Search
- Page Path
- HOME > Search
Review Articles
- Recent updates on the classification of hepatoblastoma according to the International Pediatric Liver Tumors Consensus
- Se Un Jeong, Hyo Jeong Kang
- J Liver Cancer. 2022;22(1):23-29. Published online March 17, 2022
- DOI: https://doi.org/10.17998/jlc.2022.02.24
- 5,516 Views
- 476 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Hepatoblastoma is the most common pediatric liver malignancy and usually occurs within the first 3 years of life. In recent years, the overall incidence of hepatoblastoma has exhibited the greatest increase among all pediatric malignancies worldwide. The diagnosis of hepatoblastoma may be challenging due to the lack of a current consensus classification system. The International Pediatric Liver Tumors Consensus introduced guidelines and a consensus classification for the diagnosis of hepatoblastoma as either epithelial or mixed epithelial and mesenchymal and in the updated 5th edition of the World Health Organization Classification of Digestive System Tumors.
-
Citations
Citations to this article as recorded by- Adult hepatoblastoma: making the challenging distinction from hepatocellular carcinoma
Allison Kaye L. Pagarigan, Paulo Giovanni L. Mendoza
Journal of Liver Cancer.2023; 23(1): 219. CrossRef - Advances in Histological and Molecular Classification of Hepatocellular Carcinoma
Joon Hyuk Choi, Swan N. Thung
Biomedicines.2023; 11(9): 2582. CrossRef
- Adult hepatoblastoma: making the challenging distinction from hepatocellular carcinoma

- Histopathological Variants of Hepatocellular Carcinomas: an Update According to the 5th Edition of the WHO Classification of Digestive System Tumors
- Haeryoung Kim, Mi Jang, Young Nyun Park
- J Liver Cancer. 2020;20(1):17-24. Published online March 31, 2020
- DOI: https://doi.org/10.17998/jlc.20.1.17
- 14,250 Views
- 1,004 Downloads
- 27 Citations
-
 Abstract
Abstract
 PDF
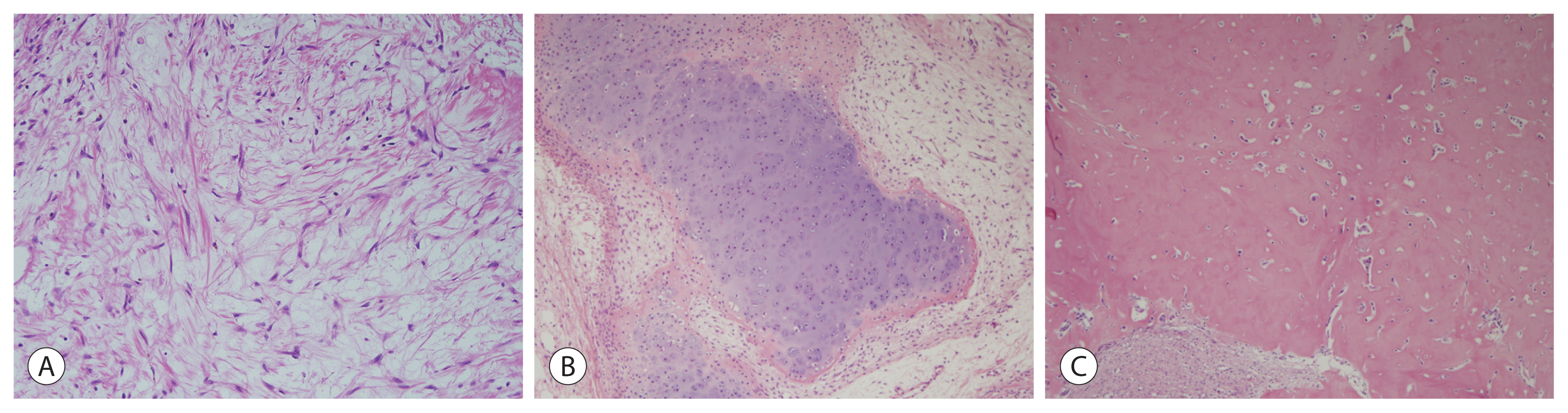
PDF - Hepatocellular carcinoma (HCC) is heterogeneous in pathogenesis, phenotype and biological behavior. Various histopathological features of HCC had been sporadically described, and with the identification of common molecular alterations of HCC and its genomic landscape over the last decade, morpho-molecular correlation of HCC has become possible. As a result, up to 35% of HCCs can now be classified into histopathological variants, many of which have unique molecular characteristics. This review will provide an introduction to the variously described histopathological variants of HCC in the updated WHO Classification of Digestive System Tumors.
-
Citations
Citations to this article as recorded by- Computational pathology: A survey review and the way forward
Mahdi S. Hosseini, Babak Ehteshami Bejnordi, Vincent Quoc-Huy Trinh, Lyndon Chan, Danial Hasan, Xingwen Li, Stephen Yang, Taehyo Kim, Haochen Zhang, Theodore Wu, Kajanan Chinniah, Sina Maghsoudlou, Ryan Zhang, Jiadai Zhu, Samir Khaki, Andrei Buin, Fatemeh
Journal of Pathology Informatics.2024; 15: 100357. CrossRef - Characterization of lymphocyte‐rich hepatocellular carcinoma and the prognostic role of tertiary lymphoid structures
Bokyung Ahn, Hee‐Sung Ahn, Jinho Shin, Eunsung Jun, Eun‐Young Koh, Yeon‐Mi Ryu, Sang‐Yeob Kim, Chang Ohk Sung, Ju Hyun Shim, JeongYeon Hong, Kyunggon Kim, Hyo Jeong Kang
Liver International.2024; 44(5): 1202. CrossRef - Clinical‐Radiologic Morphology‐Radiomics Model on Gadobenate Dimeglumine‐Enhanced MRI for Identification of Highly Aggressive Hepatocellular Carcinoma: Temporal Validation and Multiscanner Validation
Wanjing Zheng, Xiaodan Chen, Meilian Xiong, Yu Zhang, Yang Song, Dairong Cao
Journal of Magnetic Resonance Imaging.2024;[Epub] CrossRef - Diagnostic Model for Proliferative HCC Using LI‐RADS: Assessing Therapeutic Outcomes in Hepatectomy and TKI‐ICI Combination
Mengtian Lu, Zuyi Yan, Qi Qu, Guodong Zhu, Lei Xu, Maotong Liu, Jifeng Jiang, Chunyan Gu, Ying Chen, Tao Zhang, Xueqin Zhang
Journal of Magnetic Resonance Imaging.2024;[Epub] CrossRef - Low-Baseline PD1+ Granulocytes Predict Responses to Atezolizumab–Bevacizumab in Hepatocellular Carcinoma
Catia Giovannini, Fabrizia Suzzi, Francesco Tovoli, Mariangela Bruccoleri, Mariarosaria Marseglia, Eleonora Alimenti, Francesca Fornari, Massimo Iavarone, Fabio Piscaglia, Laura Gramantieri
Cancers.2023; 15(6): 1661. CrossRef - Non-alcoholic fatty liver disease: the pathologist’s perspective
Wei-Qiang Leow, Anthony Wing-Hung Chan, Paulo Giovanni L. Mendoza, Regina Lo, Kihan Yap, Haeryoung Kim
Clinical and Molecular Hepatology.2023; 29(Suppl): S302. CrossRef - 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
Journal of Liver Cancer.2023; 23(1): 1. CrossRef - Three-dimensional multifrequency magnetic resonance elastography improves preoperative assessment of proliferative hepatocellular carcinoma
Guixue Liu, Di Ma, Huafeng Wang, Jiahao Zhou, Zhehan Shen, Yuchen Yang, Yongjun Chen, Ingolf Sack, Jing Guo, Ruokun Li, Fuhua Yan
Insights into Imaging.2023;[Epub] CrossRef - Lymphocyte-Rich Hepatocellular Carcinoma with Multiple Lymphadenopathy and Positive Epstein–Barr Virus Encoding Region
Pin-Yi Wang, Yu-Hsuan Kuo, Ming-Jen Sheu, Hsing-Tao Kuo, Wen-Ying Lee, Yu-Ting Kuo, Su-Hung Wang, Zu-Yau Lin
Case Reports in Hepatology.2023; 2023: 1. CrossRef - Genome-Wide Extrachromosomal Circular DNA Profiling of Paired Hepatocellular Carcinoma and Adjacent Liver Tissues
Jianyu Ye, Peixin Huang, Kewei Ma, Zixin Zhao, Ting Hua, Wenjing Zai, Jieliang Chen, Xiutao Fu
Cancers.2023; 15(22): 5309. CrossRef - Proliferative hepatocellular carcinomas in cirrhosis: patient outcomes of LI-RADS category 4/5 and category M
Subin Heo, Hyo Jeong Kang, Sang Hyun Choi, Sehee Kim, Youngeun Yoo, Won-Mook Choi, So Yeon Kim, Seung Soo Lee
European Radiology.2023;[Epub] CrossRef - Cellular heterogeneity and plasticity in liver cancer
Lo-Kong Chan, Yu-Man Tsui, Daniel Wai-Hung Ho, Irene Oi-Lin Ng
Seminars in Cancer Biology.2022; 82: 134. CrossRef - MRI features of histologic subtypes of hepatocellular carcinoma: correlation with histologic, genetic, and molecular biologic classification
Ja Kyung Yoon, Jin-Young Choi, Hyungjin Rhee, Young Nyun Park
European Radiology.2022; 32(8): 5119. CrossRef - Variant Hepatocellular Carcinoma Subtypes According to the 2019 WHO Classification: An Imaging-Focused Review
Liang Meng Loy, Hsien Min Low, Jin-Young Choi, Hyungjin Rhee, Chin Fong Wong, Cher Heng Tan
American Journal of Roentgenology.2022; 219(2): 212. CrossRef - Paraneoplastic syndromes in hepatocellular carcinoma: a review
Yuki Ong, Cheong Wei Terence Huey, Vishalkumar Girishchandra Shelat
Expert Review of Gastroenterology & Hepatology.2022; 16(5): 449. CrossRef - Morphomolecular Classification Update on Hepatocellular Adenoma, Hepatocellular Carcinoma, and Intrahepatic Cholangiocarcinoma
Venkata S. Katabathina, Lokesh Khanna, Venkateswar R. Surabhi, Marta Minervini, Krishna Shanbhogue, Anil K. Dasyam, Srinivasa R. Prasad
RadioGraphics.2022; 42(5): 1338. CrossRef - 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma
Clinical and Molecular Hepatology.2022; 28(4): 583. CrossRef - 2022 KLCA-NCC Korea Practice Guidelines for the Management of Hepatocellular Carcinoma
Korean Journal of Radiology.2022; 23(12): 1126. CrossRef - Histomorphological Subtypes of Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma: Review and Update
Yoon Jung Hwang, Haeryoung Kim
AJSP: Reviews and Reports.2022; 27(6): 234. CrossRef - Pediatric Primary Hepatic Tumors: Diagnostic Considerations
Bryony Lucas, Sanjita Ravishankar, Irina Pateva
Diagnostics.2021; 11(2): 333. CrossRef - A Case of Lymphocyte-Rich Hepatocellular Carcinoma in a Patient Who Was Treated for Colon Cancer
Jae Won Song, Ho Soo Chun, Jae Seung Lee, Hye Won Lee, Beom Kyung Kim, Seung Up Kim, Jun Yong Park, Sang Hoon Ahn, Young Nyun Park, Dai Hoon Han, Do Young Kim
Journal of Liver Cancer.2021; 21(1): 69. CrossRef - HCC You Cannot See
Vaishnavi Boppana, Sakshi Sahni, Joseph Glass, Christopher Chang, Denis M McCarthy
Digestive Diseases and Sciences.2021; 66(7): 2185. CrossRef - An update on subtypes of hepatocellular carcinoma: From morphology to molecular
Monika Vyas, Dhanpat Jain
Indian Journal of Pathology and Microbiology.2021; 64(5): 112. CrossRef - HCC: role of pre- and post-treatment tumor biology in driving adverse outcomes and rare responses to therapy
Sandeep Arora, Roberta Catania, Amir Borhani, Natally Horvat, Kathryn Fowler, Carla Harmath
Abdominal Radiology.2021; 46(8): 3686. CrossRef - Gadoxetate-enhanced MRI Features of Proliferative Hepatocellular Carcinoma Are Prognostic after Surgery
Hyo-Jin Kang, Haeryoung Kim, Dong Ho Lee, Bo Yun Hur, Yoon Jung Hwang, Kyung-Suk Suh, Joon Koo Han
Radiology.2021; 300(3): 572. CrossRef - Radiologic Diagnosis of Hepatocellular Carcinoma
Woo Kyoung Jeong
The Korean Journal of Gastroenterology.2021; 78(5): 261. CrossRef - Update on Hepatocellular Carcinoma: a Brief Review from Pathologist Standpoint
Nese Karadag Soylu
Journal of Gastrointestinal Cancer.2020; 51(4): 1176. CrossRef
- Computational pathology: A survey review and the way forward

- Evaluation of the Outcome after Transarterial Chemoembolization; Refinement of Barcelona Clinic Liver Cancer Stage-B from Eastern Point of View
- Namiki Izumi
- J Liver Cancer. 2016;16(1):7-11. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.7
- 1,268 Views
- 10 Downloads
-
 Abstract
Abstract
 PDF
PDF - Transarterial chemoembolization (TACE) is recommended as the first line treatment option for the patients with Barcelona Clinic Liver Cancer (BCLC) stage B hepatocellular carcinoma (HCC), however, treatment strategy and evaluation of effects after TACE has not been fully established. Recently, sub-stage of BCLC stage B has been proposed and validated, but it should be validated including a large number of the patients and its refinement should be discussed. We have validated the sub-stage of BCLC stage B (B1-B4) by comparing overall survival after TACE, and there was no statistically significant difference in overall survival after TACE between B1 and B2. After excluding the patients with Child-Pugh point 7 from B1, the overall survival was significantly better than that of B2. Therefore, up-to-seven criteria is shown to be a reliable tool for the treatment strategy in the patients with intermediate stage of HCC. Refinement of sub-stage of BCLC stage B has been proposed by some other institutes, and it is important to establish novel treatment strategy for the patients with BCLC stage B after TACE to improve the prognosis of the patients after TACE, and to define the best timing for conversion to sorafenib or liver transplantation should be discussed. (J Liver Cancer 2016;16:7-11)

Case Report
- A Case of Rapid Progressive Extrahepatic Metastasis of Hepatocellular Carcinoma after Surgical Resection for Huge Single Mass
- Eun Sun Jang, Haeryoung Kim, Young Rok Choi, Jai Young Cho, Yoo-Seok Yoon, Ho-Seong Han, Ji Hyun Kim, Jin-Wook Kim, Sook-Hyang Jeong
- J Liver Cancer. 2016;16(1):42-46. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.42
- 888 Views
- 12 Downloads
-
 Abstract
Abstract
 PDF
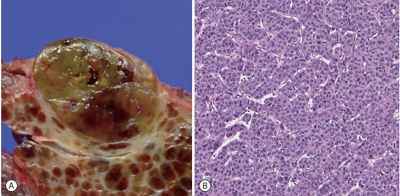
PDF - Hepatocellular carcinoma (HCC) shows a poor prognosis with high recurrence rate even after surgical resection. To improve prognosis of HCC patient, regular surveillance for high-risk group is recommended, but cost-benefit of the surveillance under 40 years old Asian male with hepatitis B infection is unclear. We share a 39-year-old male case which showed early recurrence and rapid extrahepatic metastasis after surgical resection for single huge HCC. Based on the pathologic finding, this case was diagnosed with ‘stemness’-related markerexpressing HCC. Further molecular classification for HCC could be beneficial to estimate individual risk for HCC recurrence and to predict prognosis.

Original Article
- Subclassification of Hepatocellular Carcinoma with Barcelona Clinic Liver Cancer Intermediate Stage
- Hye Won Lee, Seung Up Kim, Jun Yong Park, Do Young Kim, Snag Hoon Ahn, Kwang-Hyub Han, Beom Kyung Kim
- J Liver Cancer. 2016;16(1):17-22. Published online March 31, 2016
- DOI: https://doi.org/10.17998/jlc.16.1.17
- 1,319 Views
- 13 Downloads
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: Hepatocellular carcinoma (HCC) with Barcelona Clinic Liver Cancer (BCLC) intermediate stage includes a highly heterogeneous population. Here, we aimed to subclassify hepatocellular carcinoma with BCLC intermediate stage for better prognostification.
Methods
Between 2003 and 2008, 325 patients who were newly diagnosed as HCC with BCLC intermediate stage were considered eligible. Tumor factor and liver function were used for sub-classification. Overall survival (OS) was analyzed using Kaplan-Meier method with a comparison by log-rank test.
Results
A total of 325 patients with intermediate stage HCC were analyzed. Patients with tumor size ≥7 cm, tumor number ≥4 and Child-Pugh class B had the worse OS compared to those with tumor size <7 cm, tumor number <4 and Child-pugh class A, respectively (all P<0.05). These three variables affected the OS independently from multivariate Cox regression analysis (all P<0.05). So, using these three variables, patients were finally sub-classified as those with fulfilling none of three factors (B-a), one of three factors (B-b), two of three factors (B-c) and all of three factors (B-d) with the median OS of 39.2, 20.6, 12.0 and 8.3 months with statistical significances (all P<0.05 between B-a and B-b, between B-b and B-c, and between B-c and B-d), respectively.
Conclusions
Sub-classification of HCC with BCLC intermediate stage may be useful in not only prognostification but also guidance of treatment strategies. (J Liver Cancer 2016;16:17-22)


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter