Search
- Page Path
- HOME > Search
Original Articles
- Outcomes of Liver Resection and Transarterial Chemoembolization in Patients with Multinodular BCLC-A Hepatocellular Carcinoma
- Jiwon Yang, Won-Mook Choi, Danbi Lee, Ju Hyun Shim, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Deok-Bog Moon, Dong-Hwan Jung, Jonggi Choi
- Received March 3, 2024 Accepted March 25, 2024 Published online April 3, 2024
- DOI: https://doi.org/10.17998/jlc.2024.03.25 [Accepted]
- 760 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background
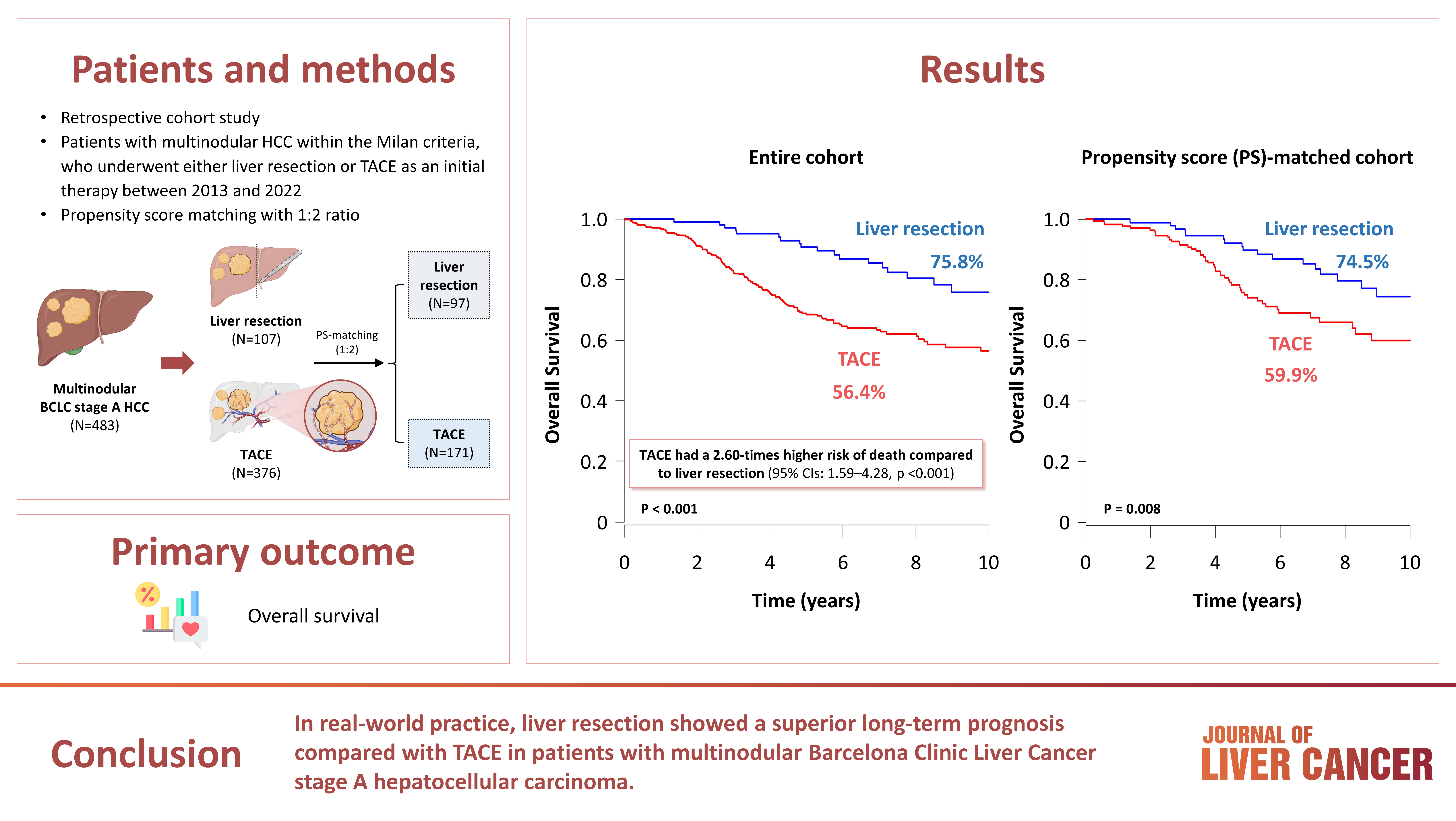
This study aimed to compare the outcomes of liver resection (LR) and transarterial chemoembolization (TACE) in patients with multinodular hepatocellular carcinoma (HCC) within the Milan criteria who were not eligible for liver transplantation.
Methods
We retrospectively analyzed 483 patients with multinodular HCC within the Milan criteria, who underwent either LR or TACE as an initial therapy between 2013 and 2022. The overall survival (OS) in the entire population and recurrence-free survival (RFS) in patients who underwent LR and TACE and achieved a complete response were analyzed. Propensity score (PS) matching analysis was also used for a fair comparison of outcomes between the two groups.
Results
Among the 483 patients, 107 (22.2%) and 376 (77.8%) underwent LR and TACE, respectively. The median size of the largest tumor was 2.0 cm, and 72.3% of the patients had two HCC lesions. The median OS and RFS were significantly longer in the LR group than in the TACE group (p <0.01 for both). In the multivariate analysis, TACE (adjusted hazard ratio [aHR], 1.81 and aHR, 2.41) and large tumor size (aHR, 1.43 and aHR, 1.44) were significantly associated with worse OS and RFS, respectively. The PS-matched analysis also demonstrated that the LR group had significantly longer OS and RFS than the TACE group (PS <0.05).
Conclusion
In this study, LR showed better OS and RFS than TACE in patients with multinodular Barcelona Clinic Liver Cancer stage A HCC. Therefore, LR can be considered an effective treatment option for these patients.

- Subclassification of advanced-stage hepatocellular carcinoma with macrovascular invasion: combined transarterial chemoembolization and radiotherapy as an alternative first-line treatment
- Sujin Jin, Won-Mook Choi, Ju Hyun Shim, Danbi Lee, Kang Mo Kim, Young-Suk Lim, Han Chu Lee, Jinhong Jung, Sang Min Yoon, Jonggi Choi
- J Liver Cancer. 2023;23(1):177-188. Published online March 23, 2023
- DOI: https://doi.org/10.17998/jlc.2023.03.04

- 1,923 Views
- 96 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
The Barcelona Clinic Liver Cancer (BCLC) guidelines recommend systemic therapy as the only first-line treatment for patients with BCLC stage C hepatocellular carcinoma (HCC) despite its heterogeneity of disease extent. We aimed to identify patients who might benefit from combined transarterial chemoembolization (TACE) and radiation therapy (RT) by subclassifying BCLC stage C.
Methods
A total of 1,419 treatment-naïve BCLC stage C patients with macrovascular invasion (MVI) who were treated with combined TACE and RT (n=1,115) or systemic treatment (n=304) were analyzed. The primary outcome was overall survival (OS). Factors associated with OS were identified and assigned points by the Cox model. The patients were subclassified into three groups based on these points.
Results
The mean age was 55.4 years, and 87.8% were male. The median OS was 8.3 months. Multivariate analysis revealed a significant association of Child-Pugh B, infiltrative-type tumor or tumor size ≥10 cm, main or bilateral portal vein invasion, and extrahepatic metastasis with poor OS. The sub-classification was categorized into low (point ≤1), intermediate (point=2), and high (point ≥3) risks based on the sum of points (range, 0–4). The OS in the low, intermediate, and high-risk groups was 22.6, 8.2, and 3.8 months, respectively. In the low and intermediate-risk groups, patients treated with combined TACE and RT exhibited significantly longer OS (24.2 and 9.5 months, respectively) than those who received systemic treatment (6.4 and 5.1 months, respectively; P<0.0001).
Conclusions
Combined TACE and RT may be considered as a first-line treatment option for HCC patients with MVI when classified into low- and intermediate-risk groups. -
Citations
Citations to this article as recorded by- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
Journal of Liver Cancer.2024; 24(1): 102. CrossRef - Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
Journal of Liver Cancer.2024; 24(1): 81. CrossRef - How to optimize the treatment strategy for advanced-stage hepatocellular carcinoma with macrovascular invasion
Beom Kyung Kim
Journal of Liver Cancer.2023; 23(1): 121. CrossRef
- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis

- Transarterial Chemoembolization versus Radiofrequency Ablation for Small Hepatocellular Carcinomas with Discrepant Features on Computed Tomography and Magnetic Resonance Imaging
- Young Youn Cho, Jung Hee Kwon, Jeong-Hoon Lee, Jeong Min Lee, Jae Young Lee, Hyo-Choel Kim, Jin Wook Chung, Won-mook Choi, Eun Ju Cho, Yoon Jun Kim, Jung-Hwan Yoon, Chung Yong Kim, Hyo-Suk Lee
- J Liver Cancer. 2015;15(1):19-29. Published online March 31, 2015
- DOI: https://doi.org/10.17998/jlc.15.1.19
- 1,330 Views
- 10 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aims
This study compared the outcomes of patients with small hepatocellular carcinomas (HCCs) who were treated using transarterial chemoembolization (TACE) or radiofrequency ablation (RFA).
Methods
This was a post-hoc analysis of a prospective study that evaluated the diagnostic efficacy of magnetic resonance imaging (MRI) and computed tomography (CT). We analyzed 41 small hepatic nodules in 32 patients that showed typical radiologic hallmarks on both CT and gadoxate-enhanced MRI (typical nodules) and 25 small hepatic nodules from 22 patients that showed atypical radiologic hallmarks on CT and typical radiologic hallmarks on MRI (discrepant nodules).
Results
There were no significant differences in the baseline characteristics of the patients with typical and discrepant nodules. Complete response rates 1 month after TACE or RFA were 75.0% (18/24) and 94.1% (16/17; P=0.20), respectively, for the patients with typical nodules and 58.8% (10/17) and 100% (8/8; P=0.05), respectively, for the patients with discrepant nodules. Treatment failure rates after TACE or RFA were 33.3% (8/24) and 5.8% (1/17; P=0.15), respectively, for the patients with typical nodules and 47.0% (8/17) and 0.0% (0/8; P=0.02), respectively, for the patients with discrepant nodules. Among patients achieving complete response, there were no significant differences in the risk of marginal recurrence.
Conclusions
RFA provided higher complete response rates and significantly lower treatment failure rates than TACE for patients with discrepant nodules of HCC. Therefore, a treatment modality such as RFA may be preferable for small HCCs which show discrepancy on two imaging modalities.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter