Current issue
- Page Path
- HOME > Articles and issues > Current issue
Editorial
- Radiofrequency for hepatocellular carcinoma larger than 3 cm: potential for applications in daily practice
- Ji Hoon Kim, Pil Soo Sung
- J Liver Cancer. 2024;24(1):1-2. Published online March 14, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.13
- 261 Views
- 23 Downloads

Correspondences
- Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
- Jongman Kim
- J Liver Cancer. 2024;24(1):3-4. Published online December 12, 2023
- DOI: https://doi.org/10.17998/jlc.2023.12.04
- 374 Views
- 28 Downloads

- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
- Kazuhiro Nouso, Kazuya Kariyama
- J Liver Cancer. 2024;24(1):5-6. Published online January 19, 2024
- DOI: https://doi.org/10.17998/jlc.2024.01.02
- 341 Views
- 25 Downloads

- Performance of HCC diagnosis in the KLCA-NCC guidelines: a closer look at MRI contrast agents and HCC imaging hallmarks
- Ji Hye Min, Young Kon Kim
- J Liver Cancer. 2024;24(1):7-8. Published online November 6, 2023
- DOI: https://doi.org/10.17998/jlc.2023.10.08
- 477 Views
- 51 Downloads

Review Articles
- Complications of immunotherapy in advanced hepatocellular carcinoma
- Young-Gi Song, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim
- J Liver Cancer. 2024;24(1):9-16. Published online November 29, 2023
- DOI: https://doi.org/10.17998/jlc.2023.11.21
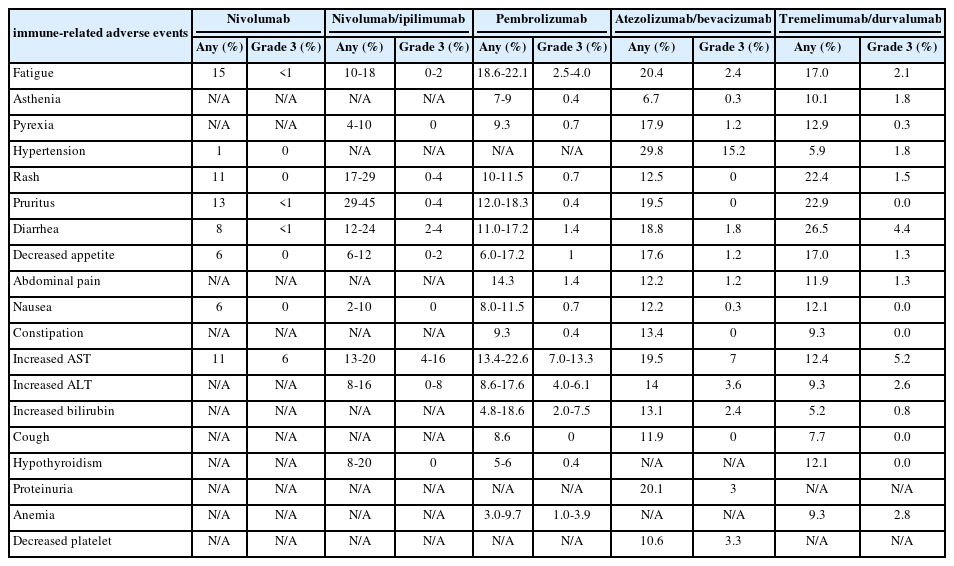
- 983 Views
- 76 Downloads
-
 Abstract
Abstract
 PDF
PDF - Immune checkpoint inhibitors (ICIs) are highly effective in cancer treatment. However, the risks associated with the treatment must be carefully balanced against the therapeutic benefits. Immune-related adverse events (irAEs) are generally unpredictable and may persist over an extended period. In this review, we analyzed common irAEs reported in highly cited original articles and systematic reviews. The prevalent adverse reactions include fatigue, pyrexia, rash, pruritus, diarrhea, decreased appetite, nausea, abdominal pain, constipation, hepatitis, and hypothyroidism. Therefore, it is crucial to conduct evaluations not only of gastrointestinal organs but also of cardiac, neurologic, endocrine (including the frequently affected thyroid), and ophthalmic systems before commencing ICIs. This review further explores commonly reported types of irAEs, specific irAEs associated with each ICI agent, rare yet potentially fatal irAEs, and available treatment options for managing them.

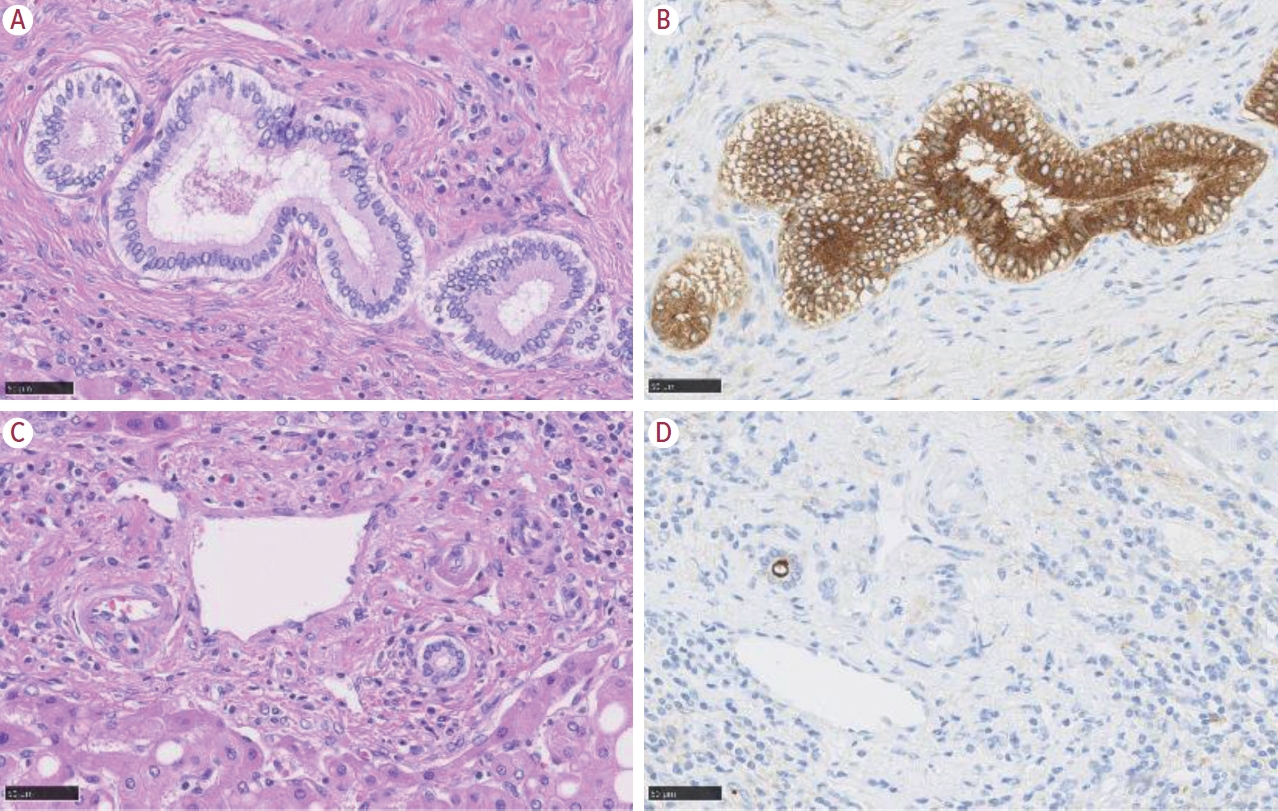
- Intrahepatic cholangiocarcinoma: histological diversity and the role of the pathologist
- Mina Komuta
- J Liver Cancer. 2024;24(1):17-22. Published online January 3, 2024
- DOI: https://doi.org/10.17998/jlc.2023.12.11
- 761 Views
- 95 Downloads
-
 Abstract
Abstract
 PDF
PDF - Intrahepatic cholangiocarcinoma (iCCA) is one of the primary liver cancers and presents with tumor heterogeneity. About 50% of iCCAs comprise actionable mutations, which completely change patient management. In addition, the precise diagnosis of iCCA, including subtype, has become crucial, and pathologists play an important role in this regard. This review focuses on iCCA heterogeneity; looking at different perspectives to guide diagnosis and optimal treatment choice.

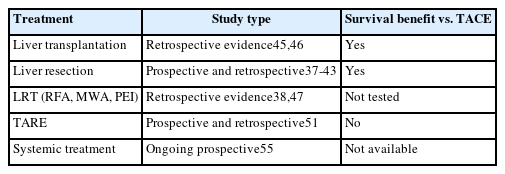
- Intermediate-stage hepatocellular carcinoma: refining substaging or shifting paradigm?
- Bernardo Stefanini, Luca Ielasi, Dante Pio Pallotta, Sofia Penazza, Mariarosaria Marseglia, Fabio Piscaglia
- J Liver Cancer. 2024;24(1):23-32. Published online March 12, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.21
- 583 Views
- 40 Downloads
-
 Abstract
Abstract
 PDF
PDF - This review explores the evolution of cancer staging, focusing on intermediate hepatocellular carcinoma (HCC), and the challenges faced by physicians. The Barcelona Clinic Liver Cancer (BCLC) staging system, introduced in 1999, was designed to address the limitations associated with providing accurate prognostic information for HCC and allocating specific treatments, to avoid overtreatment. However, criticism has emerged, particularly regarding the intermediate stage of HCC (BCLC-B) and its heterogeneous patient population. To overcome this limitation, various subclassification systems, such as the Bolondi and Kinki criteria, have been proposed. These systems are aimed at refining categorizations within the intermediate stage and have demonstrated varying degrees of success in predicting outcomes through external validation. This study discusses the shift in treatment paradigms, emphasizing the need for a more personalized approach rather than strictly adhering to cancer stages, without dismissing the relevance of staging systems. It assesses the available treatment options for intermediate-stage HCC, highlighting the importance of considering surgical and nonsurgical options alongside transarterial chemoembolization for optimal outcomes. In conclusion, the text advocates for a paradigm shift in staging systems prioritizing treatment suitability over cancer stage. This reflects the evolving landscape of HCC management, where a multidisciplinary approach is crucial for tailoring treatments to individual patients, ultimately aiming to improve overall survival.

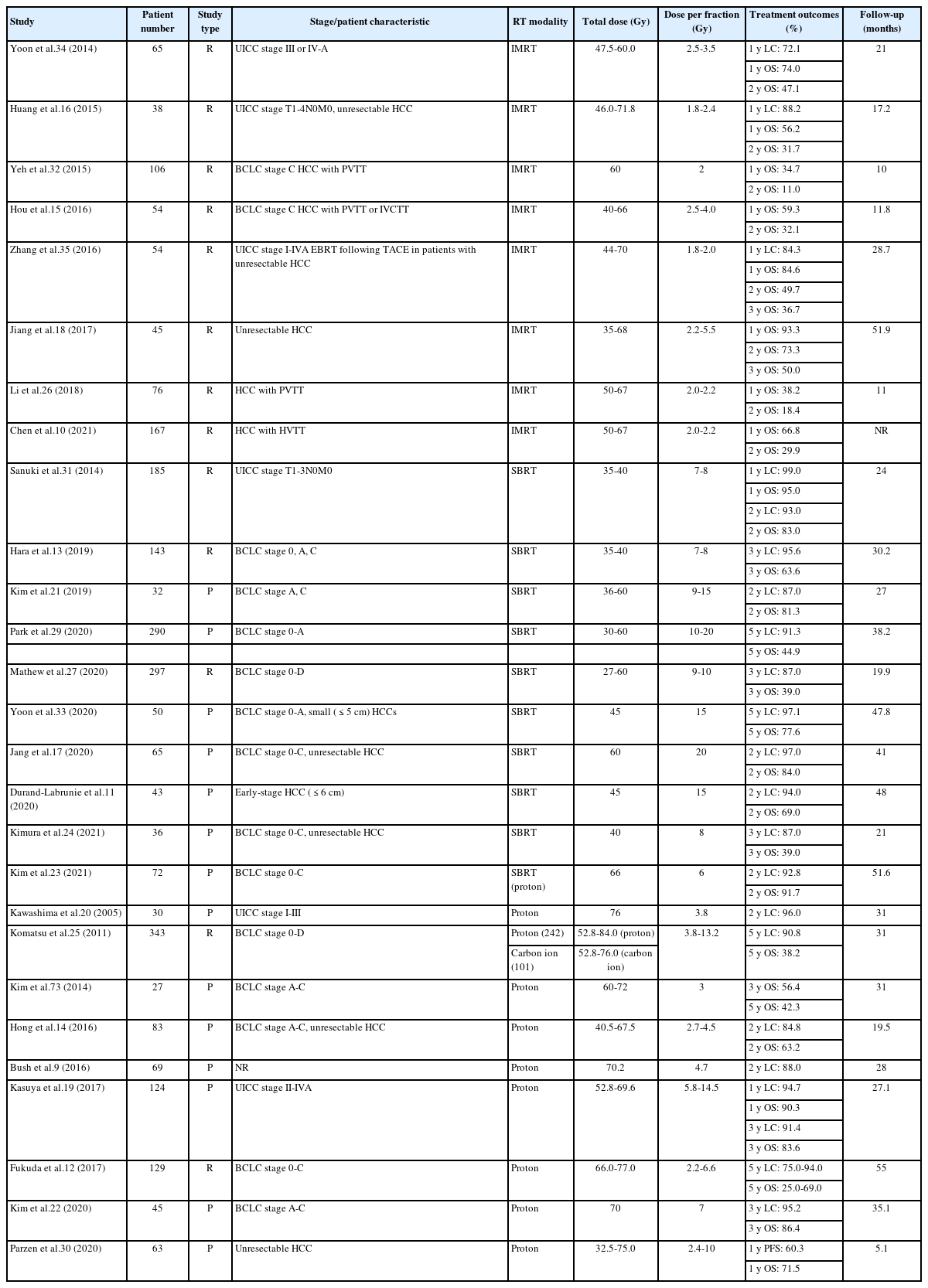
- Current perspectives on radiotherapy in hepatocellular carcinoma management: a comprehensive review
- Dowook Kim, Jun-Sang Kim
- J Liver Cancer. 2024;24(1):33-46. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.26
- 504 Views
- 51 Downloads
-
 Abstract
Abstract
 PDF
PDF - This review examines the transformative role of external beam radiotherapy (EBRT) in managing hepatocellular carcinoma (HCC), spotlighting the progression from traditional EBRT techniques to advanced modalities like intensity-modulated radiotherapy (RT), stereotactic body RT (SBRT), and innovative particle therapy, including proton beam therapy and carbon ion RT. These advancements have significantly improved the precision and efficacy of RT, marking a paradigm shift in the multimodal management of HCC, particularly in addressing complex cases and enhancing local tumor control. The review underscores the synergistic potential of integrating RT with other treatments like transarterial chemoembolization, systemic therapies such as sorafenib, and emerging immunotherapies, illustrating enhanced survival and disease control outcomes. The efficacy of RT is addressed for challenging conditions, including advanced HCC with macrovascular invasion, and RT modalities, like SBRT, are compared against traditional treatments like radiofrequency ablation for early-stage HCC. Additionally, the review accentuates the encouraging outcomes of particle therapy in enhancing local control and survival rates, minimizing treatment-related toxicity, and advocating for continued research and clinical trials. In conclusion, the integration of RT into multimodal HCC treatment strategies, coupled with the emergence of particle therapy, is crucial for advancing oncologic management, emphasizing the need for relentless innovation and personalized treatment approaches.

- Multidisciplinary approach for hepatocellular carcinoma patients: current evidence and future perspectives
- Joo Hyun Oh, Dong Hyun Sinn
- J Liver Cancer. 2024;24(1):47-56. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.02.27

- 526 Views
- 45 Downloads
-
 Abstract
Abstract
 PDF
PDF - Management of hepatocellular carcinoma (HCC) is challenging due to the complex relationship between underlying liver disease, tumor burden, and liver function. HCC is also notorious for its high recurrence rate even after curative treatment for early-stage tumor. Liver transplantation can substantially alter patient prognosis, but donor availability varies by each patient which further complicates treatment decision. Recent advancements in HCC treatments have introduced numerous potentially efficacious treatment modalities. However, high level evidence comparing the risks and benefits of these options is limited. In this complex situation, multidisciplinary approach or multidisciplinary team care has been suggested as a valuable strategy to help cope with escalating complexity in HCC management. Multidisciplinary approach involves collaboration among medical and health care professionals from various academic disciplines to provide comprehensive care. Although evidence suggests that multidisciplinary care can enhance outcomes of HCC patients, robust data from randomized controlled trials are currently lacking. Moreover, the implementation of a multidisciplinary approach necessitates increased medical resources compared to conventional cancer care. This review summarizes the current evidence on the role of multidisciplinary approach in HCC management and explores potential future directions.

- Advancing Korean nationwide registry for hepatocellular carcinoma: a systematic sampling approach utilizing the Korea Central Cancer Registry database
- Bo Hyun Kim, E Hwa Yun, Jeong-Hoon Lee, Geun Hong, Jun Yong Park, Ju Hyun Shim, Eunyang Kim, Hyun-Joo Kong, Kyu-Won Jung, Young-Suk Lim
- J Liver Cancer. 2024;24(1):57-61. Published online March 26, 2024
- DOI: https://doi.org/10.17998/jlc.2024.03.03
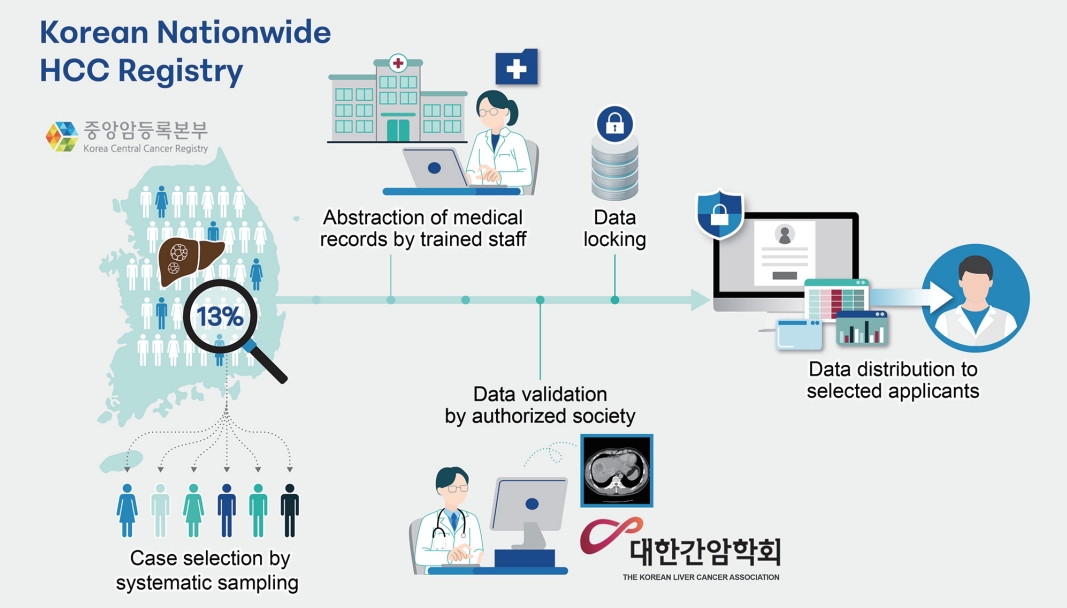
- 346 Views
- 20 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Hepatocellular carcinoma (HCC) presents a substantial public health challenge in South Korea as evidenced by 10,565 new cases annually (incidence rate of 30 per 100,000 individuals), in 2020. Cancer registries play a crucial role in gathering data on incidence, disease attributes, etiology, treatment modalities, outcomes, and informing health policies. The effectiveness of a registry depends on the completeness and accuracy of data. Established in 1999 by the Ministry of Health and Welfare, the Korea Central Cancer Registry (KCCR) is a comprehensive, legally mandated, nationwide registry that captures nearly all incidence and survival data for major cancers, including HCC, in Korea. However, detailed information on cancer staging, specific characteristics, and treatments is lacking. To address this gap, the KCCR, in partnership with the Korean Liver Cancer Association (KLCA), has implemented a systematic approach to collect detailed data on HCC since 2010. This involved random sampling of 10-15% of all new HCC cases diagnosed since 2003. The registry process encompassed four stages: random case selection, meticulous data extraction by trained personnel, expert validation, anonymization of personal data, and data dissemination for research purposes. This random sampling strategy mitigates the biases associated with voluntary reporting and aligns with stringent privacy regulations. This innovative approach positions the KCCR and KLCA as foundations for advancing cancer control and shaping health policies in South Korea.

- Changing etiology and epidemiology of hepatocellular carcinoma: Asia and worldwide
- Do Young Kim
- J Liver Cancer. 2024;24(1):62-70. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.03.13
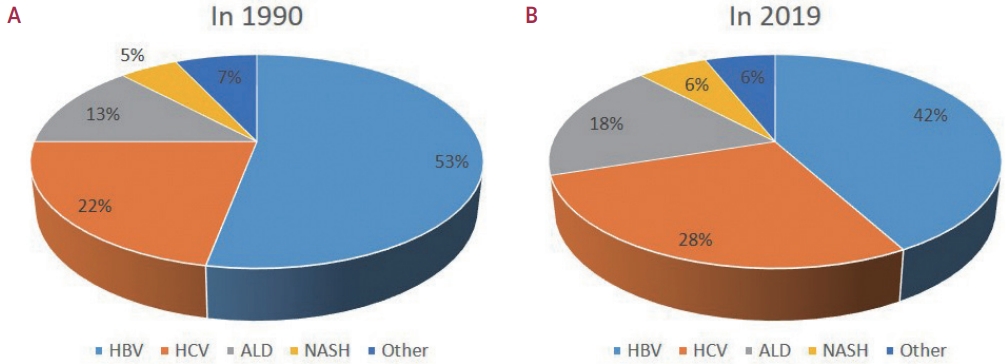
- 730 Views
- 59 Downloads
-
 Abstract
Abstract
 PDF
PDF - Approximately 80% of hepatocellular carcinoma (HCC) cases arise in sub-Saharan Africa and Eastern Asia, following a similarly high prevalence of chronic hepatitis B virus (HBV) carriers in these regions. The etiology and epidemiology of HCC have recently changed worldwide. Although HBV infection is the main contributor to HCC development, a slow but continuous decline in HBV infection rates has been reported since 1990. Owing to the widespread use of direct-acting antivirals, the incidence of hepatitis C virus-related HCC has remarkably decreased in Japan and European countries. In Korea, Taiwan, and Singapore, the incidence of HBV-related HCC has significantly decreased owing to vaccination against HBV. Globally, while HBV accounted for more than half of HCCs in 1990, this had decreased to 42% in 2019. In contrast, the proportion of patients with alcoholic- and nonalcoholic steatohepatitis (NASH) increased from 13% to 18% and from 5% to 6%, respectively. NASH-related HCC has characteristics that differ from those of virus-associated HCC. Compared with other etiologies, patients with NASHassociated HCC are older, have a higher body mass index, and have higher rates of type 2 diabetes mellitus, hypertension, hyperlipidemia, and cardiovascular disease. Nonalcoholic fatty liver disease (NAFLD)-associated HCC is also known to develop in the absence of cirrhosis, unlike alcohol-related and autoimmune liver diseases. Because patients with NAFLD usually have diabetes or obesity, surveying this population is challenging. Optimal selection of the target population and surveillance tools among patients with NAFLD needs to be determined.

Original Articles
- Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study
- Kazuya Kariyama, Kazuhiro Nouso, Atsushi Hiraoka, Hidenori Toyoda, Toshifumi Tada, Kunihiko Tsuji, Toru Ishikawa, Takeshi Hatanaka, Ei Itobayashi, Koichi Takaguchi, Akemi Tsutsui, Atsushi Naganuma, Satoshi Yasuda, Satoru Kakizaki, Akiko Wakuta, Shohei Shiota, Masatoshi Kudo, Takashi Kumada
- J Liver Cancer. 2024;24(1):71-80. Published online November 6, 2023
- DOI: https://doi.org/10.17998/jlc.2023.09.11
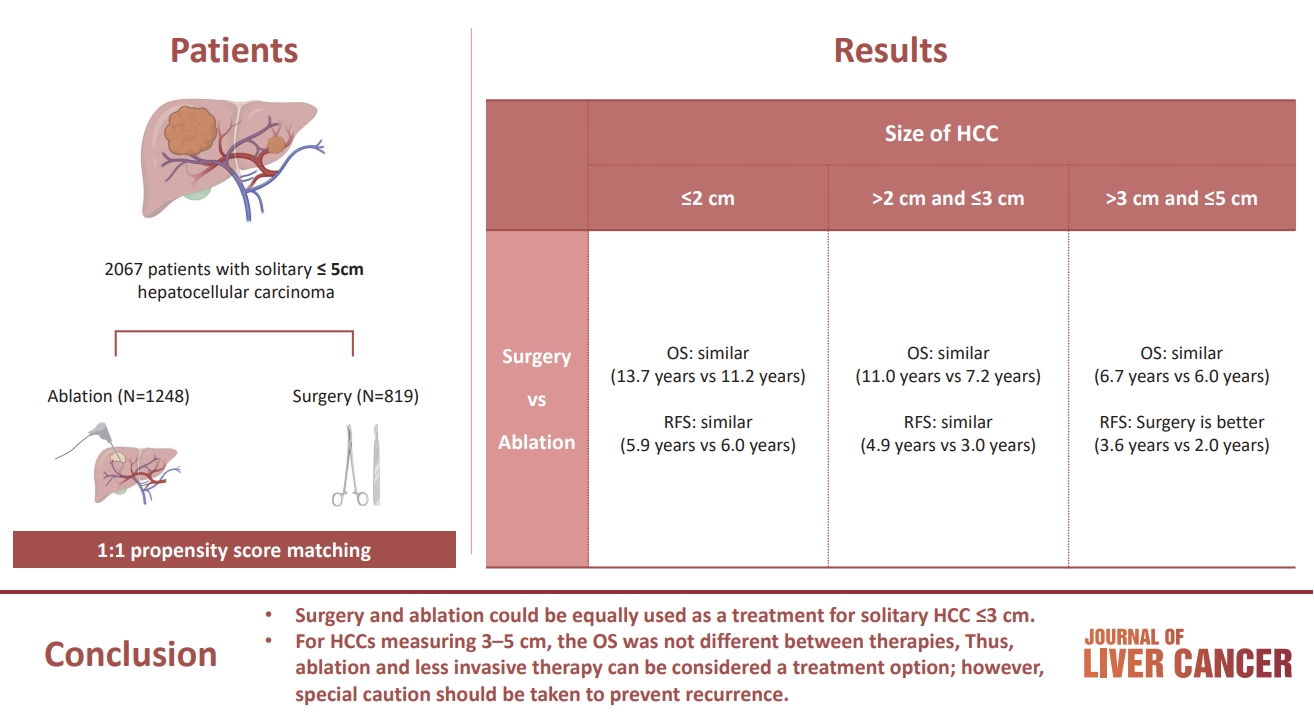
- 929 Views
- 93 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
The aim of this study was to compare the therapeutic efficacy of ablation and surgery in solitary hepatocellular carcinoma (HCC) measuring ≤5 cm with a large HCC cohort database.
Methods
The study included consecutive 2,067 patients with solitary HCC who were treated with either ablation (n=1,248) or surgery (n=819). Th e patients were divided into three groups based on the tumor size and compared the outcomes of the two therapies using propensity score matching.
Results
No significant difference in recurrence-free survival (RFS) or overall survival (OS) was found between surgery and ablation groups for tumors measuring ≤2 cm or >2 cm but ≤3 cm. For tumors measuring >3 cm but ≤5 cm, RFS was significantly better with surgery than with ablation (3.6 and 2.0 years, respectively, P=0.0297). However, no significant difference in OS was found between surgery and ablation in this group (6.7 and 6.0 years, respectively, P=0.668).
Conclusion
The study suggests that surgery and ablation can be equally used as a treatment for solitary HCC no more than 3 cm in diameter. For HCCs measuring 3-5 cm, the OS was not different between therapies; thus, ablation and less invasive therapy can be considered a treatment option; however, special caution should be taken to prevent recurrence. -
Citations
Citations to this article as recorded by- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
Kazuhiro Nouso, Kazuya Kariyama
Journal of Liver Cancer.2024; 24(1): 5. CrossRef - Radiofrequency for hepatocellular carcinoma larger than 3 cm: potential for applications in daily practice
Ji Hoon Kim, Pil Soo Sung
Journal of Liver Cancer.2024; 24(1): 1. CrossRef - Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”
Jongman Kim
Journal of Liver Cancer.2024; 24(1): 3. CrossRef
- Reply to the Letter regarding “Treatment options for solitary hepatocellular carcinoma ≤5 cm: surgery vs. ablation: a multicenter retrospective study”

- Comparison of atezolizumab plus bevacizumab and lenvatinib for hepatocellular carcinoma with portal vein tumor thrombosis
- Jeayeon Park, Yun Bin Lee, Yunmi Ko, Youngsu Park, Hyunjae Shin, Moon Haeng Hur, Min Kyung Park, Dae-Won Lee, Eun Ju Cho, Kyung-Hun Lee, Jeong-Hoon Lee, Su Jong Yu, Tae-Yong Kim, Yoon Jun Kim, Tae-You Kim, Jung-Hwan Yoon
- J Liver Cancer. 2024;24(1):81-91. Published online January 19, 2024
- DOI: https://doi.org/10.17998/jlc.2023.12.25
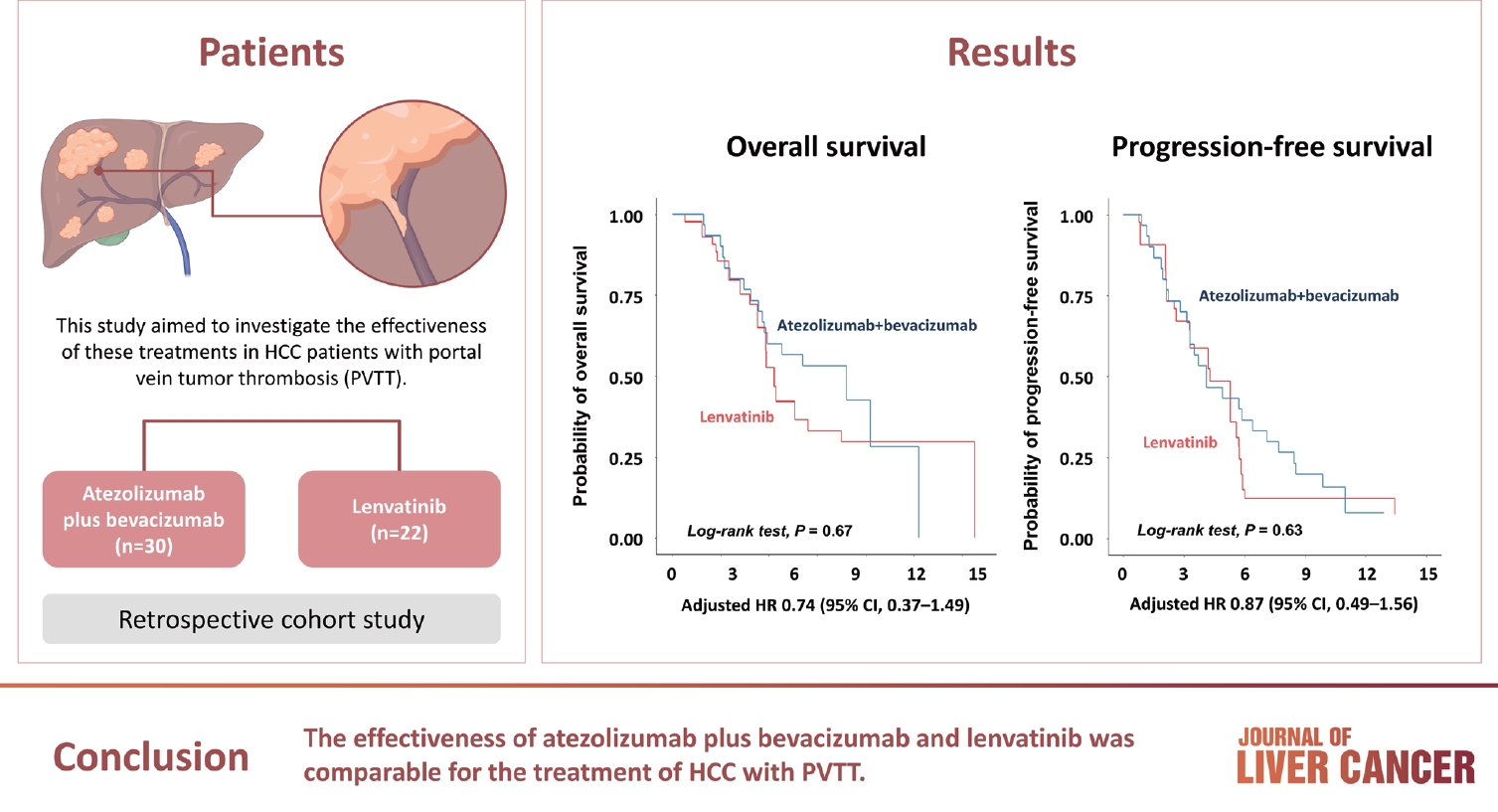
- 992 Views
- 133 Downloads
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background/Aim
Atezolizumab plus bevacizumab and lenvatinib are currently available as first-line therapy for the treatment of unresectable hepatocellular carcinoma (HCC). However, comparative efficacy studies are still limited. This study aimed to investigate the effectiveness of these treatments in HCC patients with portal vein tumor thrombosis (PVTT).
Methods
We retrospectively included patients who received either atezolizumab plus bevacizumab or lenvatinib as first-line systemic therapy for HCC with PVTT. Primary endpoint was overall survival (OS), and secondary endpoints included progressionfree survival (PFS) and disease control rate (DCR) determined by response evaluation criteria in solid tumors, version 1.1.
Results
A total of 52 patients were included: 30 received atezolizumab plus bevacizumab and 22 received lenvatinib. The median follow-up duration was 6.4 months (interquartile range, 3.9-9.8). The median OS was 10.8 months (95% confidence interval [CI], 5.7 to not estimated) with atezolizumab plus bevacizumab and 5.8 months (95% CI, 4.8 to not estimated) with lenvatinib (P=0.26 by log-rank test). There was no statistically significant difference in OS (adjusted hazard ratio [aHR], 0.71; 95% CI, 0.34-1.49; P=0.37). The median PFS was similar (P=0.63 by log-rank test), with 4.1 months (95% CI, 3.3-7.7) for atezolizumab plus bevacizumab and 4.3 months (95% CI, 2.6-5.8) for lenvatinib (aHR, 0.93; 95% CI, 0.51-1.69; P=0.80). HRs were similar after inverse probability treatment weighting. The DCRs were 23.3% and 18.2% in patients receiving atezolizumab plus bevacizumab and lenvatinib, respectively (P=0.74).
Conclusion
The effectiveness of atezolizumab plus bevacizumab and lenvatinib was comparable for the treatment of HCC with PVTT.

- Additional nodules detected using EOB-MRI in patients with resectable single hepatocellular carcinoma: an implication for active treatment strategy
- Na Reum Kim, Seoung Yoon Rho, Jonathan Navarro, Chansik An, Dai Hoon Han, Jin Sub Choi, Myeong-Jin Kim, Gi Hong Choi
- J Liver Cancer. 2024;24(1):92-101. Published online February 14, 2024
- DOI: https://doi.org/10.17998/jlc.2024.01.25
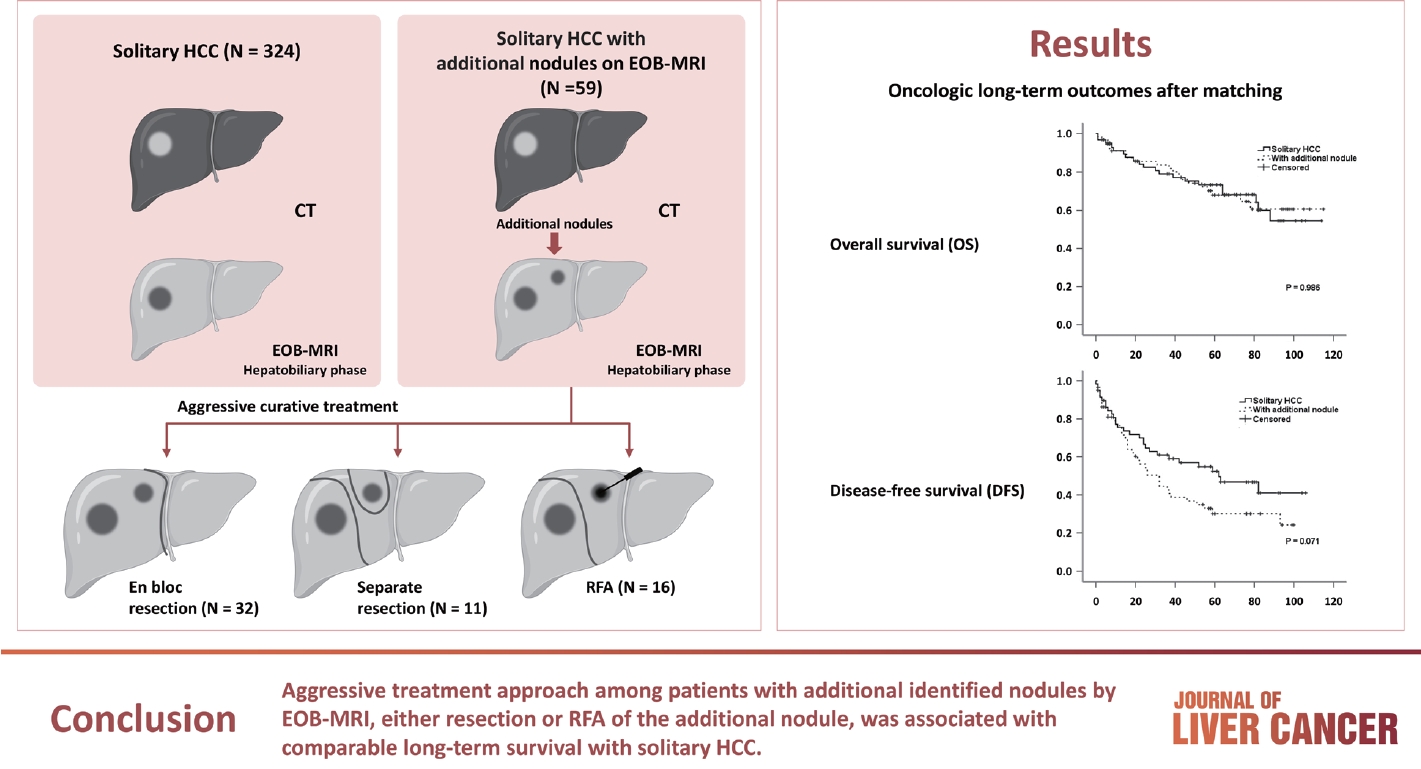
- 728 Views
- 41 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
Gadolinium-ethoxybenzyl-diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging (EOBMRI) further enhances the identification of additional hepatic nodules compared with computed tomography (CT) alone; however, the optimal treatment for such additional nodules remains unclear. We investigated the long-term oncological effect of aggressive treatment strategies for additional lesions identified using EOB-MRI in patients with hepatocellular carcinoma (HCC).
Methods
Data from 522 patients diagnosed with solitary HCC using CT between January 2008 and December 2012 were retrospectively reviewed. Propensity score-matched (PSM) analysis was used to compare the oncologic outcomes between patients with solitary HCC and those with additional nodules on EOB-MRI after aggressive treatment (resection or radiofrequency ablation [RFA]).
Results
Among the 383 patients included, 59 had additional nodules identified using EOB-MRI. Compared with patients with solitary HCC, those with additional nodules on EOB-MRI had elevated total bilirubin, aspartate transaminase, and alanine transaminase; had a lower platelet count, higher MELD score, and highly associated with liver cirrhosis (P<0.05). Regarding long-term outcomes, 59 patients with solitary HCC and those with additional nodules after PSM were compared. Disease-free survival (DFS) and overall survival (OS) were comparable between the two groups (DFS, 60.4 vs. 44.3 months, P=0.071; OS, 82.8 vs. 84.8 months, P=0.986).
Conclusion
The aggressive treatment approach, either resection or RFA, for patients with additional nodules identified on EOBMRI was associated with long-term survival comparable with that for solitary HCC. However, further studies are required to confirm these findings.

- Liver resection in selective hepatocellular carcinoma with Vp3 or Vp4 portal vein tumor thrombosis improves prognosis
- Manuel Lim, Jongman Kim, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh
- J Liver Cancer. 2024;24(1):102-112. Published online February 14, 2024
- DOI: https://doi.org/10.17998/jlc.2024.01.31
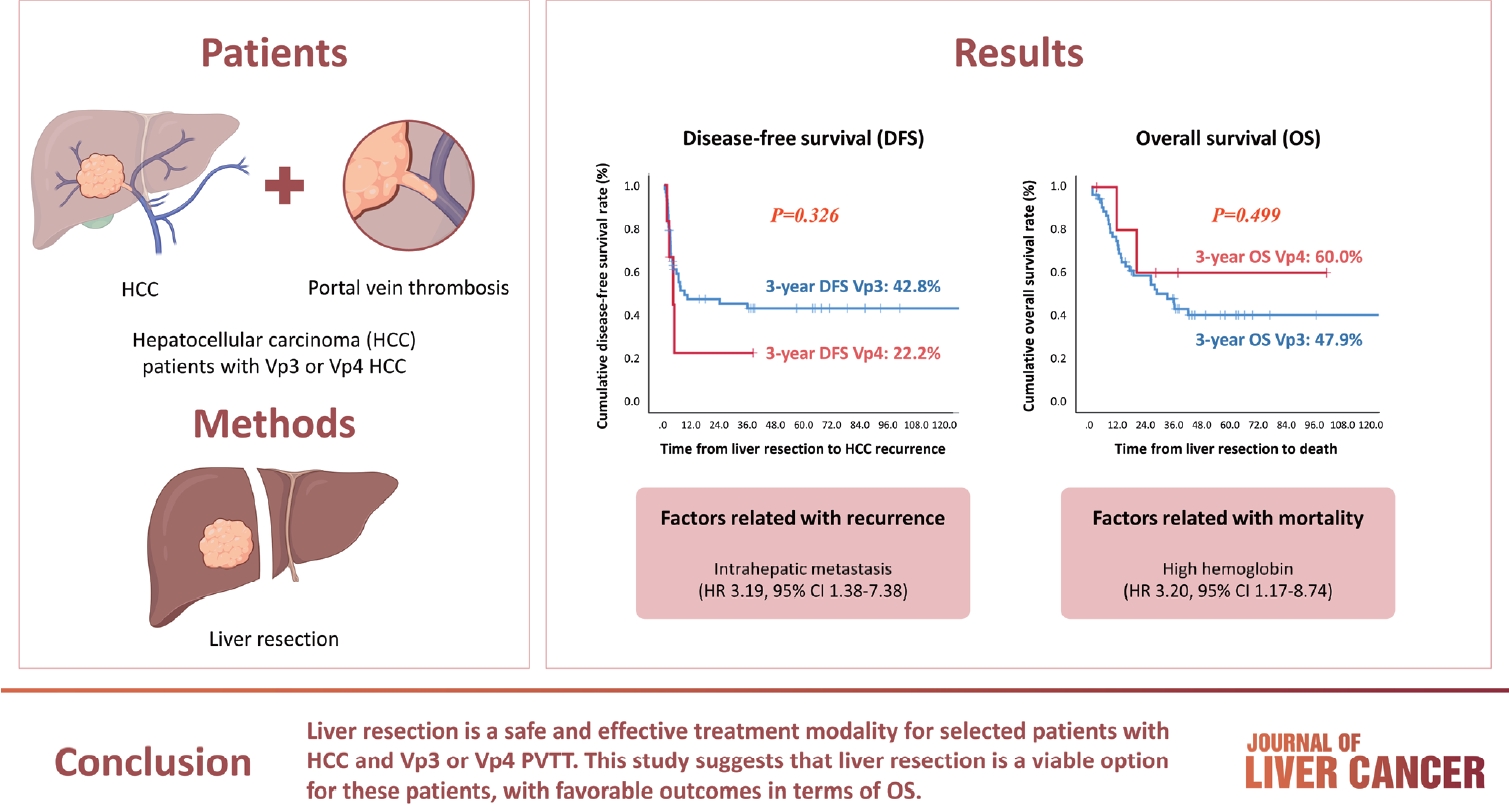
- 405 Views
- 38 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
Hepatocellular carcinoma (HCC) tumor thrombi located in the first branch of the portal vein (Vp3) or in the main portal trunk (Vp4) are associated with poor prognosis. This study aimed to investigate the clinicopathological characteristics and risk factors for HCC recurrence and mortality following liver resection (LR) in patients with Vp3 or Vp4 HCC.
Methods
The study included 64 patients who underwent LR for HCC with Vp3 or Vp4 portal vein tumor thrombosis (PVTT).
Results
Fifty-eight patients (90.6%) had Vp3 PVTT, whereas the remaining six patients exhibited Vp4 PVTT. The median tumor size measured 8 cm, with approximately 36% of patients presented with multiple tumors. Fifty-four patients (84.4%) underwent open LR, whereas 10 patients underwent laparoscopic LR. In the Vp4 cases, combined LR and tumor thrombectomy were performed. The 3-year cumulative disease-free survival rate was 42.8% for the Vp3 group and 22.2% for the Vp4 group. The overall survival (OS) rate at 3 years was 47.9% for the Vp3 group and 60.0% for the Vp4 group. Intrahepatic metastasis has been identified as an important contributor to HCC recurrence. High hemoglobin levels are associated with high mortality.
Conclusion
LR is a safe and effective treatment modality for selected patients with Vp3 or Vp4 HCC PVTT. This suggests that LR is a viable option for these patients, with favorable outcomes in terms of OS.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION



 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter