Search
- Page Path
- HOME > Search
Original Article
- Current status of ultrasonography in national cancer surveillance program for hepatocellular carcinoma in South Korea: a large-scale multicenter study
- Sun Hong Yoo, Soon Sun Kim, Sang Gyune Kim, Jung Hyun Kwon, Han-Ah Lee, Yeon Seok Seo, Young Kul Jung, Hyung Joon Yim, Do Seon Song, Seong Hee Kang, Moon Young Kim, Young-Hwan Ahn, Jieun Han, Young Seok Kim, Young Chang, Soung Won Jeong, Jae Young Jang, Jeong-Ju Yoo
- J Liver Cancer. 2023;23(1):189-201. Published online March 24, 2023
- DOI: https://doi.org/10.17998/jlc.2023.03.11
- 2,005 Views
- 71 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
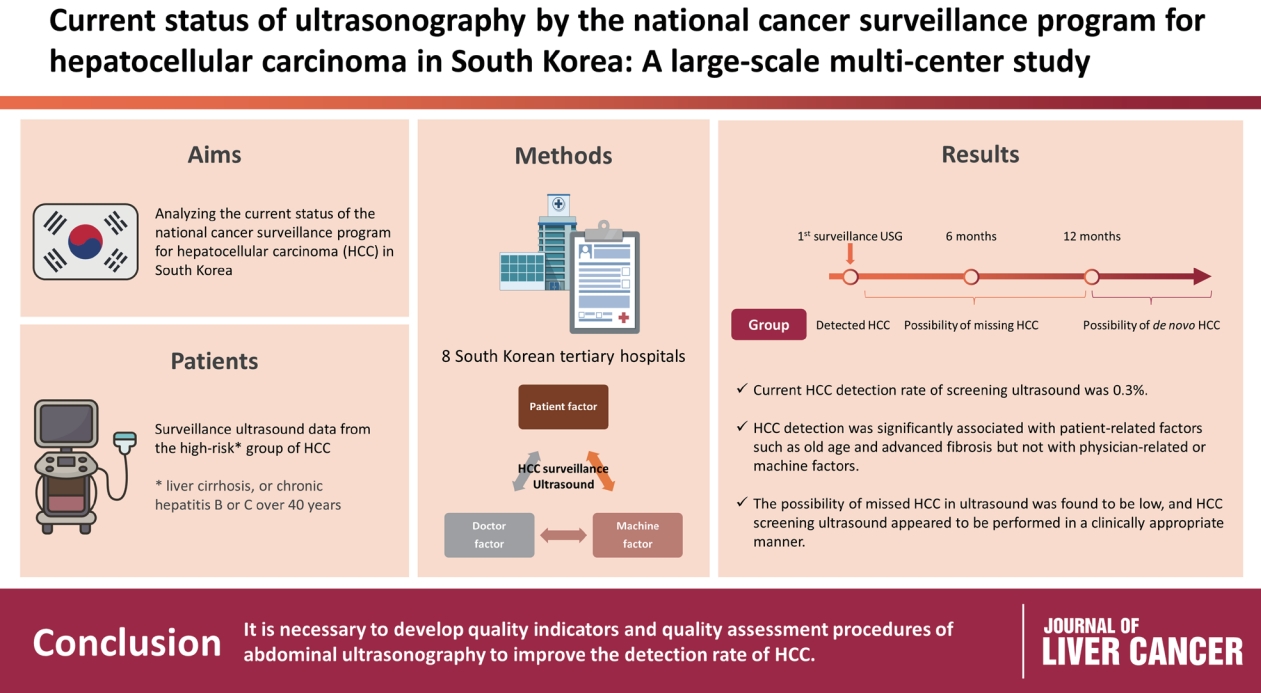
Abdominal ultrasonography (USG) is recommended as a surveillance test for high-risk groups for hepatocellular carcinoma (HCC). This study aimed to analyze the current status of the national cancer surveillance program for HCC in South Korea and investigate the effects of patient-, physician-, and machine-related factors on HCC detection sensitivity.
Methods
This multicenter retrospective cohort study collected surveillance USG data from the high-risk group for HCC (liver cirrhosis or chronic hepatitis B or C >40 years of age) at eight South Korean tertiary hospitals in 2017.
Results
In 2017, 45 experienced hepatologists or radiologists performed 8,512 USG examinations. The physicians had a mean 15.0±8.3 years of experience; more hepatologists (61.4%) than radiologists (38.6%) participated. Each USG scan took a mean 12.2±3.4 minutes. The HCC detection rate by surveillance USG was 0.3% (n=23). Over 27 months of follow-up, an additional 135 patients (0.7%) developed new HCC. The patients were classified into three groups based on timing of HCC diagnosis since the 1st surveillance USG, and no significant intergroup difference in HCC characteristics was noted. HCC detection was significantly associated with patient-related factors, such as old age and advanced fibrosis, but not with physician- or machine-related factors.
Conclusions
This is the first study of the current status of USG as a surveillance method for HCC at tertiary hospitals in South Korea. It is necessary to develop quality indicators and quality assessment procedures for USG to improve the detection rate of HCC. -
Citations
Citations to this article as recorded by- The Epidemiology of Hepatitis B Virus Infection in Korea: 15-Year Analysis
Log Young Kim, Jeong-Ju Yoo, Young Chang, Hoongil Jo, Young Youn Cho, Sangheun Lee, Dong Hyeon Lee, Jae Young Jang
Journal of Korean Medical Science.2024;[Epub] CrossRef - Long-Term HBsAg Titer Kinetics with Entecavir/Tenofovir: Implications for Predicting Functional Cure and Low Levels
Soon Kyu Lee, Soon Woo Nam, Jeong Won Jang, Jung Hyun Kwon
Diagnostics.2024; 14(5): 495. CrossRef
- The Epidemiology of Hepatitis B Virus Infection in Korea: 15-Year Analysis

Case Reports
- Early Intrahepatic Recurrence of Hepatocellular Carcinoma with Metastasis to Lung and Brain after Radiofrequency Ablation
- Jin Dong Kim, Jung Hyun Kwon, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon, Young Jun Lee, Sung Eun Rha, Ho Jong Chun, Byung Gil Choi, Hae Giu Lee
- Journal of the Korean Liver Cancer Study Group. 2009;9(1):37-40. Published online June 30, 2009
- 603 Views
- 2 Downloads
-
 Abstract
Abstract
 PDF
PDF - Radiofrequency ablation (RFA) is the preferred method of local ablation for patients with small (<3 cm sized) hepatocellular carcinoma (HCC) when surgical resection cannot be applied. If RFA procedure is sufficiently completed, it provides lower local tumor recurrence, and longer overall as well as disease-free survival. We experienced a case of early stage HCC which recurred at 2 months after successful RFA procedure, and rapidly metastasized to lung and brain.

- Rapid recurrence following living donor liver transplantation for hepatocellular carcinoma within Milan criteria
- Hyun Young Woo, Jin Dong Kim, Jung Hyun Kwon, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon, Sung Eun Rha, Jae Young Byun, Ho Jong Chun, Byung Gil Choi, Hae Kyu Lee, Young Kyoung You, Dong Gu Kim
- Journal of the Korean Liver Cancer Study Group. 2009;9(1):45-48. Published online June 30, 2009
- 619 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Liver transplantation is curative therapy for hepatocellular carcinoma especially if ,within Milan criteria, 4 year survival and recurrence-free survival was reported to be 85% and 92%, respectively. Herein we report a patient who experience rapid recurrence following living donor liver transplantation (LDLT) for hepatocellular carcinoma within Milan criteria. A 52 year-old-men patient with known liver cirrhosis associated with hepatitis B virus was admitted for the treatment of hepatocellular carcinoma (HCC). Abdominal CT revealed two nodules less than 3 cm in right hepatic lobe. After single session of transcatheter arterial chemoembolization (TACE), the patient underwent LDLT. After seven months following transplantation, recurrent HCC was detected on transplanted liver with concurrent metastatic nodule in lung. Although TACE and metastsectomy were performed for recurrent intrahepatic mass and lung metastasis, recurrent HCC showed rapid progression and patient died of progressive tumor after 10 months following LDLT.

- Treatment of Massive Hepatocellular Carcinoma with Portal Vein Invasion
- Jung Hyun Kwon, Jong Young Choi, Jin Dong Kim, Hyun Young Woo, Si Hyun Bae, Seung Kew Yoon, Young Jun Lee, Ho Jong Chun
- Journal of the Korean Liver Cancer Study Group. 2009;9(1):53-58. Published online June 30, 2009
- 551 Views
- 0 Download
-
 Abstract
Abstract
 PDF
PDF - A 52 year-old-man patient was admitted for evaluation of hepatic mass which was detected on screening ultrasonography. His abdominal CT showed a massive infiltrating mass in left hepatic lobe and another 2.4 cm nodule in S6 of Rt. Hepatic lobe with arterial enhancement and rapid wash out underlying liver cirrhosis. Also, low density tumor thrombus are filled in Lt. portal vein and extended into main portal vein. He was finally diagnosed HCC (UICC stage IVa) with liver cirrhosis (Child-Pugh class A) and hepatitis B. With the four times of trasnarterial chemo-lipiodolization and seven times of intraarterial infusion chemotherapy for huge mass and one time Radiofrequency ablation (RFA) for daughter nodule, his HCC showed no stain in hepatic angiogram at nine month from initial diagnosis. After additional eight times of intra-arterial infusion chemotherapy, new small nodule developed in S6 and was ablated with RFA. At eighteen months after initial diagnosis, he shows no viable lesion on the imaging study and tumor markers are normalized.

- A Case of Advanced Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis Achieving Complete Response with New Therapeutic Modalities
- Hyun Young Woo, Jin Dong Kim, Jung Hyun Kwon, Chan Ran You, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Se Hyun Cho, Seung Kew Yoon, Dong Hoon Lee, Ho Jong Chun, Byung Gil Choi, Chul Seung Kay
- Journal of the Korean Liver Cancer Study Group. 2008;8(1):124-127. Published online June 30, 2008
- 787 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - A 45-year-old man was admitted for the treatment of hepatocellular carcinoma (HCC). He was diagnosed hepatitis B carrier 16 years ago and has not done a routine check. Abdominal CT showed a diffuse infiltrative HCC involving right hepatic lobe with portal vein tumor thrombosis (PVTT) involving right portal vein and proximal portion of left portal vein umbilical portion. With concurrent transcatheter arterial chemotherapy (TAC), helical tomotherapy for portal vein thrombosis was done. With these treatments, main tumor and PVTT was decreased in size markedly and no stain in hepatic angiogram. Due to repeated TAC, hepatic arterial stenosis occurred and TAC was stopped. 3 months after, recurrent tumor was detected in MRI. Radiofrequency ablation followed by High Intensity Focused Ultrasound (HIFU) was done for this recurrent mass. No viable mass was shown in the follow up MRI done 6 months after HIFU.

- Combined hepatocellular and cholangiocarcinoma
- Jung Hyun Kwon, Si Hyun Bae, Jung Pil Suh, Ho Sung Park, Chan Ran You, Jong Young Choi, Seung Kew Yoon, Dong Hoon Lee, Ho Jong Chun, Byung Gil Choi, Chan Kwon Chung, Eun Sun Jung, Mi Ryung Ryu
- Journal of the Korean Liver Cancer Study Group. 2007;7(1):49-54. Published online June 30, 2007
- 620 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - A 43 year-old-women patient was admitted for one month of jaundice. She was diagnosed hepatitis B carrier 17 years ago and has not done a routine check. Abdominal CT showed a large ill defined mass in left hepatic lobe with inhomogenous enhancement in arterial and delayed phase. The result of biopsy including the immunohistochemical stains showed the combined hepatocellular and cholangiocarcinoma (stage IVa, type C by Allen and Lisa). With the radiation therapy (3,910 cGy), six times of transarterial chemo-lipiodolization and two times of percutaneous ethanol injection, huge mass was markedly decreased in size and no stain in hepatic angiogram. She underwent left lobectomy.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter