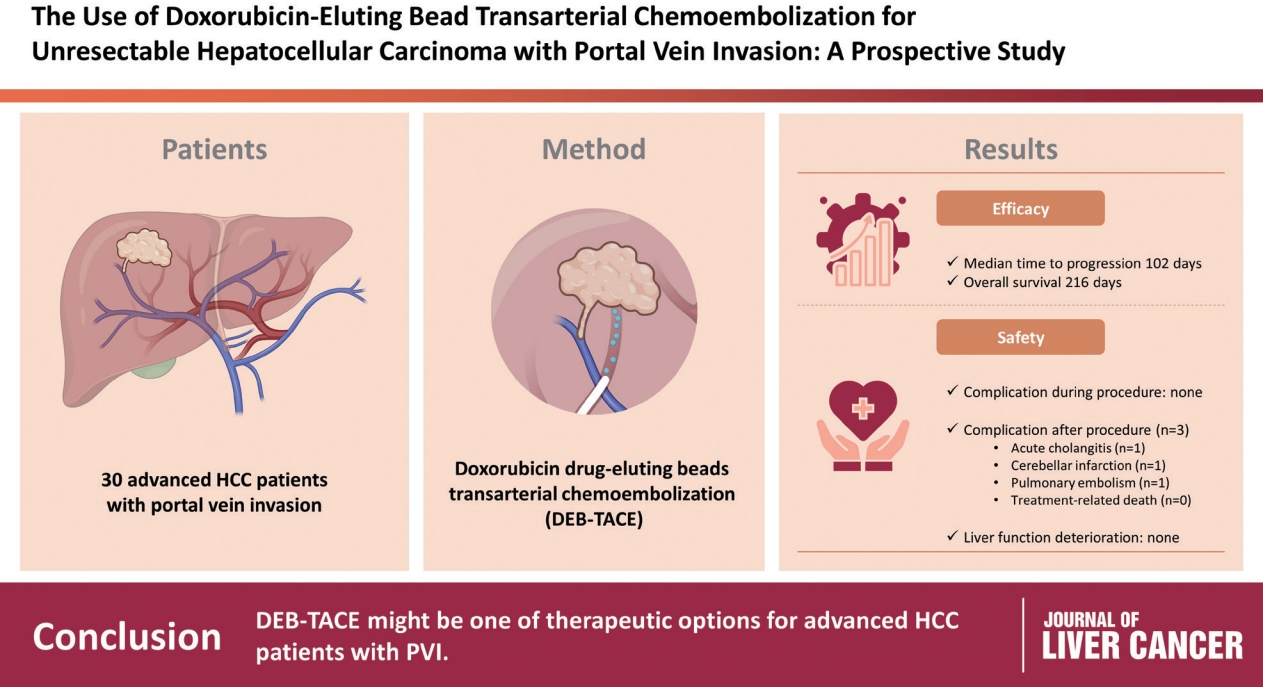
To evaluate the applicability of transarterial chemoembolization (TACE) treatment with doxorubicin drug-eluting beads (DEBs) in advanced hepatocellular carcinoma (HCC) patients with portal vein invasion (PVI).
Methods
This prospective study was approved by the institutional review board and informed consent was obtained from all participants. A total of 30 HCC patients with PVI received DEB-TACE between 2015 and 2018. The following parameters were evaluated: complications during DEB-TACE, abdominal pain, fever, and laboratory outcomes, including liver function change. Overall survival (OS), time to progression (TTP), and adverse events were also analyzed and assessed.
Results
DEBs measuring 100–300 μm in diameter were loaded with doxorubicin (150 mg per procedure). There were no complications during DEB-TACE and no significant differences in the levels of prothrombin time, serum albumin, or total bilirubin at follow-up compared to baseline. The median TTP was 102 days (95% confidence interval [CI], 42–207 days) and the median OS was 216 days (95% CI, 160–336 days). Three patients (10%) had severe adverse reactions, including transient acute cholangitis (n=1), cerebellar infarction (n=1), and pulmonary embolism (n=1), but no treatment-related death occurred.
Conclusions
DEB-TACE may be a therapeutic option for advanced HCC patients with PVI.

Case Report
- Hepatocellular carcinoma diagnosed in a patient who had Fontan operation 30 years ago: a case report
- Moon Haeng Hur, Haeryoung Kim, Jeong-Hoon Lee
- J Liver Cancer. 2022;22(2):188-193. Published online August 31, 2022
- DOI: https://doi.org/10.17998/jlc.2022.08.17
- 2,611 Views
- 65 Downloads
-
 Abstract
Abstract
 PDF
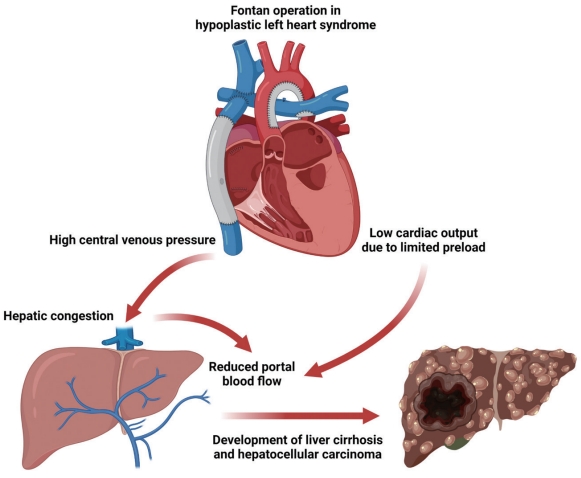
PDF - The Fontan operation is performed in patients with a single ventricle. As the systemic venous return is directly connected to the pulmonary circulation during this procedure, chronic hepatic congestion is induced, leading to Fontan-associated liver disease (FALD) including liver cirrhosis and hepatocellular carcinoma (HCC). In this report, we present a case of HCC diagnosed in a patient who underwent the Fontan operation 30 years ago. The patient underwent regular surveillance for FALD, which revealed a 4 cm-sized hepatic mass with elevated serum alpha-fetoprotein. After surgical treatment, there was no evidence of HCC recurrence during 3 years of follow-up. As the risk of HCC and Fontan-associated liver cirrhosis increases with the duration elapsed since the operation, regular surveillance should be emphasized. Serial follow-up of serum alpha-fetoprotein levels and abdominal imaging are necessary to achieve early and accurate diagnosis of HCC in post-Fontan patients.

Notice of Retraction and Replacement
- Yoon et al. Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
- Jeong-Hoon Lee
- J Liver Cancer. 2022;22(2):207-207. Published online June 8, 2022
- DOI: https://doi.org/10.17998/jlc.21.1.58.e1
- Retracts: J Liver Cancer 2021;21(1):58
- 3,417 Views
- 72 Downloads
- 1 Citation

Original Articles
- Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
- Jun Sik Yoon, Han Ah Lee, Hwi Young Kim, Dong Hyun Sinn, Dong Ho Lee, Suk Kyun Hong, Ju-Yeon Cho, Jonggi Choi, Young Chang, Hyun-Joo Kong, Eunyang Kim, Young-Joo Won, Jeong-Hoon Lee
- J Liver Cancer. 2021;21(1):58-68. Published online March 31, 2021
- DOI: https://doi.org/10.17998/jlc.21.1.58
- 7,188 Views
- 277 Downloads
- 18 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aims
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the second leading cause of cancer-related death in Korea. This study evaluated the characteristics of Korean patients newly diagnosed with HCC in 2015.
Methods
Data from the Korean Primary Liver Cancer Registry (KPLCR), a representative sample of patients newly diagnosed with HCC in Korea, were analyzed. A total of 1,558 patients with HCC registered in the KPLCR in 2015 were investigated.
Results
The median age was 61.0 years (interquartile range, 54.0-70.0 years), and men accounted for 79.7% of the subjects. Hepatitis B virus infection was the most common underlying liver disease (58.1%). According to the Barcelona Clinic Liver Cancer (BCLC) staging system, stage 0, A, B, C, and D HCCs accounted for 14.2%, 31.5%, 7.6%, 39.0%, and 7.8% of patients, respectively. Transarterial therapy (32.1%) was the most commonly performed initial treatment, followed by surgical resection (23.2%), best supportive care (20.2%), and local ablation therapy (10.7%). Overall, 34.5% of patients were treated in accordance with the BCLC guidelines: 59.2% in stage 0/A, 48.4% in stage B, 18.1% in stage C, and 71.6% in stage D. The 1-, 3-, and 5-year OS rates were 67.1%, 50.9%, and 27.0%, respectively.
Conclusions
In 2015, approximately 45% of Korean HCC cases were diagnosed at a very early or early stage, and 35% of patients underwent potentially curative initial treatment. BCLC guidance was followed in 34.5% of patients; in patients with stage B or C disease, there was relatively low adherence. -
Citations
Citations to this article as recorded by- Concurrent nivolumab and external beam radiation therapy for hepatocellular carcinoma with macrovascular invasion: A phase II study
Bo Hyun Kim, Hee Chul Park, Tae Hyun Kim, Young-Hwan Koh, Jung Yong Hong, Yuri Cho, Dong Hyun Sinn, Boram Park, Joong-Won Park
JHEP Reports.2024; 6(4): 100991. CrossRef - Identification of patients with favorable prognosis after resection in intermediate-stage-hepatocellular carcinoma
Han Ah Lee, Minjong Lee, Jeong-Ju Yoo, Ho Soo Chun, Yewan Park, Hwi Young Kim, Tae Hun Kim, Yeon Seok Seo, Dong Hyun Sinn
International Journal of Surgery.2024; 110(2): 1008. CrossRef - Factors associated with the survival outcomes of patients with untreated hepatocellular carcinoma: An analysis of nationwide data
Min Jung Kwon, Soy Chang, Ji Hoon Kim, Ji Won Han, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon, Pil Soo Sung
Frontiers in Oncology.2023;[Epub] CrossRef - The imitator of immune-tolerant chronic hepatitis B: A killer in disguise
Moon Haeng Hur, Jeong-Hoon Lee
Clinical and Molecular Hepatology.2023; 29(2): 363. CrossRef - Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study
Sun Hong Yoo, Soon Sun Kim, Sang Gyune Kim, Jung Hyun Kwon, Han-Ah Lee, Yeon Seok Seo, Young Kul Jung, Hyung Joon Yim, Do Seon Song, Seong Hee Kang, Moon Young Kim, Young-Hwan Ahn, Jieun Han, Young Seok Kim, Young Chang, Soung Won Jeong, Jae Young Jang, J
Journal of Liver Cancer.2023; 23(1): 189. CrossRef - A Case of Transverse Myelitis Following Treatment with Atezolizumab for Advanced Hepatocellular Carcinoma
Kyung Han Kim, Yang-Hyun Baek, Yeo Wool Kang, Byeol-A Yoon, Sang Yi Moon
The Korean Journal of Gastroenterology.2023; 82(1): 35. CrossRef - Comparative Analysis of Atezolizumab Plus Bevacizumab and Hepatic Artery Infusion Chemotherapy in Unresectable Hepatocellular Carcinoma: A Multicenter, Propensity Score Study
Ji Kim, Hee-Chul Nam, Chang-Wook Kim, Hee Cho, Jae-Sung Yoo, Ji Han, Jeong Jang, Jong Choi, Seung Yoon, Hyun Yang, Si Bae, Suho Kim, Jung Oh, Ho Chun, Chang Jeon, Jaegyoon Ahn, Pil Sung
Cancers.2023; 15(17): 4233. CrossRef - A nationwide study on the current treatment status and natural prognosis of hepatocellular carcinoma in elderly
Jeong-Ju Yoo, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park
Scientific Reports.2023;[Epub] CrossRef - Modeling the Risk of Liver Cancer in Adults: A Machine Learning Investigation into the Role of Obesity and Overweight
Bah Karamo, Bah Adama Ns , Jallow Amadou Wurry
Archives of Pathology and Clinical Research.2023; 7(1): 034. CrossRef - Surgical resection versus ablation for early hepatocellular carcinoma: The debate is still open
Bo Hyun Kim
Clinical and Molecular Hepatology.2022; 28(2): 174. CrossRef - Cause of death and cause-specific mortality for primary liver cancer in South Korea: A nationwide population-based study in hepatitis B virus-endemic area
Bo Hyun Kim, Dahhay Lee, Kyu-Won Jung, Young-Joo Won, Hyunsoon Cho
Clinical and Molecular Hepatology.2022; 28(2): 242. CrossRef - Impact of tumor size on hepatectomy outcomes in hepatocellular carcinoma: a nationwide propensity score matching analysis
Suk Kyun Hong, Kwang-Woong Lee, Sola Lee, Su young Hong, Sanggyun Suh, Eui Soo Han, YoungRok Choi, Nam-Joon Yi, Kyung-Suk Suh
Annals of Surgical Treatment and Research.2022; 102(4): 193. CrossRef - Efficacy and feasibility of surgery and external radiotherapy for hepatocellular carcinoma with portal invasion: A meta-analysis
Han Ah Lee, Yeon Seok Seo, In-Soo Shin, Won Sup Yoon, Hye Yoon Lee, Chai Hong Rim
International Journal of Surgery.2022; 104: 106753. CrossRef - Yoon et al. Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
Jeong-Hoon Lee
Journal of Liver Cancer.2022; 22(2): 207. CrossRef - Surveillance for hepatocellular carcinoma: It is time to move forward
Bo Hyun Kim, Yuri Cho, Joong-Won Park
Clinical and Molecular Hepatology.2022; 28(4): 810. CrossRef - Treatment patterns for hepatocellular carcinoma in patients with Child–Pugh class B and their impact on survival: A Korean nationwide registry study
Dongsub Jeon, Gi‐Won Song, Han Chu Lee, Ju Hyun Shim
Liver International.2022; 42(12): 2830. CrossRef - Metastatic breast cancer from a hepatocellular carcinoma: a case report
Hyewon Bang, Nam-Hee Kim, Seung Hye Choi, Si Hyun Bae, Eun Sun Jung, Ki Ouk Min, Yong Hwa Eom
Korean Journal of Clinical Oncology.2022; 18(2): 93. CrossRef - Current Status and Future Directions of Hepatocellular Carcinoma Surveillance Test Based on Cost-effective Analysis
Jihyun An
The Korean Journal of Gastroenterology.2021; 78(5): 255. CrossRef
- Concurrent nivolumab and external beam radiation therapy for hepatocellular carcinoma with macrovascular invasion: A phase II study

- Hepatocellular Carcinoma in Korea between 2012 and 2014: an Analysis of Data from the Korean Nationwide Cancer Registry
- Young Eun Chon, Han Ah Lee, Jun Sik Yoon, Jun Yong Park, Bo Hyun Kim, In Joon Lee, Suk Kyun Hong, Dong Hyeon Lee, Hyun-Joo Kong, Eunyang Kim, Young-Joo Won, Jeong-Hoon Lee
- J Liver Cancer. 2020;20(2):135-147. Published online September 30, 2020
- DOI: https://doi.org/10.17998/jlc.20.2.135

- 4,979 Views
- 164 Downloads
- 17 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aims
Considering the high prevalence and mortality of hepatocellular carcinoma (HCC) in Korea, accurate statistics for HCC are important. We evaluated the characteristics of Korean patients with newly diagnosed HCC.
Methods
We retrospectively evaluated data from the Korean Primary Liver Cancer Registry (KPLCR). The baseline characteristics, treatment modalities, and overall survival (OS) of 4,572 patients with HCC registered in the KPLCR between 2012 and 2014 were investigated.
Results
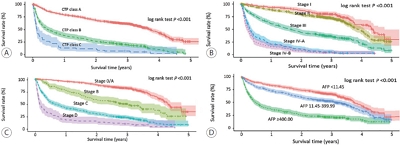
At the time of HCC diagnosis, the median age was 60.0 years, with male predominance (79.6%). Hepatitis B virus infection was the most common etiology (59.1%). The rates of Barcelona Clinic Liver Cancer (BCLC) stages 0, A, B, C, and D at diagnosis were 3.9%, 36.9%, 12.5%, 39.4%, and 7.3%, respectively. The proportion of very early or early stage HCC at diagnosis (BCLC stage 0 or A) in the 2012-2014 cohort was significantly lower than that in the 2008-2011 cohort (40.8% vs. 48.3%, P<0.001). Transarterial therapy (37.5%) was the most commonly performed initial treatment, followed by surgical resection (19.8%), best supportive care (19.1%), and local ablation (10.6%). The median OS was 2.9 years, and the 1-, 3-, and 5-year OS rates were 67.7%, 49.3% and 41.9%, respectively. The OS rate of the 2012-2014 cohort was significantly higher than that of the 2008-2011 cohort (log-rank, P<0.001).
Conclusions
The OS of HCC patients registered in the KPLCR between 2012 and 2014 significantly improved. Nevertheless, as about half of the HCC patients were diagnosed at an advanced stage, vigorous and optimized HCC screening strategies should be implemented. -
Citations
Citations to this article as recorded by- Recent Hepatocellular Carcinoma Managements in Korea: Focus on the Updated Guidelines in 2022
Yuri Cho, Bo Hyun Kim, Young-Suk Lim
Digestive Disease Interventions.2024;[Epub] CrossRef - Limited Generalizability of Retrospective Single-Center Cohort Study in Comparison to Multicenter Cohort Study on Prognosis of Hepatocellular Carcinoma
Ye Rim Kim, Sung Won Chung, Min-Ju Kim, Won-Mook Choi, Jonggi Choi, Danbi Lee, Han Chu Lee, Ju Hyun Shim
Journal of Hepatocellular Carcinoma.2024; Volume 11: 1235. CrossRef - Hepatocellular carcinoma incidence is decreasing in Korea but increasing in the very elderly
Young Eun Chon, Seong Yong Park, Han Pyo Hong, Donghee Son, Jonghyun Lee, Eileen Yoon, Soon Sun Kim, Sang Bong Ahn, Soung Won Jeong, Dae Won Jun
Clinical and Molecular Hepatology.2023; 29(1): 120. CrossRef - 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
Journal of Liver Cancer.2023; 23(1): 1. CrossRef - Factors associated with the survival outcomes of patients with untreated hepatocellular carcinoma: An analysis of nationwide data
Min Jung Kwon, Soy Chang, Ji Hoon Kim, Ji Won Han, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon, Pil Soo Sung
Frontiers in Oncology.2023;[Epub] CrossRef - Clinical practice guideline and real-life practice in hepatocellular carcinoma: A Korean perspective
Myung Ji Goh, Dong Hyun Sinn, Jong Man Kim, Min Woo Lee, Dong Ho Hyun, Jeong Il Yu, Jung Yong Hong, Moon Seok Choi
Clinical and Molecular Hepatology.2023; 29(2): 197. CrossRef - Implications of the first edition of the Korean expert consensus-based practice recommendations for transarterial chemoembolization in the management of hepatocellular carcinoma
Jin Wook Chung
Journal of Liver Cancer.2023; 23(2): 235. CrossRef - Nomogram for predicting overall survival in patients with large (>5 cm) hepatocellular carcinoma based on real-world practice
Nalee Kim, Jeong Il Yu, Hee Chul Park, Jung Yong Hong, Ho Yeong Lim, Myung Ji Goh, Yong-Han Paik
Journal of Liver Cancer.2023; 23(2): 350. CrossRef - Surgical resection versus ablation for early hepatocellular carcinoma: The debate is still open
Bo Hyun Kim
Clinical and Molecular Hepatology.2022; 28(2): 174. CrossRef - A case report of advanced hepatocellular carcinoma treated with hepatic arterial infusion chemotherapy and sorafenib combination therapy followed by metastasectomy of lung and muscle metastases
Sang Yi Moon, Sang Young Han, Yang-Hyun Baek
Journal of Liver Cancer.2022; 22(1): 57. CrossRef - Cause of death and cause-specific mortality for primary liver cancer in South Korea: A nationwide population-based study in hepatitis B virus-endemic area
Bo Hyun Kim, Dahhay Lee, Kyu-Won Jung, Young-Joo Won, Hyunsoon Cho
Clinical and Molecular Hepatology.2022; 28(2): 242. CrossRef - 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
Clinical and Molecular Hepatology.2022; 28(4): 583. CrossRef - Surveillance for hepatocellular carcinoma: It is time to move forward
Bo Hyun Kim, Yuri Cho, Joong-Won Park
Clinical and Molecular Hepatology.2022; 28(4): 810. CrossRef - 2022 KLCA-NCC Korea Practice Guidelines for the Management of Hepatocellular Carcinoma
Korean Journal of Radiology.2022; 23(12): 1126. CrossRef - Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
Jun Sik Yoon, Han Ah Lee, Hwi Young Kim, Dong Hyun Sinn, Dong Ho Lee, Suk Kyun Hong, Ju-Yeon Cho, Jonggi Choi, Young Chang, Hyun-Joo Kong, Eunyang Kim, Young-Joo Won, Jeong-Hoon Lee
Journal of Liver Cancer.2021; 21(1): 58. CrossRef - Cost-Effectiveness of Adjuvant Immunotherapy With Cytokine-Induced Killer Cell for Hepatocellular Carcinoma Based on a Randomized Controlled Trial and Real-World Data
Jeong-Yeon Cho, Sun-Hong Kwon, Eui-Kyung Lee, Jeong-Hoon Lee, Hye-Lin Kim
Frontiers in Oncology.2021;[Epub] CrossRef - Efficacy of Hepatic Arterial Infusion Chemotherapy and Radiofrequency Ablation against Hepatocellular Carcinoma Refractory to Transarterial Chemoembolization and Vascular Variation: A Case Study
Sang Yi Moon, Sang Young Han, Yang-Hyun Baek
Kosin Medical Journal.2021; 36(2): 161. CrossRef
- Recent Hepatocellular Carcinoma Managements in Korea: Focus on the Updated Guidelines in 2022

- Hepatocellular Carcinoma in Korea Between 2008 and 2011: an Analysis of Korean Nationwide Cancer Registry
- Jun Sik Yoon, Han Ah Lee, Jun Yong Park, Bo Hyun Kim, In Joon Lee, Young Eun Chon, Suk Kyun Hong, Dong Hyeon Lee, Hyun-Joo Kong, Young-Joo Won, Eunyang Kim, Jeong-Hoon Lee
- J Liver Cancer. 2020;20(1):41-52. Published online March 31, 2020
- DOI: https://doi.org/10.17998/jlc.20.1.41

- 5,407 Views
- 198 Downloads
- 15 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Backgrounds/Aims
Backgrounds/Aims: In Korea, hepatocellular carcinoma (HCC) is the sixth most common cancer and results in the second-highest cancer death rate among all cancers. We aimed to describe the characteristics of patients who were newly diagnosed with HCC in Korea between 2008 and 2011.
Methods
The Korean Primary Liver Cancer Registry (KPLCR) is a random sample consisting of approximately 15% of patients with newly diagnosed primary liver cancer registered in the Korean Central Cancer Registry. We investigated the baseline characteristics, treatment modalities, and overall survival (OS) of patients with HCC registered in the KPLCR between 2008 and 2011.
Results
A total of 6,083 patients were histologically or radiologically diagnosed with HCC. The hepatitis B virus was the predominant HCC etiology (72.0%). According to the Barcelona Clinic Liver Cancer (BCLC) staging system, stages 0, A, B, C, and D accounted for 8.6%, 39.7%, 11.5%, 33.8%, and 6.9%, respectively. Transarterial therapy (41.7%) was the most commonly performed initial treatment, followed by best supportive care (21.7%), surgical resection (16.7%), and local ablation therapies (10.6%). The overall rate of adherence to the BCLC treatment guideline was only 37.7%. The 1-, 3-, and 5-year OS rates were 65.6%, 46.2%, and 36.8%, respectively.
Conclusions
Between 2008 and 2011, approximately half of patients with HCC (48.3%) were candidates for curative treatment (BCLC stage 0 or A), but one-third of patients (33.8%) had advanced HCC (BCLC stage C). Transarterial therapy was the most commonly conducted initial treatment and the 5-year OS rate was 36.8% in this period. -
Citations
Citations to this article as recorded by- Adjuvant and neoadjuvant immunotherapies in hepatocellular carcinoma
Josep M. Llovet, Roser Pinyol, Mark Yarchoan, Amit G. Singal, Thomas U. Marron, Myron Schwartz, Eli Pikarsky, Masatoshi Kudo, Richard S. Finn
Nature Reviews Clinical Oncology.2024; 21(4): 294. CrossRef - Hepatocellular carcinoma incidence is decreasing in Korea but increasing in the very elderly
Young Eun Chon, Seong Yong Park, Han Pyo Hong, Donghee Son, Jonghyun Lee, Eileen Yoon, Soon Sun Kim, Sang Bong Ahn, Soung Won Jeong, Dae Won Jun
Clinical and Molecular Hepatology.2023; 29(1): 120. CrossRef - Implications of the first edition of the Korean expert consensus-based practice recommendations for transarterial chemoembolization in the management of hepatocellular carcinoma
Jin Wook Chung
Journal of Liver Cancer.2023; 23(2): 235. CrossRef - Surgical resection versus ablation for early hepatocellular carcinoma: The debate is still open
Bo Hyun Kim
Clinical and Molecular Hepatology.2022; 28(2): 174. CrossRef - Cause of death and cause-specific mortality for primary liver cancer in South Korea: A nationwide population-based study in hepatitis B virus-endemic area
Bo Hyun Kim, Dahhay Lee, Kyu-Won Jung, Young-Joo Won, Hyunsoon Cho
Clinical and Molecular Hepatology.2022; 28(2): 242. CrossRef - Impact of expanding hepatitis B treatment guidelines: A modelling and economic impact analysis
Young‐Suk Lim, Sang Hoon Ahn, Jae‐Jun Shim, Homie Razavi, Devin Razavi‐Shearer, Dong Hyun Sinn
Alimentary Pharmacology & Therapeutics.2022; 56(3): 519. CrossRef - Surveillance for hepatocellular carcinoma: It is time to move forward
Bo Hyun Kim, Yuri Cho, Joong-Won Park
Clinical and Molecular Hepatology.2022; 28(4): 810. CrossRef - Therapeutic Decision Making in Hepatocellular Carcinoma According to Age and Child–Pugh Class: A Nationwide Cohort Analysis in South Korea
Sunmin Park, Chai Hong Rim, Young Kul Jung, Won Sup Yoon, Alessandro Granito
Canadian Journal of Gastroenterology and Hepatology.2021; 2021: 1. CrossRef - Outcome of Immune Checkpoint Inhibitor and Molecular Target Agent Combination for Advanced Hepatocellular Carcinoma: Beyond Sorafenib Era
Nae-Yun Heo
The Korean Journal of Gastroenterology.2021; 77(3): 145. CrossRef - Rare Case of Pyogenic Brain Abscess after Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma: Case Report and Literature Review
Jun-Ho Myeong, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Journal of Liver Cancer.2021; 21(1): 81. CrossRef - Hepatocellular Carcinoma in Korea: an Analysis of the 2015 Korean Nationwide Cancer Registry
Jun Sik Yoon, Han Ah Lee, Hwi Young Kim, Dong Hyun Sinn, Dong Ho Lee, Suk Kyun Hong, Ju-Yeon Cho, Jonggi Choi, Young Chang, Hyun-Joo Kong, Eunyang Kim, Young-Joo Won, Jeong-Hoon Lee
Journal of Liver Cancer.2021; 21(1): 58. CrossRef - Glucose Variability and Risk of Hepatocellular Carcinoma in Patients with Diabetes: A Nationwide Population-Based Study
Jeong-Ju Yoo, Eun Ju Cho, Kyungdo Han, Soo Seong Heo, Bo-Yeon Kim, Dong Wook Shin, Su Jong Yu
Cancer Epidemiology, Biomarkers & Prevention.2021; 30(5): 974. CrossRef -
Lens culinaris agglutinin-reactive fraction of alpha-fetoprotein improves diagnostic accuracy for hepatocellular carcinoma
Han Ah Lee, Yoo Ra Lee, Young-Sun Lee, Young Kul Jung, Ji Hoon Kim, Hyunggin An, Hyung Joon Yim, Yoon Tae Jeen, Jong Eun Yeon, Kwan Soo Byun, Yeon Seok Seo
World Journal of Gastroenterology.2021; 27(28): 4687. CrossRef - Hepatocellular Carcinoma in Korea between 2012 and 2014: an Analysis of Data from the Korean Nationwide Cancer Registry
Young Eun Chon, Han Ah Lee, Jun Sik Yoon, Jun Yong Park, Bo Hyun Kim, In Joon Lee, Suk Kyun Hong, Dong Hyeon Lee, Hyun-Joo Kong, Eunyang Kim, Young-Joo Won, Jeong-Hoon Lee
Journal of Liver Cancer.2020; 20(2): 135. CrossRef - Efficacy of Local Treatments for Hepatocellular Carcinoma Involving the Inferior Vena Cava and/or Right Atrium
Han Ah Lee, Chai Hong Rim
Journal of Hepatocellular Carcinoma.2020; Volume 7: 435. CrossRef
- Adjuvant and neoadjuvant immunotherapies in hepatocellular carcinoma

Case Report
- Hepatocellular Carcinoma with Segmental Portal Vein Invasion Exhibiting a Complete Response after Transarterial Radioembolization
- Jun Sik Yoon, Su Jong Yu, Yun Bin Lee, Eun Ju Cho, Jeong-Hoon Lee, Yoon Jun Kim, Jung-Hwan Yoon
- J Liver Cancer. 2019;19(2):159-164. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.159

- 5,506 Views
- 78 Downloads
-
 Abstract
Abstract
 PDF
PDF - The treatment options available for patients with hepatocellular carcinoma (HCC) with portal vein invasion (PVI) include sorafenib, transarterial radioembolization (TARE), radiation therapy (RT), transarterial chemoembolization with RT, and proton beam irradiation. Herein, we present a case of HCC with segmental PVI that was managed via TARE. The patient had a 4 cm HCC that invaded the segment VIII portal vein branch without extrahepatic spread. Liver function was Child-Pugh grade A, and performance status was good. TARE was performed without any adverse events, and a radiological complete response (CR) was achieved. Thereafter, the patient was followed-up every 3-6 months without any further treatment, and the CR was maintained for >3 years. Therefore, TARE may be a useful alternative therapeutic option for patients with HCC exhibiting segmental PVI.

Original Articles
- Tenofovir and Entecavir Have Similar Renal Adverse Events on Hepatocellular Carcinoma Patients Treated with Transarterial Chemoembolization
- Young Youn Cho, Young Hwan Choi, Su Jong Yu, Eun Ju Cho, Jeong-Hoon Lee, Yoon Jun Kim, Jung-Hwan Yoon
- J Liver Cancer. 2019;19(2):128-135. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.128
- 4,110 Views
- 50 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
Tenofovir disoproxil fumarate (TDF) is potentially nephrotoxic in chronic hepatitis B patients. Hepatocellular carcinoma (HCC) patients treated using transarterial chemoembolization (TACE) are at an increased risk of renal injury. The aim of this study was to determine whether TDF is associated with more renal adverse events than entecavir (ETV) in HCC patients treated with TACE.
Methods
In this retrospective single-center study, we selected 53 HCC patients who were treated with TDF from January 2012 to July 2013 and had their first TACE procedure in the same period. These patients were matched by age and sex to patients treated with ETV.
Results
There were no significant differences in baseline characteristics, including HCC factors, and nephrotoxic drug use, between the two groups. The median follow-up period was 17.0 and 20.0 months for the TDF and ETV groups, respectively. There was no difference during the follow-up period between the TDF and ETV groups in the increase in creatinine over 0.5 mg/dL (17.0% and 17.0%, P=1.00, respectively) and the decrease in eGFR over 25% (43.4% and 41.5%, P=0.84, respectively). Multivariate analysis revealed that Child-Pugh class over B (hazard ratio [HR], 7.30; 95% confidence interval [CI] 2.79-19.10; P<0.01) was associated with increase in creatinine, and Child-Pugh class over B (HR, 82.74; 95% CI 12.31-555.83; P<0.01) and Barcelona-Clinic Liver Cancer stage over B (HR, 14.93; 95% CI 1.60-139.51; P=0.02) were associated with decrease in eGFR.
Conclusions
TDF has comparable safety to that of ETV for HCC patients undergoing TACE. -
Citations
Citations to this article as recorded by- Big Data Information under Proportional Hazard Mathematical Model in Analysis of Hepatitis B Virus Infection Data of Patients with Interventional Liver Cancer through Antiviral Therapy of Entecavir
Yichi Zhang, Shuai Zhao, Han Ding, Xiaoling Song, Huijie Miao, Xuya Cui, Jian Wang, Bing Han, Enas Abdulhay
Journal of Healthcare Engineering.2021; 2021: 1. CrossRef
- Big Data Information under Proportional Hazard Mathematical Model in Analysis of Hepatitis B Virus Infection Data of Patients with Interventional Liver Cancer through Antiviral Therapy of Entecavir

- A Case of Hepatocellular Carcinoma with Recurrent Peritoneal Metastasis after Hepatectomy Who Showed Complete Response by Surgical Resection
- Hyo Young Lee, Jeong-Hoon Lee, Joon Yeul Nam, Young Chang, Hyeki Cho, Young Youn Cho, Eung Ju Cho, Su Jong Yu, Yoon Jun Kim, Jung-Hwan Yoon
- J Liver Cancer. 2017;17(2):153-157. Published online September 30, 2017
- DOI: https://doi.org/10.17998/jlc.17.2.153
- 1,844 Views
- 18 Downloads
-
 Abstract
Abstract
 PDF
PDF - Recurrence of hepatocellular carcinoma (HCC) after hepatic resection is quite common. Peritoneal
recurrence has been considered incurable status and related to poor prognosis. Although
peritoneal metastasectomy is a therapeutic option for some selected patients with a few
peritoneal metastasis, the indication and therapeutic effect has not been clear. We report a
case
of a 61-year-old man achieving complete remission of recurrent peritoneal metastasis after repeated surgical resection by a multidisciplinary approach. Peritoneal metastasectomy might be a therapeutic option for selected patients with localized oligonodular peritoneal metastasis.

Case Report
- Two Cases of Early Recurred Hepatocellular Carcinoma after Surgical Resection Which Showed Different Outcomes
- Young Youn Cho, Jeong-Hoon Lee, Nam Joon Yi, Kwang Woong Lee, Kyung Suk Suh, Yoon Joon Kim, Jung-Hwna Yoon
- J Liver Cancer. 2015;15(2):126-131. Published online September 30, 2015
- DOI: https://doi.org/10.17998/jlc.15.2.126
- 843 Views
- 8 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) has poor prognosis, even after curative resection. Early
recurrence after curative treatment is a major cause of the poor prognosis. Pathologic factors
such as vessel invasion, satellite nodule, size of tumor and pathologic grade are prognostic
factors predicting early recurrence and poor prognosis. We share our experience of two
case
s which both showed early recurrence after curative hepatic resection, but eventually demonstrated different prognosis. Since the most common cause of death after potentially curative treatment is tumor recurrence, suppression of tumor recurrence might be linked to survival gain. Currently, there is no adjuvant therapy for HCC endorsed by international guidelines. However, recent studies have shown that antiviral treatment for hepatitis B virusrelated HCC and immunotherapy using autologous cytokine-induced killer cell reduced HCC recurrence. Further study is needed to select patients who will benefit from adjuvant treatments.

Original Article
- Transarterial Chemoembolization versus Radiofrequency Ablation for Small Hepatocellular Carcinomas with Discrepant Features on Computed Tomography and Magnetic Resonance Imaging
- Young Youn Cho, Jung Hee Kwon, Jeong-Hoon Lee, Jeong Min Lee, Jae Young Lee, Hyo-Choel Kim, Jin Wook Chung, Won-mook Choi, Eun Ju Cho, Yoon Jun Kim, Jung-Hwan Yoon, Chung Yong Kim, Hyo-Suk Lee
- J Liver Cancer. 2015;15(1):19-29. Published online March 31, 2015
- DOI: https://doi.org/10.17998/jlc.15.1.19
- 1,330 Views
- 10 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
This study compared the outcomes of patients with small hepatocellular carcinomas (HCCs) who were treated using transarterial chemoembolization (TACE) or radiofrequency ablation (RFA).
Methods
This was a post-hoc analysis of a prospective study that evaluated the diagnostic efficacy of magnetic resonance imaging (MRI) and computed tomography (CT). We analyzed 41 small hepatic nodules in 32 patients that showed typical radiologic hallmarks on both CT and gadoxate-enhanced MRI (typical nodules) and 25 small hepatic nodules from 22 patients that showed atypical radiologic hallmarks on CT and typical radiologic hallmarks on MRI (discrepant nodules).
Results
There were no significant differences in the baseline characteristics of the patients with typical and discrepant nodules. Complete response rates 1 month after TACE or RFA were 75.0% (18/24) and 94.1% (16/17; P=0.20), respectively, for the patients with typical nodules and 58.8% (10/17) and 100% (8/8; P=0.05), respectively, for the patients with discrepant nodules. Treatment failure rates after TACE or RFA were 33.3% (8/24) and 5.8% (1/17; P=0.15), respectively, for the patients with typical nodules and 47.0% (8/17) and 0.0% (0/8; P=0.02), respectively, for the patients with discrepant nodules. Among patients achieving complete response, there were no significant differences in the risk of marginal recurrence.
Conclusions
RFA provided higher complete response rates and significantly lower treatment failure rates than TACE for patients with discrepant nodules of HCC. Therefore, a treatment modality such as RFA may be preferable for small HCCs which show discrepancy on two imaging modalities.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter