Articles
- Page Path
- HOME > J Liver Cancer > Volume 23(2); 2023 > Article
-
Case Report
A single hepatic mass with two tales: hepatic tuberculosis and hepatocellular carcinoma -
Yi De Ian Koh1
 , Wei-Qiang Leow2,3,4
, Wei-Qiang Leow2,3,4
-
Journal of Liver Cancer 2023;23(2):397-401.
DOI: https://doi.org/10.17998/jlc.2023.08.30
Published online: September 8, 2023
1Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore
2Department of Anatomical Pathology, Singapore General Hospital, Singapore
3Duke-NUS Medical School, Singapore
4School of Biological Sciences, Nanyang Technological University, Singapore
-
Corresponding author: Yi De Ian Koh, Lee Kong Chian School of Medicine, Nanyang Technological University, 11 Mandalay Road, Singapore 308232, Singapore
Tel. +65-93865117 E-mail: iankohyide@gmail.com
© 2023 The Korean Liver Cancer Association.
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 977 Views
- 62 Downloads
Abstract
- Hepatic tuberculosis (HTB) is an uncommon manifestation of tuberculous infections, and there has been no proven causal link between HTB and hepatocellular carcinoma (HCC). We herein present a rare case of a synchronous presentation of HTB and HCC within a single hepatic mass. A 57-year-old Chinese gentleman with recently diagnosed sigmoid adenocarcinoma was found to have a left lower lobe pulmonary nodule and solitary hepatic mass on staging computed tomography. Biopsies showed the hepatic mass to have both HTB and HCC components. This serves as a reminder that HTB is an important differential to consider for space-occupying lesions in the liver. Histological evaluation of suspected hepatic malignancies is recommended to exclude the presence of HTB in appropriate clinical settings.
- Tuberculosis (TB) is endemic in Singapore, commonly manifesting as pulmonary TB. Hepatic tuberculosis (HTB) is rare in the absence of disseminated TB, as transmission typically occurs either via hematogenous spread from the lungs, or locally from the gastrointestinal tract.1 It is often a mimicker of malignancy, although no causal link between TB and malignancy has been established.2 We present the case of an asymptomatic Chinese patient found to have pulmonary TB with concomitant HTB and hepatocellular carcinoma (HCC).
INTRODUCTION
- A 57-year-old Chinese gentleman with metabolic syndrome, chronic kidney disease, and recently diagnosed pT3N0M0 sigmoid adenocarcinoma, was found to have a left lower lobe pulmonary nodule and a liver segment VIII lesion on staging computed tomography (CT).
- The patient was a non-smoker and non-drinker. He was asymptomatic, and specifically did not display any constitutional symptoms or respiratory symptoms. Physical examination was also unremarkable.
- Laboratory investigations showed mildly elevated alkaline phosphatase, 103 IU/L and aspartate transaminase, 43 IU/L. His inflammatory markers were unremarkable with a normal white cell count, 9.1×109/L and C-reactive protein, 8.2 mg/L. His erythrocyte edimentation rate was not measured. Carcinoembryonic antigen, 4.2 ng/L and alpha-fetoprotein, <2.7 ng/L were not elevated. CT thorax revealed a 1.9×1.3×0.7 cm nodule in the left lung lower lobe with irregular margins and tiny cavitation within, suspicious for metastasis. Magnetic resonance imaging of the liver found a hypervascular mass with arterial hyper-enhancement and subsequent washout on a background cirrhotic liver, worrisome for a primary HCC.
- He underwent laparoscopic high anterior resection for the sigmoid adenocarcinoma without adjuvant chemotherapy. He then underwent a CT-guided transthoracic biopsy of the pulmonary nodule and ultrasound-guided core biopsy of the hepatic mass.
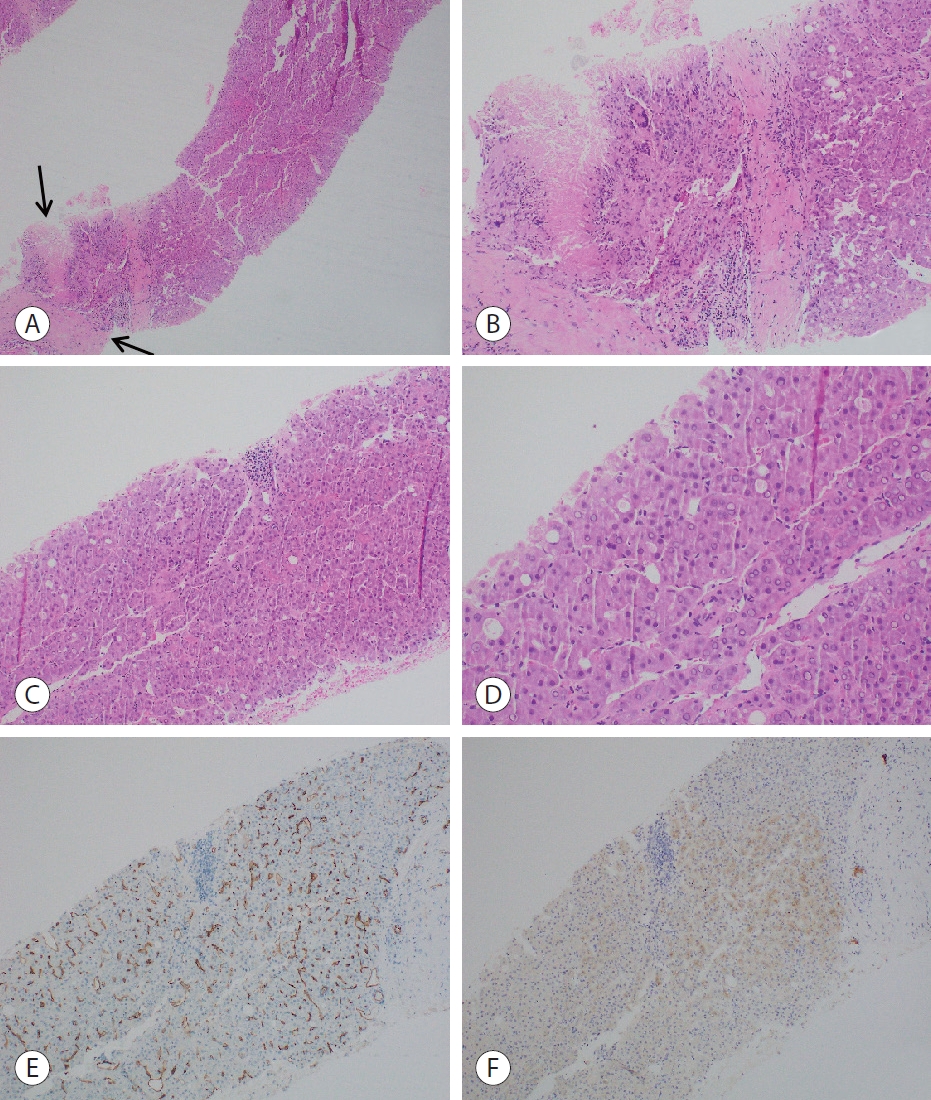
- CT-guided transthoracic biopsy of the pulmonary nodule showed caseating granulomas with positive Ziehl-Neelsen (ZN) staining for acid fast bacilli on histology, in keeping with pulmonary TB (Fig. 1).
- Ultrasound-guided core biopsy of the hepatic mass showed tumor cells with features indicative of HCC, including pseudoglandular architectures and capillarization of the liver sinusoids (Fig. 2). The HCC tumor cells also stained positive for glypican-3. In addition, there were focal areas of caseating granulomas, similar to those appreciated in the pulmonary nodule, seen on the same core biopsy. However, ZN and Fite histochemical stains were negative for acid-fast bacilli. This may be due to the poor sensitivity of the stains on the core biopsy specimens.
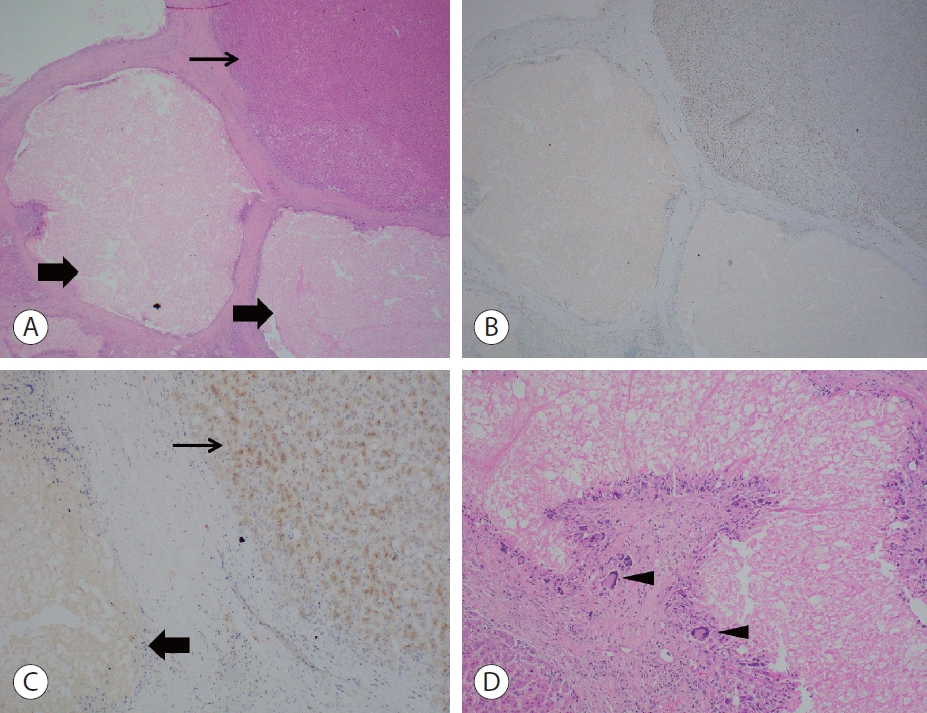
- Subsequently, the patient was started on anti-tuberculous medications and underwent a central hepatectomy. The central hepatectomy specimen showed a solid nodular tan tumor measuring 3×1.5×1.4 cm in segment IV/VIII, with surrounding foci of yellowish necrotic nodules (Fig. 3). Further histology confirmed the concomitant occurrence of HCC and necrotizing granulomas suggestive of HTB within a single lesion (Fig. 4). ZN and Fite stains were both negative, and polymerase chain reaction (PCR) for TB was not performed.
CASE REPORT
- HTB is an uncommon entity, accounting for less than 1% of all TB infections.3 Levine has previously classified HTB as miliary TB, pulmonary TB with hepatic compromise, primary HTB, focal or tuberculous abscess, and tuberculous cholangitis.4 Miliary TB is the most common form, while HTB in the absence of disseminated TB is rare.
- It is rare to find HCC with HTB within the same hepatic lesion, and the link between the two disease entities, if any, is unclear. Currently, there have only been four other known cases of such synchronous presentations in the same patient.5,6 More often, HTB is diagnosed during the work-up for a suspected HCC during histological evaluation. It also seems unlikely for tuberculosis to contribute to the pathogenesis of HCC. More likely, this patient has developed HCC with superimposed tuberculosis.
- HTB is also often misdiagnosed as an abscess, cyst, or a benign tumor, and has an average misdiagnosis rate of 93.1% in China.7 Difficulty in HTB diagnosis is also contributed by large variations in its presentation and investigation results. It commonly presents with non-specific symptoms such as fever and abdominal pain, and even then, their frequency varies greatly across numerous papers, with the incidence of fever ranging from 30% to 100%.8 Liver function tests are often normal or mildly deranged, and imaging findings can be identical to primary HCC9 with the classic triphasic CT features of arterial phase hyperintensity and portal venous phase washout. Without identification of the caseating granulomas on histology, it may be impossible to distinguish HCC from HTB. ZN staining could also be negative, and multiple modalities such as TB culture and PCR tests may be required to detect tuberculous bacteria.10 In the presence of granulomatous inflammation in the liver, other important differential diagnoses to consider would include fungal or parasitic infections, autoimmune conditions such as primary biliary cholangitis and sarcoidosis, vasculitides, as well as drug-induced granulomas.
- In the context of Singapore where TB is endemic and latent TB is present in up to 30% of the older population, it is important to consider HTB as a differential for a space-occupying lesion in the liver,10 especially in immunocompromised patients, or in those with known pulmonary TB. This allows for timely anti-tuberculous medications if necessary. It may present synchronously with HCC as seen in this patient, but more commonly it presents as a mimicker of HCC. In fact, HTB is such a great mimicker that should the clinical context warrant a high suspicion of tuberculosis, even in the presence of typical CT findings of HCC, it would be prudent to first perform a biopsy to confirm the diagnosis histologically before subjecting the patient to surgical resection of the liver.
- HTB is uncommon and its clinical and radiological features significantly overlap with those of HCC. This report presents an interesting case of a patient with concomitant HTB and HCC within a single hepatic mass. HTB continues to prove itself a diagnostic challenge and is an important differential for space-occupying lesions of the liver. In the absence of contraindications, a biopsy of hepatic lesions suspicious for malignancy should be conducted to exclude the presence of HTB, especially in appropriate clinical context with high suspicion of tuberculosis.
DISCUSSION
-
Conflicts of Interest
The authors have no conflicts of interest to disclose.
-
Ethics Statement
The SingHealth Centralised Institutional Review Board waived the requirement for ethics approval and informed consent.
-
Funding Statement
None.
-
Data Availability
Data sharing not applicable to this article as no datasets were generated or analyzed for this case report.
-
Author Contribution
Conceptualization: WQL
Data curation: YDIK
Writing original draft: YDIK
Writing review and editing: All authors
Approval of final manuscript: All authors
Article information


- 1. Akıcı M, Bozkurt E, Özdemir Ç, F Kaya. Primary hepatic tuberculosis mimicking malignancy. Int Surg J 2019;6:3078−3082.ArticlePDF
- 2. Falagas ME, Kouranos VD, Athanassa Z, Kopterides P. Tuberculosis and malignancy. QJM 2010;103:461−487.ArticlePubMed
- 3. Tatco VR, Mejia-Santos MMA, Uy JAU. The many faces of hepatic tuberculosis. TB Corner 2015;1:1−6.
- 4. Levine C. Primary macronodular hepatic tuberculosis: US and CT appearances. Gastrointest Radiol 1990;15:307−309.ArticlePubMedPDF
- 5. Limaiem F, Gargouri F, Bouraoui S, Lahmar A, Mzabi S. Co-existence of hepatocellular carcinoma and hepatic tuberculosis. Surg Infect (Larchmt) 2014;15:437−440.ArticlePubMed
- 6. Shah D, P G, S S, Koushik AK. Synchronous presentation of tuberculosis and hepatocellular carcinoma in a cirrhotic patient: a case report. Trop Doct 2020;50:71−74.ArticlePubMedPDF
- 7. Liao JR, Zhang D, Wu XL. Pulmonary tuberculosis combined with hepatic tuberculosis: a case report and literature review. Clin Respir J 2015;9:501−505.ArticlePubMedPDF
- 8. Hickey AJ, Gounder L, Moosa MY, Drain PK. A systematic review of hepatic tuberculosis with considerations in human immunodeficiency virus co-infection. BMC Infect Dis 2015;15:209. ArticlePubMedPMCPDF
- 9. Zhang L, Yang NB, Ni SL, Zhang SN, Shen CB, Lu MQ. A case of multiple macronodular hepatic tuberculosis difficult to differentiate from hepatocellular carcinoma with intrahepatic metastasis: CTguided fine needle aspiration biopsy confirmed the diagnosis. Int J Clin Exp Pathol 2014;7:8240−8244.PubMedPMC
- 10. Yang C, Liu X, Ling W, Song B, Liu F. Primary isolated hepatic tuberculosis mimicking small hepatocellular carcinoma: a case report. Medicine (Baltimore) 2020;99:e22580.PubMedPMC
References
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link Download Citation
Download Citation
- Download Citation
- Close
- Related articles
-
- Complications of immunotherapy in advanced hepatocellular carcinoma
- A multidisciplinary approach with immunotherapies for advanced hepatocellular carcinoma
- The role of lenvatinib in the era of immunotherapy of hepatocellular carcinoma
- Adult hepatoblastoma: making the challenging distinction from hepatocellular carcinoma
- Diagnostic performance of serum exosomal miRNA-720 in hepatocellular carcinoma

 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION


 Follow JLC on Twitter
Follow JLC on Twitter