Search
- Page Path
- HOME > Search
Original Article
- Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study
- Sun Hong Yoo, Soon Sun Kim, Sang Gyune Kim, Jung Hyun Kwon, Han-Ah Lee, Yeon Seok Seo, Young Kul Jung, Hyung Joon Yim, Do Seon Song, Seong Hee Kang, Moon Young Kim, Young-Hwan Ahn, Jieun Han, Young Seok Kim, Young Chang, Soung Won Jeong, Jae Young Jang, Jeong-Ju Yoo
- J Liver Cancer. 2023;23(1):189-201. Published online March 24, 2023
- DOI: https://doi.org/10.17998/jlc.2023.03.11
- 2,005 Views
- 71 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
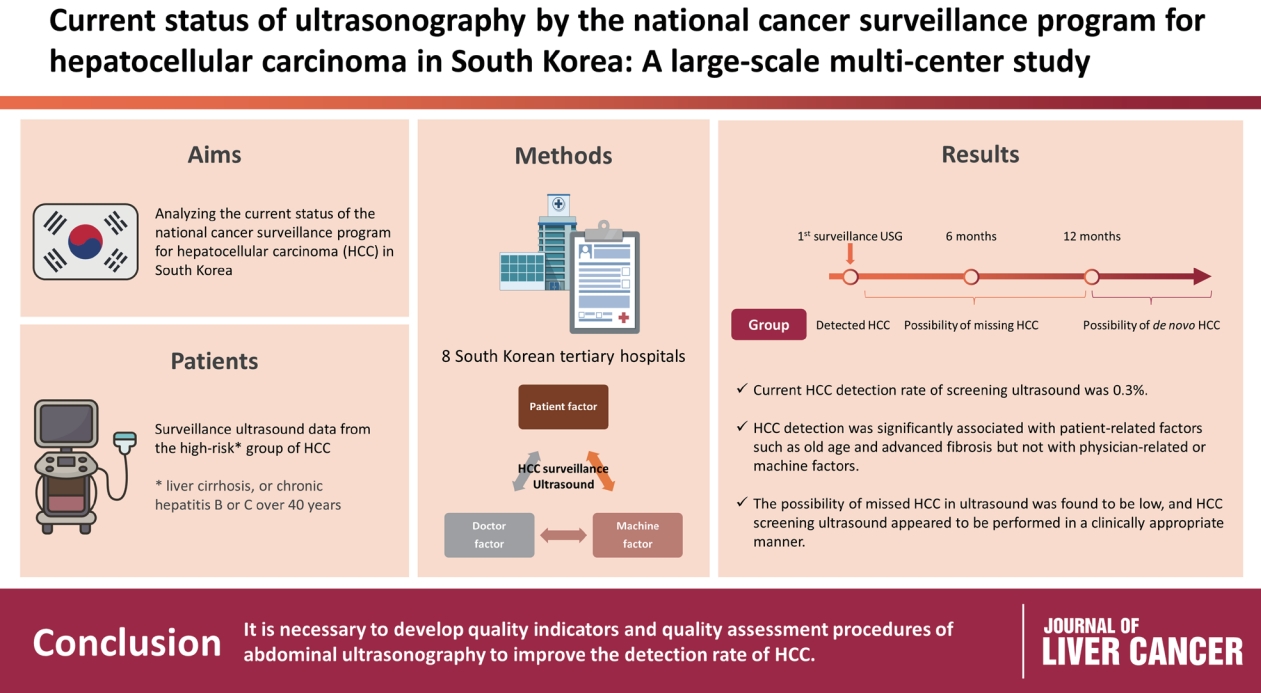
Abdominal ultrasonography (USG) is recommended as a surveillance test for high-risk groups for hepatocellular carcinoma (HCC). This study aimed to analyze the current status of the national cancer surveillance program for HCC in South Korea and investigate the effects of patient-, physician-, and machine-related factors on HCC detection sensitivity.
Methods
This multicenter retrospective cohort study collected surveillance USG data from the high-risk group for HCC (liver cirrhosis or chronic hepatitis B or C >40 years of age) at eight South Korean tertiary hospitals in 2017.
Results
In 2017, 45 experienced hepatologists or radiologists performed 8,512 USG examinations. The physicians had a mean 15.0±8.3 years of experience; more hepatologists (61.4%) than radiologists (38.6%) participated. Each USG scan took a mean 12.2±3.4 minutes. The HCC detection rate by surveillance USG was 0.3% (n=23). Over 27 months of follow-up, an additional 135 patients (0.7%) developed new HCC. The patients were classified into three groups based on timing of HCC diagnosis since the 1st surveillance USG, and no significant intergroup difference in HCC characteristics was noted. HCC detection was significantly associated with patient-related factors, such as old age and advanced fibrosis, but not with physician- or machine-related factors.
Conclusions
This is the first study of the current status of USG as a surveillance method for HCC at tertiary hospitals in South Korea. It is necessary to develop quality indicators and quality assessment procedures for USG to improve the detection rate of HCC. -
Citations
Citations to this article as recorded by- The Epidemiology of Hepatitis B Virus Infection in Korea: 15-Year Analysis
Log Young Kim, Jeong-Ju Yoo, Young Chang, Hoongil Jo, Young Youn Cho, Sangheun Lee, Dong Hyeon Lee, Jae Young Jang
Journal of Korean Medical Science.2024;[Epub] CrossRef - Long-Term HBsAg Titer Kinetics with Entecavir/Tenofovir: Implications for Predicting Functional Cure and Low Levels
Soon Kyu Lee, Soon Woo Nam, Jeong Won Jang, Jung Hyun Kwon
Diagnostics.2024; 14(5): 495. CrossRef
- The Epidemiology of Hepatitis B Virus Infection in Korea: 15-Year Analysis

Review Articles
- Imaging Modalities for Hepatocellular Carcinoma Surveillance: Expanding Horizons beyond Ultrasound
- Hyo Jung Park, So Yeon Kim
- J Liver Cancer. 2020;20(2):99-105. Published online September 30, 2020
- DOI: https://doi.org/10.17998/jlc.20.2.99
- 5,403 Views
- 211 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
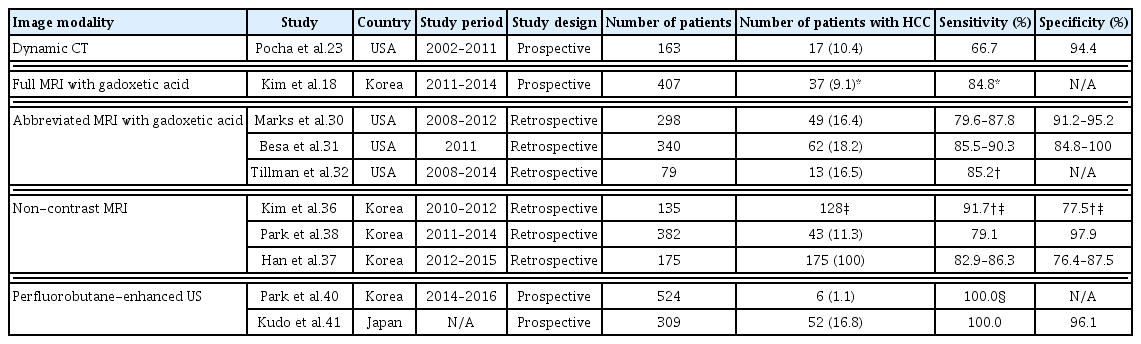
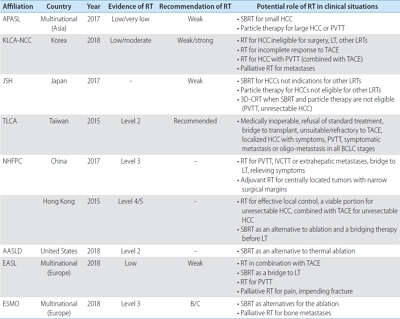
PDF - In Asian countries favoring loco-regional treatment such as surgical resection or ablation, very early-stage hepatocellular carcinoma (HCC) should be the main target for surveillance. Even though ultrasound (US) has been accepted as a primary imaging modality for HCC surveillance, its performance in detecting very early-stage HCCs is insufficient. Moreover, in more than 20% of patients at high risk for HCC, visualization of the liver on US may be limited owing to the advanced distortion and heterogeneity of the liver parenchyma. Recently revised HCC clinical guidelines allow the use of alternative surveillance tools including computed tomography or magnetic resonance imaging in patients with inadequate US exams. This paper summarizes the findings of recent studies using imaging modalities other than US as surveillance tools for HCC as well as strengths and limitations of these modalities.
-
Citations
Citations to this article as recorded by- Imaging features of hepatobiliary MRI and the risk of hepatocellular carcinoma development
Jong-In Chang, Dong Hyun Sinn, Woo Kyoung Jeong, Jeong Ah Hwang, Ho Young Won, Kyunga Kim, Wonseok Kang, Geum-Youn Gwak, Yong-Han Paik, Moon Seok Choi, Joon Hyeok Lee, Kwang Cheol Koh, Seung-Woon Paik
Scandinavian Journal of Gastroenterology.2022; 57(12): 1470. CrossRef
- Imaging features of hepatobiliary MRI and the risk of hepatocellular carcinoma development

- Liver Magnetic Resonance Imaging for Hepatocellular Carcinoma Surveillance
- So Hyun Park, Bohyun Kim
- J Liver Cancer. 2020;20(1):25-31. Published online March 31, 2020
- DOI: https://doi.org/10.17998/jlc.20.1.25
- 6,125 Views
- 252 Downloads
- 6 Citations
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) surveillance is recommended when the annual incidence of HCC exceeds 1.5%. In 2018, several international guidelines included alternative surveillance modalities, such as computed tomography and magnetic resonance imaging (MRI), as alternatives for patients with inadequate surveillance with an ultrasound. Currently, abbreviated MRI selectively includes several key sequences and is emerging as an effective tool for HCC surveillance with reduced cost and scan time and the required diagnostic performance. The incidence of HCC substantially impacts the benefits of surveillance in terms of cost-effectiveness. Therefore, we need to individualize imaging surveillance of HCC, tailor screening, and determine risk-stratified strategies. The purpose of this article was to present a brief overview of the diagnostic performance and cost-effectiveness of liver MRI as an HCC surveillance tool.
-
Citations
Citations to this article as recorded by- A Post-International Gastrointestinal Cancers’ Conference (IGICC) Position Statements
Suayib Yalcin, Sahin Lacin, Ahmed Kaseb, Bora Peynircioğlu, Murat Cantasdemir, Barbaros Çil, Pervin Hurmuz, Ahmet Doğrul, Murat Bozkurt, Hüseyin Abali, Okan Akhan, Halis Şimşek, Berksoy Sahin, Faruk Aykan, İdris Yücel, Gürkan Tellioğlu, Fatih Selçukbirici
Journal of Hepatocellular Carcinoma.2024; Volume 11: 953. CrossRef - Adding MRI as a Surveillance Test for Hepatocellular Carcinoma in Patients with Liver Cirrhosis Can Improve Prognosis
Su Jong Yu, Jeong-Ju Yoo, Dong Ho Lee, Su Jin Kim, Eun Ju Cho, Se Hyung Kim, Jeong-Hoon Lee, Yoon Jun Kim, Jeong Min Lee, Jae Young Lee, Jung-Hwan Yoon
Biomedicines.2023; 11(2): 382. CrossRef - MRI features of histologic subtypes of hepatocellular carcinoma: correlation with histologic, genetic, and molecular biologic classification
Ja Kyung Yoon, Jin-Young Choi, Hyungjin Rhee, Young Nyun Park
European Radiology.2022; 32(8): 5119. CrossRef - Imaging features of hepatobiliary MRI and the risk of hepatocellular carcinoma development
Jong-In Chang, Dong Hyun Sinn, Woo Kyoung Jeong, Jeong Ah Hwang, Ho Young Won, Kyunga Kim, Wonseok Kang, Geum-Youn Gwak, Yong-Han Paik, Moon Seok Choi, Joon Hyeok Lee, Kwang Cheol Koh, Seung-Woon Paik
Scandinavian Journal of Gastroenterology.2022; 57(12): 1470. CrossRef - Potential of a Non-Contrast-Enhanced Abbreviated MRI Screening Protocol (NC-AMRI) in High-Risk Patients under Surveillance for HCC
François Willemssen, Quido de Lussanet de la Sablonière, Daniel Bos, Jan IJzermans, Robert De Man, Roy Dwarkasing
Cancers.2022; 14(16): 3961. CrossRef - Prognosis of hepatocellular carcinoma patients diagnosed under regular surveillance: potential implications for surveillance goal
Joo Hye Song, Myung Ji Goh, Yewan Park, Joo Hyun Oh, Wonseok Kang, Dong Hyun Sinn, Geum-Youn Gwak, Yong-Han Paik, Moon Seok Choi, Joon Hyeok Lee, Kwang Cheol Koh, Seung Woon Paik
Scandinavian Journal of Gastroenterology.2021; 56(3): 274. CrossRef
- A Post-International Gastrointestinal Cancers’ Conference (IGICC) Position Statements

Original Article
- Discrepancy between the Actual Clinical Status of Patients with Hepatocellular Carcinoma and Expectations from Hepatocellular Carcinoma Surveillance: a Single-Center Study
- Nak Min Kim, Young Seok Doh, Ji Woong Jang, Seok-Hwan Kim, Hyuk Soo Eun, Jae Hyuck Jun, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
- J Liver Cancer. 2019;19(1):30-37. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.30

- 4,869 Views
- 102 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
The National Liver Cancer Screening Program (NLCSP) has been implemented for the past 15 years in Korea. However, the actual clinical experience in Korea is inconsistent with the expectations of the hepatocellular carcinoma (HCC) surveillance program. To evaluate the actual clinical situation of HCC diagnoses, we investigated disease severity in patients with HCC and the diagnostic environment.
Methods
From January 2011 to December 2015, all patients who were diagnosed with HCC in a single secondary hospital in Daejeon city were retrospectively enrolled in this study. Severity of HCC was evaluated according to the Barcelona Clinic Liver Cancer (BCLC) staging system.
Results
Over the course of 5 years, 298 participants were enrolled. The mean age of participants was 64.0 years. Positive hepatitis B surface antigen was confirmed in 134 patients (45.0%), 35 patients (11.7%) tested positive for anti-hepatitis C virus antibody, and 93 patients (32.2%) had more than 40 g/day of alcohol consumption. The proportions of patients according to BCLC stages were as follows: BCLC-0, 28 patients (9.4%); BCLC-A, 42 patients (14.1%); BCLC-B, 26 patients (8.7%); BCLC-C, 134 patients (45.0%); and BCLC-D, 68 patients (22.8%). The diagnostic environments were as follows: 19 patients were in the NLCSP group (6.4%), 114 in the group with presenting signs (38.3%), 110 in the regular outpatient care group (36.9%), and 55 patients in the incidental diagnosis group (18.5%).
Conclusions
Most patients (67.8%) had advanced stage HCC at diagnosis, and curative treatment was not indicated due to the severity disease. Thus, the actual situation is far worse than the theoretical expectation of HCC surveillance, suggesting that many high-risk patients for HCC are missed in surveillance. -
Citations
Citations to this article as recorded by- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis
Wojciech Książek, Filip Turza, Paweł Pławiak
International Journal for Numerical Methods in Biomedical Engineering.2022;[Epub] CrossRef - Imaging Modalities for Hepatocellular Carcinoma Surveillance: Expanding Horizons beyond Ultrasound
Hyo Jung Park, So Yeon Kim
Journal of Liver Cancer.2020; 20(2): 99. CrossRef
- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis

Review Articles
- Treatment and Surveillance of Hepatocellular Carcinoma in Elderly Patients
- Rho, Seoung Yoon , Lee, Hyun Woong , Kim, Kyung Sik
- J Liver Cancer. 2018;18(2):103-114. Published online September 30, 2018
- DOI: https://doi.org/10.17998/jlc.18.2.103
- 2,363 Views
- 74 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is the third most common cancer in the digestive system based on survey of domestic cancer incidence, and the ratio of elderly aged 65 or older is expected to rise steadily, leading to a higher incidence of total hepatocellular carcinoma. The most important thing in treating these older patients with HCC is to assess the benefits and risks of the treatment in advance. In other words, the benefit of treatment should be greater than the reduction of survival period or maladjustment due to treatment. Based on these perspectives, we examined how the detailed treatment of hepatocellular carcinoma differs from that of general treatment in elderly patients. In conclusion, older age was not a definite prognostic factor of survival risk-benefit comparison in the most treatment modalities. However it should be carefully considered and approached about possible complications in treating HCC in elderly patients.

- Surveillance for Hepatocellular Carcinoma
- Kung-Hung Lin, Wei-Lun Tsai Tsai
- Journal of the Korean Liver Cancer Study Group. 2013;13(2):93-104. Published online September 30, 2013
- DOI: https://doi.org/10.17998/jlc.13.2.93
- 1,115 Views
- 16 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is the fifth most common cancer and the third leading cause of cancer death worldwide. HCC is a suitable disease for surveillance programs because it is relatively common in patients with chronic liver disease, and has very good prognosis if diagnosed at an early stage. When HCC presents with clinical symptoms, the tumor is typically very far advanced and the patient has few therapeutic options. Individuals with chronic viral hepatitis and other forms of liver disease are at risk for developing HCC. Thus, screening and surveillance for HCC would appear to be very appropriate. However, there is no definitive evidence that surveillance improves patient outcomes and the current surveillance tests have less than optimal sensitivity, specificity and accuracy. Nonetheless, measurement of alpha-fetoprotein levels in serum and ultrasound of the liver have become routine practice in many countries, despite a lack of evidence of their overall benefit. Clearly, better methods are needed for early diagnosis of HCC. This review outlines the target population at risk for HCC and diagnostic techniques for screening and surveillance.

- Early Detection of HCC: What is the Best Strategy?
- Do Young Kim
- Journal of the Korean Liver Cancer Study Group. 2012;12(2):113-119. Published online September 30, 2012
- 510 Views
- 8 Downloads
-
 Abstract
Abstract
 PDF
PDF - HCC is an appropriate cancer to apply surveillance program for early cancer detection. Currently, liver ultrasonography (US) combined with serum biomarker, alpha‐fetoprotein (AFP), measurement every 6 months is the standard method of HCC surveillance. Although US is the most widely used tool, its sensitivity in early HCC (within Milan criteria) detection during surveillance is only 63%. AFP is the representative biomarker for both HCC surveillance and diagnosis. The unsatisfactory performance of AFP as a surveillance tool requires discovery of novel biomarker or combination with other serum markers. Desgamma‐ carboxy prothrombin (DCP) and AFP‐L3 are candidate biomarkers which are complementary to AFP. AFP‐L3 is an emerging biomarker for diagnosis of HCC, but it needs to be validated as a surveillance tool. Regarding surveillance interval, 6 months or less seems to be superior to more longer interval in terms of early HCC detection and survival improvement. The strategies of HCC surveillance are different in countries according to health care system including available resources and health insurance coverage. Many studies demonstrated that rate of early cancer detection and application of curative therapies was increased, along with survival benefit, by HCC surveillance which is now the standard care, not just a recommendation. Improved ultrasound technology and biomarker discovery such as a specific microRNA are necessary to make more progress in HCC surveillance.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter