Search
- Page Path
- HOME > Search
Review Article
- Current perspectives on radiotherapy in hepatocellular carcinoma management: a comprehensive review
- Dowook Kim, Jun-Sang Kim
- J Liver Cancer. 2024;24(1):33-46. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.26
- 714 Views
- 60 Downloads
-
 Abstract
Abstract
 PDF
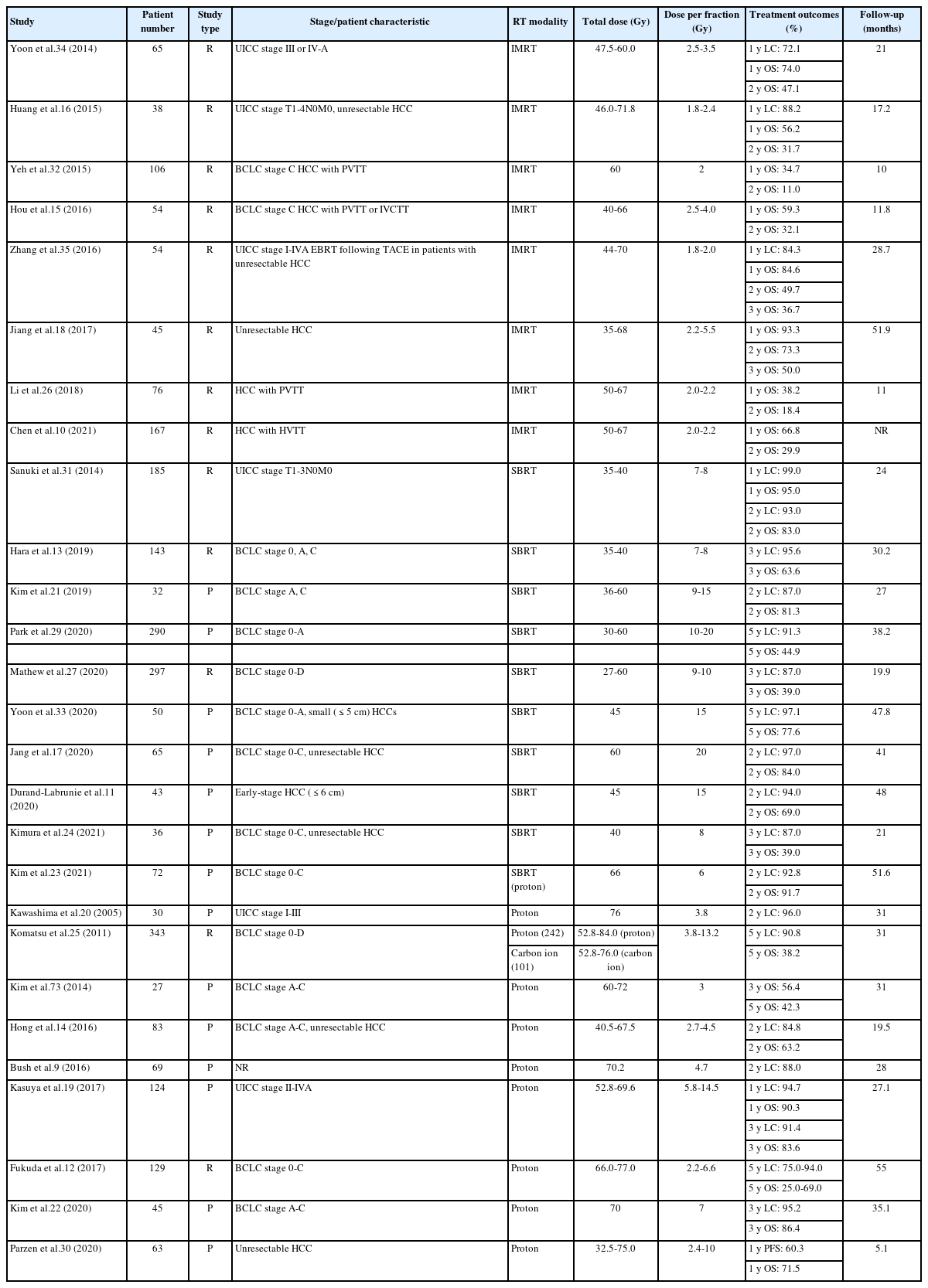
PDF - This review examines the transformative role of external beam radiotherapy (EBRT) in managing hepatocellular carcinoma (HCC), spotlighting the progression from traditional EBRT techniques to advanced modalities like intensity-modulated radiotherapy (RT), stereotactic body RT (SBRT), and innovative particle therapy, including proton beam therapy and carbon ion RT. These advancements have significantly improved the precision and efficacy of RT, marking a paradigm shift in the multimodal management of HCC, particularly in addressing complex cases and enhancing local tumor control. The review underscores the synergistic potential of integrating RT with other treatments like transarterial chemoembolization, systemic therapies such as sorafenib, and emerging immunotherapies, illustrating enhanced survival and disease control outcomes. The efficacy of RT is addressed for challenging conditions, including advanced HCC with macrovascular invasion, and RT modalities, like SBRT, are compared against traditional treatments like radiofrequency ablation for early-stage HCC. Additionally, the review accentuates the encouraging outcomes of particle therapy in enhancing local control and survival rates, minimizing treatment-related toxicity, and advocating for continued research and clinical trials. In conclusion, the integration of RT into multimodal HCC treatment strategies, coupled with the emergence of particle therapy, is crucial for advancing oncologic management, emphasizing the need for relentless innovation and personalized treatment approaches.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION
 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter