Previous issues
- Page Path
- HOME > Articles and issues > Previous issues
Review Articles
- Recent Advances and Future Directions in Immunotherapeutics for Hepatocellular Carcinoma
- Yuri Cho, Jimin Han, Won Kim
- J Liver Cancer. 2019;19(1):1-11. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.1

- 5,410 Views
- 149 Downloads
- 5 Citations
-
 Abstract
Abstract
 PDF
PDF - Systemic target therapeutic drugs, such as sorafenib, lenvatinib, or regorafenib are the only drugs that are known to be effective against advanced hepatocellular carcinoma (HCC). However, these agents show a limited efficacy in killing residual tumors. Immunotherapy is an alternative approach to this treatment and has been used to successfully treat different cancers, including HCC. HCC is an inflammation-induced cancer and represents a very interesting target for immunotherapeutics. Immunotherapies aim to reverse the immune tolerance and suppression found in tumor microenvironments and include approaches, such as adoptive cell therapy, immune checkpoint inhibition, and cancer vaccination. Adoptive cell therapy uses autologous natural killer or cytokine-induced killer cells by cultivating them ex vivo and subsequently reinfusing them into the patient. Immune checkpoint inhibitors reactivate tumorspecific T cells by suppressing checkpoint-mediated inhibitory signaling. Cancer vaccination induces a tumor-specific immune response by activating effector T lymphocytes. A wide range of potential immunotherapy-related adverse events occur; therefore, a multidisciplinary collaborative management is required across the clinical spectrum. This review summarizes the current status of immunotherapy for HCC and provides a perspective on its future applications.
-
Citations
Citations to this article as recorded by- Exploring the potential of Toxoplasma gondii in drug development and as a delivery system
Chanjin Yoon, Yu Seong Ham, Woo Jin Gil, Chul-Su Yang
Experimental & Molecular Medicine.2024; 56(2): 289. CrossRef - Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
Journal of Liver Cancer.2024; 24(1): 81. CrossRef - Revamping the innate or innate-like immune cell-based therapy for hepatocellular carcinoma: new mechanistic insights and advanced opportunities
Disha D. Shah, Bhavarth P. Dave, Parv A. Patel, Mehul R. Chorawala, Vishvas N. Patel, Palak A. Shah, Manish P. Patel
Medical Oncology.2023;[Epub] CrossRef - Differences between exhausted CD8+ T cells in hepatocellular carcinoma patients with and without uremia
Chen Xiaohong, Zou Jianzhou, Shen Bo, Lv Wenlv, Cao Xuesen, Xiang Fangfang
Canadian Journal of Physiology and Pharmacology.2021; 99(4): 395. CrossRef - Nivolumab for Advanced Hepatocellular Carcinoma with Multiple Lung Metastases after Sorafenib Failure
Jaewoong Kim, Jin Won Chang, Jun Yong Park
Journal of Liver Cancer.2020; 20(1): 72. CrossRef
- Exploring the potential of Toxoplasma gondii in drug development and as a delivery system

- Clinical Application of Liver Stiffness Measurement for Assessing the Risk of Hepatocellular Carcinoma
- Jeong-Ju Yoo, Eun-Ae Jung, Sang Gyune Kim
- J Liver Cancer. 2019;19(1):12-18. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.12

- 4,382 Views
- 101 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - The most significant risk factor for hepatocellular carcinoma (HCC) is the presence of cirrhosis or advanced fibrosis of the liver. Liver biopsy was traditionally considered the gold standard for assessing the liver fibrosis burden. Recently, non-invasive methods, particularly transient elastography (TE), have proven effective at measuring fibrosis and determining cirrhosis. Clinical application of TE ranges from measuring fibrosis to predicting long-term prognosis and treatment response. Here, we focus on recent studies on the prognostic value of TE for predicting HCC.
-
Citations
Citations to this article as recorded by- Metabolic dysfunction associated fatty liver disease and the risk of hepatocellular carcinoma
Byeong Geun Song, Sung Chul Choi, Myung Ji Goh, Wonseok Kang, Dong Hyun Sinn, Geum-Youn Gwak, Yong-Han Paik, Moon Seok Choi, Joon Hyeok Lee, Seung Woon Paik
JHEP Reports.2023; : 100810. CrossRef
- Metabolic dysfunction associated fatty liver disease and the risk of hepatocellular carcinoma

- Conventional Chemoembolization for Hepatocellular Carcinoma: Role of Cone-Beam Computed Tomography Guidance
- In Joon Lee, Jin Wook Chung
- J Liver Cancer. 2019;19(1):19-29. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.19

- 5,501 Views
- 151 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
PDF - Conventional chemoembolization using Lipiodol-based regimens was introduced in the 1980s, and it is currently recommended as the primary treatment modality for patients with unresectable, intermediate, or locally advanced hepatocellular carcinoma (HCC) by the international guidelines. For better therapeutic efficacy and safety, chemoembolization should be performed as selectively as possible through tumor-feeding arteries, based on the detection of arterial supply to the HCC. With the technical advancement of flat-panel detector, cone-beam computed tomography (CBCT) is mounted on the C-arm of the angiographic machine. CBCT facilitates the detection of small occult HCCs and fine tumor-feeding arteries, recognition of extrahepatic collateral supply, navigation of a microcatheter to the target feeding arteries, prevention of non-target embolization, and intraprocedural assessment of the completeness of treatment with chemoembolization. These functions performed by CBCT ultimately improve the safety and efficacy of chemoembolization and may contribute to improving the prognosis of the patient with HCC.
-
Citations
Citations to this article as recorded by- Transarterial Chemoembolization for Hepatocellular Carcinoma: 2023 Expert Consensus-Based Practical Recommendations of the Korean Liver Cancer Association
Yuri Cho, Jin Woo Choi, Hoon Kwon, Kun Yung Kim, Byung Chan Lee, Hee Ho Chu, Dong Hyeon Lee, Han Ah Lee, Gyoung Min Kim, Jung Suk Oh, Dongho Hyun, In Joon Lee, Hyunchul Rhim
Korean Journal of Radiology.2023; 24(7): 606. CrossRef - Transarterial chemoembolization for hepatocellular carcinoma: 2023 expert consensus-based practical recommendations of the Korean Liver Cancer Association
Yuri Cho, Jin Woo Choi, Hoon Kwon, Kun Yung Kim, Byung Chan Lee, Hee Ho Chu, Dong Hyeon Lee, Han Ah Lee, Gyoung Min Kim, Jung Suk Oh, Dongho Hyun, In Joon Lee, Hyunchul Rhim
Journal of Liver Cancer.2023; 23(2): 241. CrossRef - Transarterial chemoembolization for hepatocellular carcinoma: 2023 Expert consensus-based practical recommendations of the Korean Liver Cancer Association
Yuri Cho, Jin Woo Choi, Hoon Kwon, Kun Yung Kim, Byung Chan Lee, Hee Ho Chu, Dong Hyeon Lee, Han Ah Lee, Gyoung Min Kim, Jung Suk Oh, Dongho Hyun, In Joon Lee, Hyunchul Rhim
Clinical and Molecular Hepatology.2023; 29(3): 521. CrossRef - The efficacy of TACE; how can automated feeder software help?
Hassan Abdelsalam, Doaa M. Emara, Ehab M. Hassouna
Egyptian Journal of Radiology and Nuclear Medicine.2022;[Epub] CrossRef
- Transarterial Chemoembolization for Hepatocellular Carcinoma: 2023 Expert Consensus-Based Practical Recommendations of the Korean Liver Cancer Association

Original Articles
- Discrepancy between the Actual Clinical Status of Patients with Hepatocellular Carcinoma and Expectations from Hepatocellular Carcinoma Surveillance: a Single-Center Study
- Nak Min Kim, Young Seok Doh, Ji Woong Jang, Seok-Hwan Kim, Hyuk Soo Eun, Jae Hyuck Jun, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
- J Liver Cancer. 2019;19(1):30-37. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.30

- 4,869 Views
- 102 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
The National Liver Cancer Screening Program (NLCSP) has been implemented for the past 15 years in Korea. However, the actual clinical experience in Korea is inconsistent with the expectations of the hepatocellular carcinoma (HCC) surveillance program. To evaluate the actual clinical situation of HCC diagnoses, we investigated disease severity in patients with HCC and the diagnostic environment.
Methods
From January 2011 to December 2015, all patients who were diagnosed with HCC in a single secondary hospital in Daejeon city were retrospectively enrolled in this study. Severity of HCC was evaluated according to the Barcelona Clinic Liver Cancer (BCLC) staging system.
Results
Over the course of 5 years, 298 participants were enrolled. The mean age of participants was 64.0 years. Positive hepatitis B surface antigen was confirmed in 134 patients (45.0%), 35 patients (11.7%) tested positive for anti-hepatitis C virus antibody, and 93 patients (32.2%) had more than 40 g/day of alcohol consumption. The proportions of patients according to BCLC stages were as follows: BCLC-0, 28 patients (9.4%); BCLC-A, 42 patients (14.1%); BCLC-B, 26 patients (8.7%); BCLC-C, 134 patients (45.0%); and BCLC-D, 68 patients (22.8%). The diagnostic environments were as follows: 19 patients were in the NLCSP group (6.4%), 114 in the group with presenting signs (38.3%), 110 in the regular outpatient care group (36.9%), and 55 patients in the incidental diagnosis group (18.5%).
Conclusions
Most patients (67.8%) had advanced stage HCC at diagnosis, and curative treatment was not indicated due to the severity disease. Thus, the actual situation is far worse than the theoretical expectation of HCC surveillance, suggesting that many high-risk patients for HCC are missed in surveillance. -
Citations
Citations to this article as recorded by- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis
Wojciech Książek, Filip Turza, Paweł Pławiak
International Journal for Numerical Methods in Biomedical Engineering.2022;[Epub] CrossRef - Imaging Modalities for Hepatocellular Carcinoma Surveillance: Expanding Horizons beyond Ultrasound
Hyo Jung Park, So Yeon Kim
Journal of Liver Cancer.2020; 20(2): 99. CrossRef
- NCA‐GA‐SVM: A new two‐level feature selection method based on neighborhood component analysis and genetic algorithm in hepatocellular carcinoma fatality prognosis

- High-dose versus Low-dose 5-Fluorouracil and Cisplatin Based Hepatic Arterial Infusion Chemotherapy for Advanced Hepatocellular Carcinoma
- Chae-June Lim, Ji-Yun Hong, Yang-Seok Ko, Min-Woo Chung, Chung-Hwan Jun, Sung-Kyu Choi, Sung-Bum Cho
- J Liver Cancer. 2019;19(1):38-45. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.38
- 4,696 Views
- 176 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
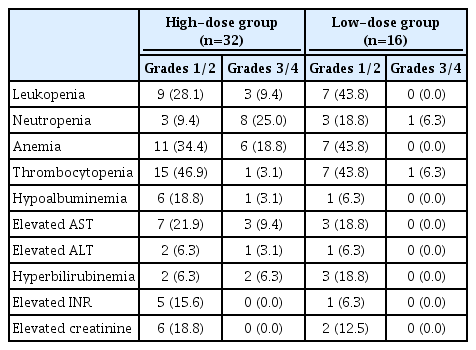
PDF - Backgrounds/Aims
Hepatic arterial infusion chemotherapy (HAIC) has been reported as an effective treatment for advanced hepatocellular carcinoma. The aim of this study is to compare the effect and safety between a high-dose regimen (750 mg/m2 5-fluorouracil [FU] and 25 mg/m2 cisplatin on day 1-4) and a low-dose regimen (500 mg/m2 5-FU on day 1-3 with 60 mg/m2 cisplatin on day 2).
Methods
A total of 48 patients undergoing HAIC were retrospectively analyzed. Thirty-two patients were treated with the high-dose and 16 patients with the low-dose regimen.
Results
Complete response (CR), partial response (PR), stable disease (SD), and progressive disease were noted in one (3.1%), 15 (46.9%), three (9.4%), and 13 patients (40.6%) in the highdose group, and 0 (0%), one (6.3%), eight (50%), and seven patients (43.8%) in the low-dose group (p=0.002). The disease control rate (CR, PR, and SD) did not differ between groups (59.4% vs. 56.3%, p=1.000), but the objective response rate (CR and PR) was significantly higher in the high-dose group (50.0% vs. 6.3%, p=0.003). The median progression free survival did not differ between groups (4.0 vs. 6.0, p=0.734), but overall survival was significantly longer in the high-dose group (not reached vs. 16.0, p=0.028). Fourteen (43.8%) patients in the highdose group and two patients (12.5%) in the low-dose group experienced grade 3-4 toxicities (p=0.050).
Conclusions
High dose HAIC may achieve better tumor response and may improve overall survival compared to a low-dose regimen. However, the high-dose regimen should be administered cautiously because of the higher incidence of adverse events. -
Citations
Citations to this article as recorded by- A programmed cell death-related gene signature to predict prognosis and therapeutic responses in liver hepatocellular carcinoma
Xinyu Gu, Jie Pan, Yanle Li, Liushun Feng
Discover Oncology.2024;[Epub] CrossRef - Development of a novel chromatographic method for concurrent determination of 5-fluorouracil and cisplatin: Validation, greenness evaluation, and application on drug-eluting film
Souha H. Youssef, Franklin Afinjuomo, Yunmei Song, Sanjay Garg
Microchemical Journal.2021; 168: 106510. CrossRef
- A programmed cell death-related gene signature to predict prognosis and therapeutic responses in liver hepatocellular carcinoma

- Effect of PTEN Polymorphism on the Development of Hepatitis B Virus-associated Hepatocellular Carcinoma
- Soon Sun Kim, Jung Woo Eun, Hyo Jung Cho, Hyun-Young Lee, Chul Won Seo, Gil Ho Lee, So Young Yoon, Choong Kyun Noh, Sung Won Cho, Jae Youn Cheong
- J Liver Cancer. 2019;19(1):46-54. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.46

- 4,688 Views
- 133 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
Phosphatase and tensin homolog (PTEN) is a known tumor suppressor gene that is downregulated in hepatocellular carcinoma (HCC). Here, we investigated the association between single nucleotide polymorphisms (SNPs) of PTEN and HCC development in patients with hepatitis B virus (HBV) infection.
Methods
Six SNPs of PTEN at positions rs1234221, rs1903860, rs1234220, rs1903858, rs2299941, and rs17431184 were analyzed in a development population (417 chronic HBV carriers without HCC and 281 chronic HBV carriers with HCC). PTEN rs1903858, rs1903860, and rs2299941 SNPs were further assessed for the development of HCC in a validation population of 200 patients with HBV-related liver cirrhosis.
Results
In the development population, PTEN rs1903860 C allele, rs1903858 G allele, and rs2299941 G allele were associated with a low risk of HCC. The haplotype A-T-A-A-A was associated with an increased risk of HCC (recessive model; odds ratio=2.277, 95% confidence interval [CI] =1.144-4.532, P=0.019). In the validation population, PTEN rs2299941 G allele was the only significant protective genetic polymorphism related to HCC development after adjustment for age and sex (hazard ratio=0.582, 95% CI =0.353-0.962, P=0.035).
Conclusions
These findings suggest that genetic polymorphisms in PTEN may affect HCC development in patients with chronic HBV infection. -
Citations
Citations to this article as recorded by- Association of genetic variations in phosphatase and tensin homolog (PTEN) gene with polycystic ovary syndrome in South Indian women: a case control study
Swapna Siddamalla, Suresh Govatati, Veena Kunjumol Venu, Nagendram Erram, Mamata Deenadayal, Sisinthy Shivaji, Manjula Bhanoori
Archives of Gynecology and Obstetrics.2020; 302(4): 1033. CrossRef
- Association of genetic variations in phosphatase and tensin homolog (PTEN) gene with polycystic ovary syndrome in South Indian women: a case control study

Case Reports
- Hepatic Failure Due to Hepatitis E Virus Infection in a Patient with Necrotic Hepatocellular Carcinoma
- Ji Hye Kim, Young Seok Doh, Ji Woong Jang, Min Seok Kang, Nak Min Kim, Sae Hee Kim, Il Hyun Baek, Sung Hee Jung
- J Liver Cancer. 2019;19(1):55-58. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.55
- 3,678 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
PDF - In patients with hepatocellular carcinoma (HCC) or liver cirrhosis (LC) accompanied by hepatitis E virus (HEV) infection, hepatic failure often leads to debility. Here, we report about a 63-year-old man with alcoholic LC who was referred to our hospital with jaundice and abdominal distension 10 days earlier. Abdominal computed tomography showed necrotic HCC accompanied by left lobe shrinkage without tumor progression. Laboratory and imaging findings revealed no acute infection focus. The patient reported no herbal medicine or alcohol consumption, and there was no evidence of acute viral hepatitis. One month later, HEV immunoglobulin M positivity was confirmed, and deterioration of liver function due to HEV infection was suspected. The patient often ate raw oysters and sashimi, as well as boar meat, which is a well-known risk food for HEV infection. His umbilical hernia deteriorated due to tense ascites and infection by skin abrasion. The patient progressed to hepatorenal syndrome and eventually died. Liver function preservation is important when treating HCC patients. Therefore, clinicians should pay more attention to the prevention of HEV and others causes of direct liver injury.

- A Case of Spontaneous Rupture of Hepatocellular Carcinoma Supplied by the Right Renal Capsular Artery Treated by Transcatheter Arterial Embolization
- Joo Yeon Jang, Ung Bae Jeon, Jin Hyeok Kim, Tae Un Kim, Hwaseong Ryu, Mong Cho, Young Mi Hong, Maeran Kim
- J Liver Cancer. 2019;19(1):59-63. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.59
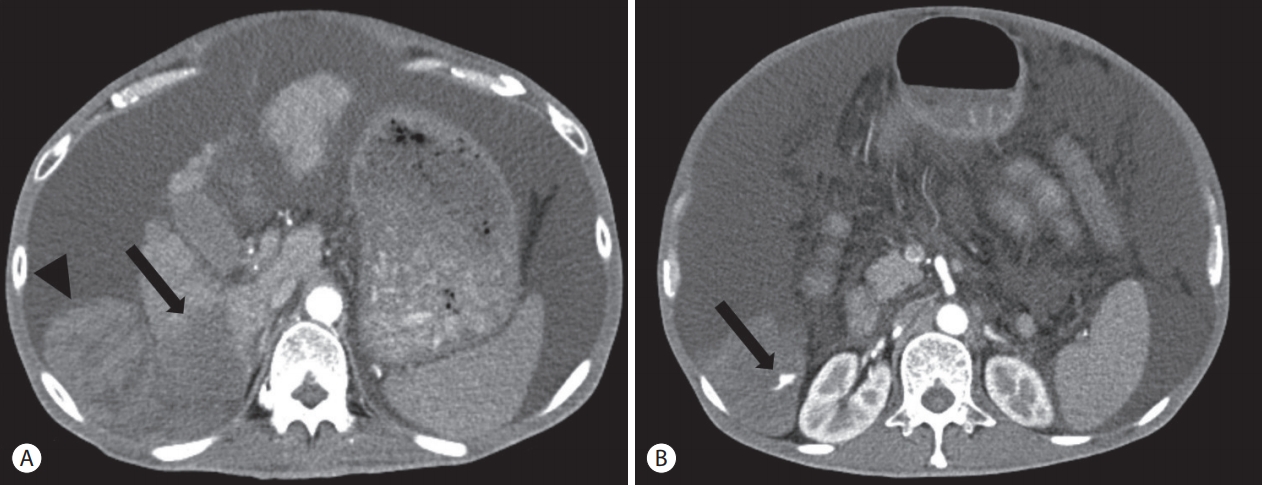
- 5,435 Views
- 92 Downloads
-
 Abstract
Abstract
 PDF
PDF - We present a case of spontaneous rupture of hepatocellular carcinoma with poor liver function managed by transcatheter arterial embolization (TAE). The patient’s bilirubin level was 2.1 mg/dL, albumin level was 2.4 g/dL, and prothrombin time international normalized ratio was 2.1. In addition, the patient had also developed a large number of ascites. The tumor was supplied by the right renal capsular artery, as observed on angiography. With successful TAE, no hepatic failure occurred. We believe TAE can be a safe and effective treatment option, even in patients with poor liver function, if tumors are supplied only by extrahepatic collateral vessels.

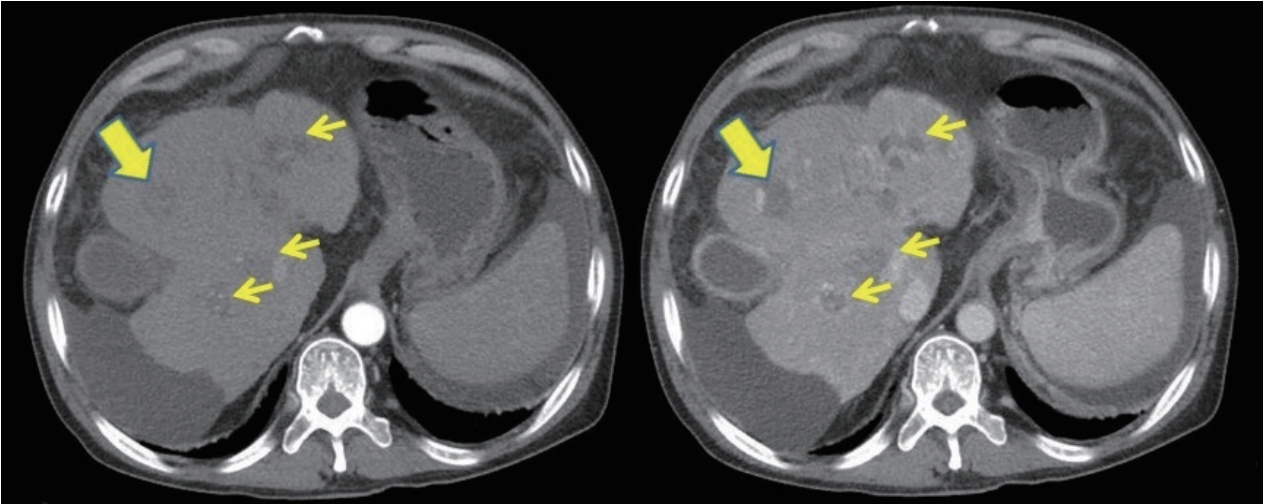
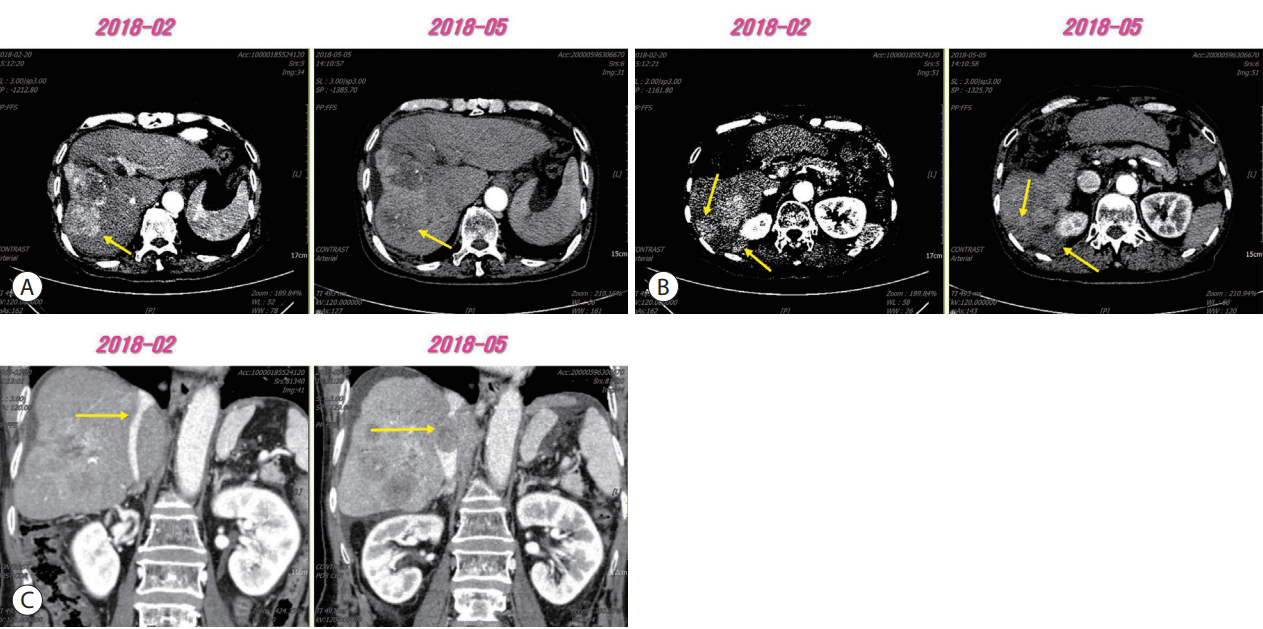
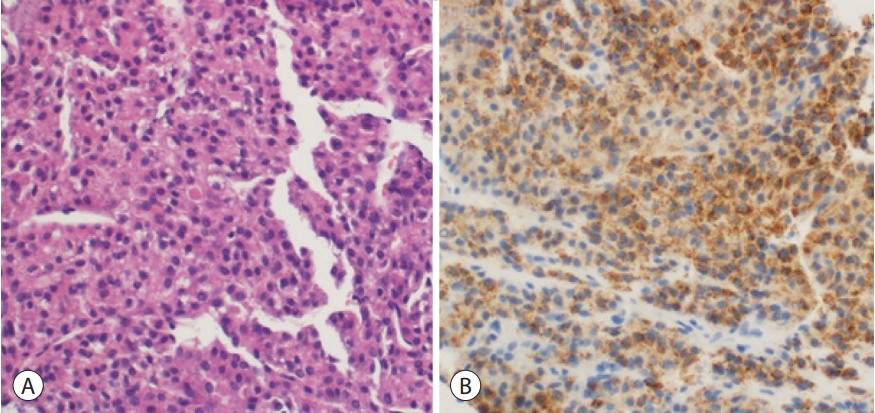
- Liver Transplantation after Successful Downstaging with Hepatic Arterial Infusion Chemotherapy in a Patient with Hepatocellular Carcinoma with Portal Vein Tumor Thrombus
- Hee Chul Nam, Pil Soo Sung, Ho Jong Chun, Dong Goo Kim, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon
- J Liver Cancer. 2019;19(1):64-68. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.64
- 3,544 Views
- 61 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. The majority of patients with HCC are diagnosed at advanced disease stages with vascular invasion, where curative approaches are often not feasible. Currently, sorafenib is the only available standard therapy for HCC with portal vein tumor thrombosis (PVTT). However, in many cases, sorafenib therapy fails to achieve satisfactory results in clinical practice. We present a case of advanced HCC with PVTT that was treated with hepatic arterial infusion chemotherapy (HAIC) followed by liver transplantation. Three cycles of HAIC treatment resulted in necrotic changes in most of the tumors, and PVTT was reduced to an extent at which liver transplantation was possible. Further studies are required to determine the treatment strategies for advanced HCC with PVTT that can improve prognosis.

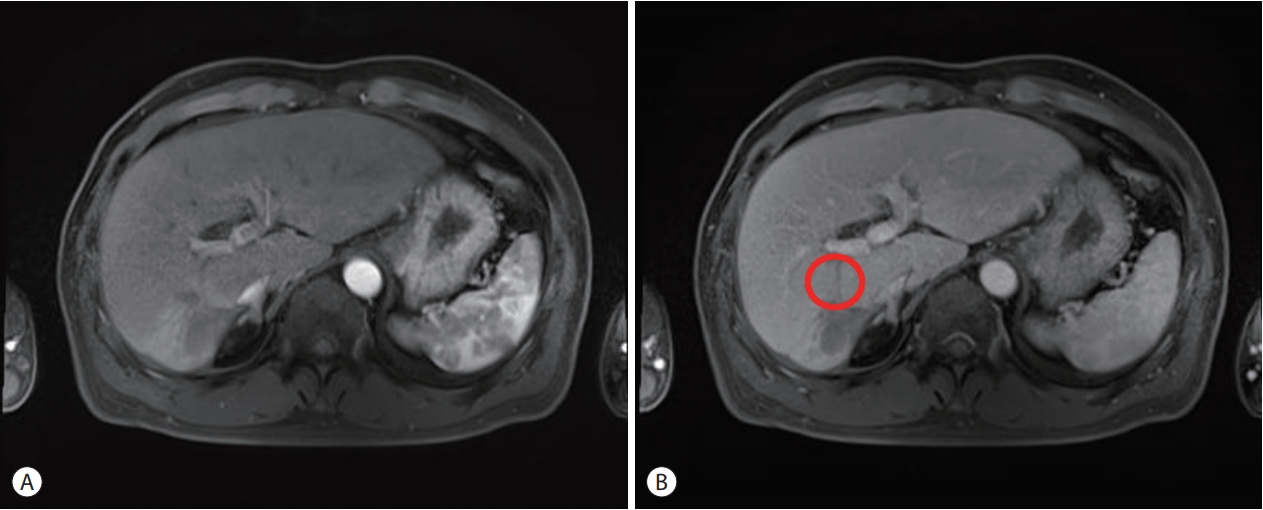
- Gallbladder Fistula Treated with N-Butyl-2-Cyanoacrylate after Radiofrequency Ablation in a Hepatocellular Carcinoma Patient: a Case Report
- In Tae So, Byoung Kook Jang, Jae Seok Hwang, Young hwan Kim
- J Liver Cancer. 2019;19(1):69-73. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.69

- 3,895 Views
- 59 Downloads
-
 Abstract
Abstract
 PDF
PDF - Radiofrequency ablation (RFA) is a minimally invasive local therapy for hepatocellular carcinoma (HCC). Even though RFA is considered to be a safe treatment modality, a variety of complications have been reported. Recently, we encountered a case of refractory fistula between a liver abscess and the gallbladder after RFA. A 64-year-old woman diagnosed with HCC associated with chronic hepatitis B was treated by RFA. After RFA, she experienced abdominal pain, and abdominal computed tomography (CT) revealed a liver abscess complicated by a previous treatment of HCC, she was treated with intravenous antibiotics and percutaneous abscess drainage. Follow-up abdominal CT revealed a fistula between the liver abscess and gallbladder, which was successfully treated with percutaneous transcatheter n-butyl-2-cyanoacrylate (NBCA) embolization. We herein report the rare case of a refractory fistula between a liver abscess and the gallbladder after RFA in a patient treated with NBCA embolization.

- A Case of Achieving Partial Remission with the Combination of Sorafenib and Nivolumab in a Patient with Hepatocellular Carcinoma Showing Disease Progression after Nivolumab Therapy
- Sang Youn Hwang, Seon-Mi Lee, Jung Woo Im, Ki Jeong Jeon, Cheol-Won Choi, Kyung-Su Kim, Wan Jeon
- J Liver Cancer. 2019;19(1):74-78. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.74
- 3,471 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
PDF - Sorafenib is a well-known approved systemic therapeutic agent used in patients with advanced hepatocellular carcinoma (HCC). Regorafenib and nivolumab are approved as second-line therapeutic drugs in patients showing disease progression after sorafenib therapy. However, there is no established third- or fourth-line therapy in patients with progression after regorafenib or nivolumab treatment. Recently, the combination of tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors (ICPIs) has been attempted as a firstline treatment strategy in advanced HCC patients based on the hypothesis that combination therapy may overcome resistance in ICPI monotherapy. On the basis of this suggestion, we herein describe the case of an HCC patient demonstrating macrovascular invasion, whereby partial remission was achieved via the combination of sorafenib and nivolumab following disease progression after nivolumab therapy. Further studies on the combination of TKIs and ICPIs are necessary to determine ways to manage HCC patients showing disease progression after ICPI therapy.

- Combination Therapy of Angiotherapy, Radiation Therapy, and Radiofrequency Ablation for Pulmonary Metastasis of Hepatocellular Carcinoma Accompanied by Nontuberculous Mycobacteria
- Sang Hyun Park, Seul Ki Kim, Ji Hye Kim, Seokgyo Seo, Hyun Pyo Hong, Soo-Youn Ham, Byung Ik Kim
- J Liver Cancer. 2019;19(1):79-84. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.79
- 3,450 Views
- 55 Downloads
-
 Abstract
Abstract
 PDF
PDF - With the advances in hepatocellular carcinoma (HCC) treatment, the lung metastasis of HCC is becoming increasingly important. In treating the lung metastasis of HCC, a multidisciplinary approach can lead to better results than systemic chemotherapy alone. Here, we report on a patient who presented with pulmonary masses, while the HCC was being controlled in the abdominal cavity. The presence of nontuberculous mycobacteria was identified during the diagnosis of the pulmonary masses. The pulmonary metastases of HCC were treated with a combination of angiotherapy, radiation therapy, and radiofrequency ablation. The patient showed a satisfactory progress with this multidisciplinary localized treatment. We report the clinical progress and review the recent literature regarding the treatment of pulmonary metastasis without intrahepatic HCC herein.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION



 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter