Search
- Page Path
- HOME > Search
Review Article
- Multidisciplinary approach for hepatocellular carcinoma patients: current evidence and future perspectives
- Joo Hyun Oh, Dong Hyun Sinn
- J Liver Cancer. 2024;24(1):47-56. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.27

- 593 Views
- 48 Downloads
-
 Abstract
Abstract
 PDF
PDF - Management of hepatocellular carcinoma (HCC) is challenging due to the complex relationship between underlying liver disease, tumor burden, and liver function. HCC is also notorious for its high recurrence rate even after curative treatment for early-stage tumor. Liver transplantation can substantially alter patient prognosis, but donor availability varies by each patient which further complicates treatment decision. Recent advancements in HCC treatments have introduced numerous potentially efficacious treatment modalities. However, high level evidence comparing the risks and benefits of these options is limited. In this complex situation, multidisciplinary approach or multidisciplinary team care has been suggested as a valuable strategy to help cope with escalating complexity in HCC management. Multidisciplinary approach involves collaboration among medical and health care professionals from various academic disciplines to provide comprehensive care. Although evidence suggests that multidisciplinary care can enhance outcomes of HCC patients, robust data from randomized controlled trials are currently lacking. Moreover, the implementation of a multidisciplinary approach necessitates increased medical resources compared to conventional cancer care. This review summarizes the current evidence on the role of multidisciplinary approach in HCC management and explores potential future directions.

Case Reports
- Multidisciplinary approach for hepatocellular carcinoma arising from cirrhotic liver with Budd-Chiari syndrome: a case report
- Sangmi Kim, Ji Hoon Kim, Ji Won Han, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon, Pil Soo Sung
- J Liver Cancer. 2022;22(2):202-206. Published online September 20, 2022
- DOI: https://doi.org/10.17998/jlc.2022.09.17
- 1,896 Views
- 45 Downloads
-
 Abstract
Abstract
 PDF
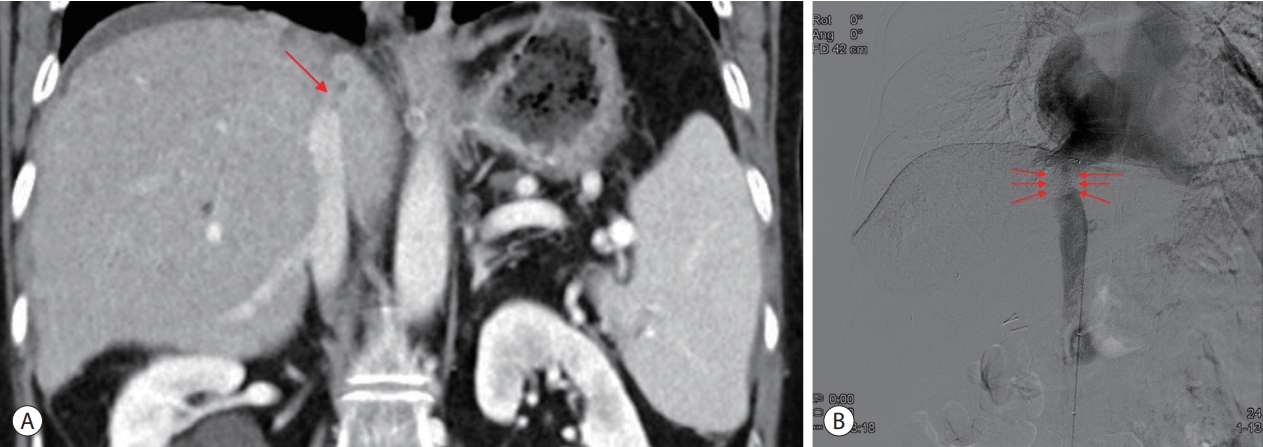
PDF - Budd-Chiari syndrome (BCS) is defined by the obstruction of the hepatic venous outflow between the small hepatic veins and the junction of the inferior vena cava (IVC) with the right atrium. BCS with IVC obstruction occasionally progresses to hepatocellular carcinoma (HCC). Here, we report the case of a patient with HCC arising from a cirrhotic liver with BCS, in whom the hepatic portion of the IVC was obstructed, and who had a favorable outcome with a multidisciplinary approach and IVC balloon angioplasty.

- Multidisciplinary treatment with immune checkpoint inhibitors for advanced stage hepatocellular carcinoma
- Ahlim Lee, Jaejun Lee, Hyun Yang, Soo-Yoon Sung, Chang Ho Jeon, Su Ho Kim, Moon Hyung Choi, Young Joon Lee, Ho Jong Chun, Si Hyun Bae
- J Liver Cancer. 2022;22(1):75-83. Published online March 18, 2022
- DOI: https://doi.org/10.17998/jlc.2022.03.04
- 3,996 Views
- 93 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is a cytotoxic chemotherapy-resistant tumor and most HCCs arise in a background of liver cirrhosis of various causes. Although the IMBrave150 trial showed remarkable advancements in the treatment of unresectable HCC with atezolizumab plus bevacizumab (AteBeva), therapeutic outcomes were unsatisfactory in more than half of the patients. Accordingly, many ongoing trials combine conventional modalities with new drugs such as immune checkpoint inhibitors for better treatment outcomes, and they are expected to benefit patients with limited responses to conventional treatment. Here, two patients with advanced stage HCC with preserved liver function and good performance status showed partial response after treatment with combination or sequential therapy of AteBeva, hepatic arterial infusion chemotherapy, radiation therapy, and transarterial chemoembolization. These findings indicate the efficacy of multidisciplinary treatment against advanced HCC. Additional studies are required to establish optimal treatment strategies.
-
Citations
Citations to this article as recorded by- Complications of immunotherapy in advanced hepatocellular carcinoma
Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
Journal of Liver Cancer.2024; 24(1): 9. CrossRef - Feasibility of additional radiotherapy in patients with advanced hepatocellular carcinoma treated with atezolizumab plus bevacizumab
Tae Hyun Kim, Bo Hyun Kim, Yu Ri Cho, Young-Hwan Koh, Joong-Won Park
Journal of Liver Cancer.2023; 23(2): 330. CrossRef - Is multidisciplinary treatment effective for hepatocellular carcinoma with portal vein tumor thrombus?
Won Hyeok Choe
Journal of Liver Cancer.2022; 22(1): 1. CrossRef
- Complications of immunotherapy in advanced hepatocellular carcinoma

- A Case of Complete Response by Multidisciplinary Management in a Patient with Solitary Bone Metastasis after Curative Resection of Hepatocellular Carcinoma
- Seawon Hwang, Hyun Yang, Hae Lim Lee, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon
- J Liver Cancer. 2016;16(1):52-56. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.52
- 1,022 Views
- 12 Downloads
-
 Abstract
Abstract
 PDF
PDF - Despite recent advances in the treatment of hepatocellular carcinoma (HCC), the prognosis of patients with extrahepatic metastasis from HCC still remains dismal. The current study presents a case of HCC that was metastatic to the pelvis and describes successful treatment with multidisciplinary approach to the skeletal metastasis. The patient was a 67-year-old male who presented with right pelvic pain 28 months following right hepatectomy for HCC. Computed tomography and magnetic resonance imaging indicated a solitary bone metastasis without intrahepatic recurrence. Complete response was achieved with multidisciplinary management including sorafenib, transarterial embolization, surgery to remove the metastatic mass and radiotherapy after surgery. A post-operative follow-up 15 months later found that the patient remained in good health with maintained complete response. This case suggests that a multidisciplinary approach can achieve long-term cancer-free survival and prolonged life expectancy beyond palliative care for patients with solitary bone metastasis after curative surgery for HCC.

Review Article
- Directions for Future Hepatocellular Carcinoma Treatment Guidelines; Hepatologist’s Perspective: Systemic Approach to Multidisciplinary Treatment
- Soo Young Park, Won Young Tak
- Journal of the Korean Liver Cancer Study Group. 2013;13(1):8-13. Published online February 28, 2013
- DOI: https://doi.org/10.17998/jlc.13.1.8
- 963 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma is one of the most important malignancies in Korea with high mortality rates. Although current guidelines define treatment algorithm by performance status, underlying liver function, size and number of hepatocellular carcinoma, those are not fully reflect the complexities of patients’ characteristics and recently advanced available therapeutic options. Treatment can be optimized by available therapeutic options based on the patients’ characteristics. Because of the heterogeneity in presentation among patients, it is now widely accepted that management of hepatocellular carcinoma requires multimodality and multidisciplinary treatment approaches involving hepatologists, surgeons, interventional radiologists, and radiation oncologists. These approaches are important in improving the survival of patients with hepatocellular carcinoma.

Case Report
- A Case of Advanced Hepatocellular Carcinoma Treated with Curative Surgical Resection after Downstaging by Hepatic Arterial Infusion Chemotherapy
- Jong Ryul Eun, Heon Ju Lee, Jae Woon Kim, Jay Chun Chang, Sung Su Yun, Joon Hyuk Choi
- Journal of the Korean Liver Cancer Study Group. 2011;11(1):60-64. Published online February 28, 2011
- 512 Views
- 2 Downloads
-
 Abstract
Abstract
 PDF
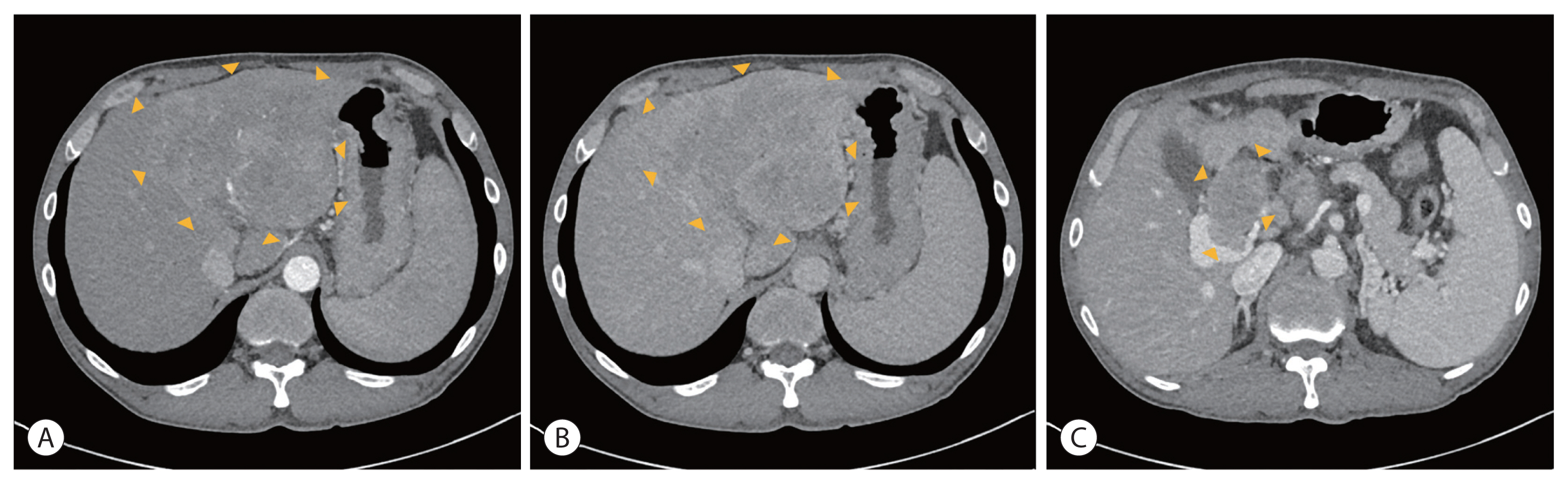
PDF - Cure by single modality for advanced hepatocellular carcinoma (HCC) is difficult. Therefore, multidisciplinary approaches are needed to get a better outcome for advanced HCC. In this paper, we report a case of advanced HCC treated with curative surgical resection after downstaging by hepatic arterial infusion chemotherapy (HAIC). A 50-year-old male patient had a maximum 16.0 cm sized HCC in the right lobe. He achieved a partial response after 2 cycles of HAIC with 5-FU (750 mg/m2) and cisplatin (25 mg/m2). After completion of 6 cycles, he received a curative right hepatectomy and the histopathology revealed 95% of tumor necrosis. He is under follow-up without recurrence at 14 months of surgery. This case suggests that surgery after downstaging by HAIC may provide good clinical outcome in advanced HCC.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter