Gallbladder Fistula Treated with N-Butyl-2-Cyanoacrylate after Radiofrequency Ablation in a Hepatocellular Carcinoma Patient: a Case Report
Article information
Abstract
Radiofrequency ablation (RFA) is a minimally invasive local therapy for hepatocellular carcinoma (HCC). Even though RFA is considered to be a safe treatment modality, a variety of complications have been reported. Recently, we encountered a case of refractory fistula between a liver abscess and the gallbladder after RFA. A 64-year-old woman diagnosed with HCC associated with chronic hepatitis B was treated by RFA. After RFA, she experienced abdominal pain, and abdominal computed tomography (CT) revealed a liver abscess complicated by a previous treatment of HCC, she was treated with intravenous antibiotics and percutaneous abscess drainage. Follow-up abdominal CT revealed a fistula between the liver abscess and gallbladder, which was successfully treated with percutaneous transcatheter n-butyl-2-cyanoacrylate (NBCA) embolization. We herein report the rare case of a refractory fistula between a liver abscess and the gallbladder after RFA in a patient treated with NBCA embolization.
INTRODUCTION
Although the mainstay of hepatocellular carcinoma (HCC) therapy is surgical resection, the majority of patients are not treated by surgery because of tumor extent and poor hepatic reserve [1]. Radiofrequency ablation (RFA) is a minimally invasive local therapy that is a thermal ablation technique for achieving coagulative necrosis of HCC and has been considered a relatively safe treatment modality [2,3]. However, RFA may cause complications, such as injury to the adjacent normal tissue related to mechanical and thermal damages. We report the case of a refractory fistula that developed between a liver abscess and the gallbladder after RFA in a patient that was successfully treated with percutaneous transcatheter n-butyl-2-cyanoacrylate (NBCA) embolization.
CASE REPORT
A 64-year-old female patient presented to the hospital with the chief complaint of right upper quadrant ab dominal pain. Five years prior, she had been diagnosed with HCC associated with chronic hepatitis B and had undergone repeated transarterial chemoembolization. Ten days prior, the patient was discharged without complications after RFA due to HCC recurrence in segment 8. She had no alcohol consumption and smoking history. With the exception of appendectomy and vitiligo, she had no medical history. Physical examination showed tenderness in the right upper abdomen. She appeared acutely ill, with a blood pressure of 74/40 mmHg, heart rate of 84 beats/min, respiratory rate of 18 breaths/min, and body temperature of 37.5℃.
Laboratory test results showed a white blood cell count of 35,420/mm3, hemoglobin level of 11.9 g/dL, platelet count of 432,000/μL, aspartate aminotransferase level of 31 IU/L, alanine aminotransferase level of 24 IU/L, total protein level of 6.8 g/dL, total albumin level of 4.1 g/dL, prothrombin time of 14.4 seconds, total bilirubin concentration of 0.5 mg/dL, alpha-fetoprotein level of 33.2 ng/mL, lactate level of 6.1 mmol/L, and C reactive protein level of 11.22 mg/dL. Hepatitis virus markers showed hepatitis B surface antigen positivity, hepatitis B surface antibody negativity, immunoglobulin G anti-hepatitis B core antigen positivity, serum hepatitis B virus DNA level <15 IU/mL, and anti-hepatitis C virus negativity.
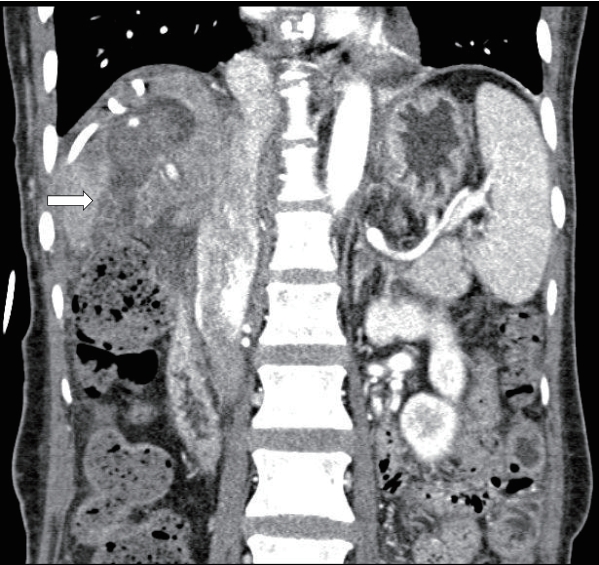
Dynamic abdominal computed tomography (CT) that was conducted at the time of the hospital visit showed complete ablation of the HCC in segment 8, but also a low-density mass with irregular margins suggestive of a liver abscess at the RFA site and perihepatic fluid collection (Fig. 1).

Dynamic CT during arterial phase showing an ill-defined, irregularly shaped liver abscess in the right anterior, superior segment of the liver and perihepatic fluid collection. CT, computed tomography.
The patient was diagnosed with liver abscess and septic shock after RFA in consideration of hypotension, fever, and laboratory and CT findings. She was hospitalized, was administered intravenous empirical antibiotics and inotropics, and underwent ultrasound-guided percutaneous abscess drainage by placement of a pigtail catheter in the abscess. The patient’s vital signs were stabilized, and abdominal pain and leukocytosis also improved. While the drainage amount gradually decreased, from the 14 days of pigtail catheter insertion, 50-80 mL of greenish fluid was continuously drained. Drained fluid analysis showed a greenish color and polydominant exudate suggestive of a bile and pus mixture. Follow-up abdominal CT was performed on the 18th day of pigtail catheter insertion to check for complications, and CT showed suspicion of a liver abscess and gallbladder fistula (Fig. 2). The tubography via the pigtail catheter also revealed a fistulous communication between the gallbladder and liver abscess (Fig. 3). Surgical resection including cholecystectomy was considered for fistula treatment, but the patient refused the surgery because of concern about the associated complications and risk. Therefore, we expected the closure of the fistula while continuing the conservative treatment of percutaneous abscess drainage and antibiotics. However, the fistula that failed to resolve after 4 weeks of conservative treatment was considered persistent, and right pleural effusion occurred; we decided to perform embolization of the persistent fistula tract using NBCA (Histoacryl®, B. Braun Avitum AG, Spangenberg, Germany).
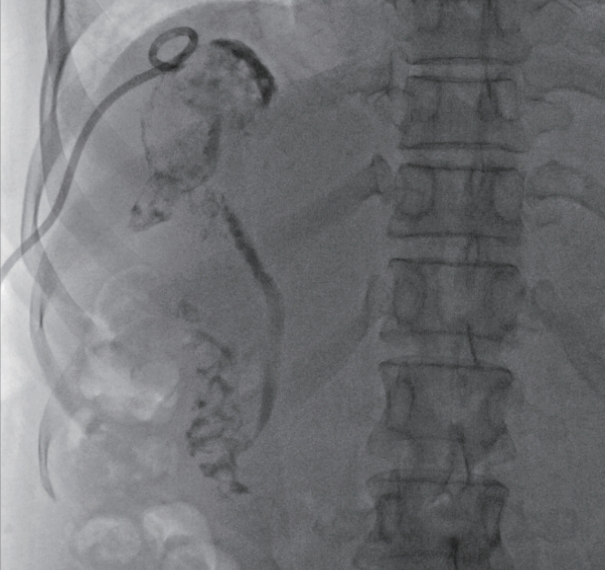
Tubography via a pigtail catheter showing the passage of the contrast dye through the gallbladder, cystic duct, common bile duct, and duodenum due to fistula formation between the abscess and gallbladder.
NBCA and oily contrast agent Lipiodol Ultra-Fluid (Guerbert GmbH, Sulzbach, Germany) were mixed in a 1:1 ratio and injected at a volume and rate suitable for polymerization reaction to fill and seal the gallbladder, fistula tract, and remnant abscess cavity (Fig. 4). After the embolization procedure, the percutaneous drainage catheter was withdrawn. Seven days after the procedure, CT showed that the NBCA had sealed the remnant abscess cavity, fistula tract, and gallbladder, and tubography confirmed fistula tract occlusion through non-visualization of the cystic duct, common bile duct, and duodenum (Figs. 5, 6). The patient was discharged and was followed up periodically in the outpatient clinic with abdominal CT. Fistula-related complications no longer occurred, and NBCA and Lipiodol Ultra-Fluid mixtures were no longer visible on follow-up CT 2 years later.
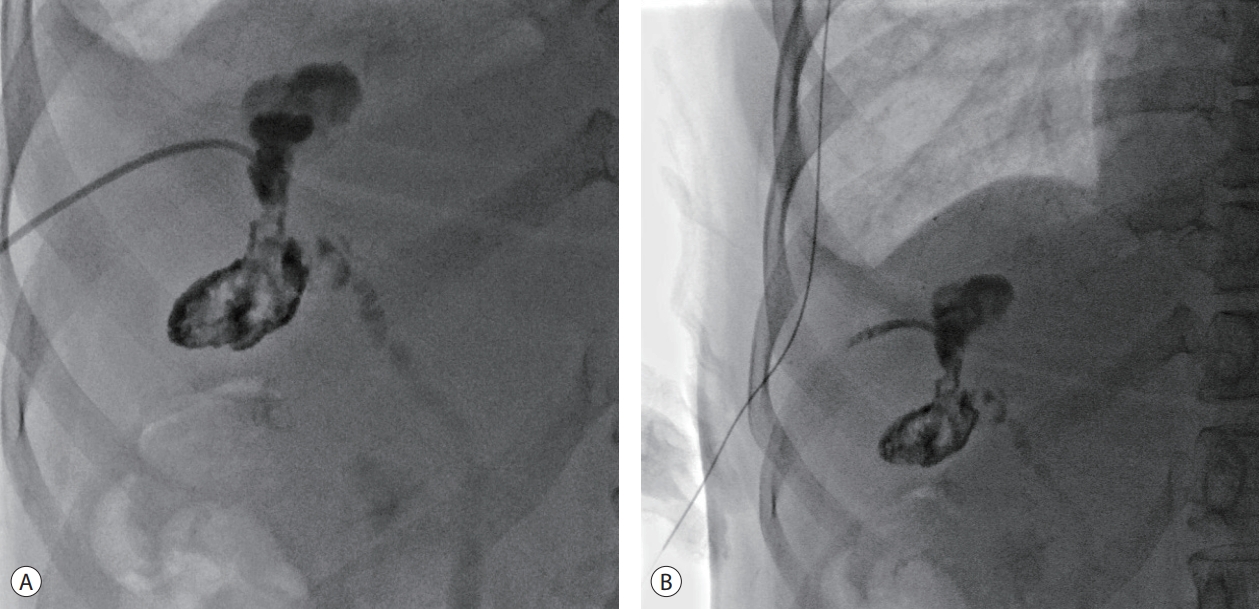
(A) Tubography showing fistula embolization with an NBCA-lipiodol mixture, and NBCA is observed along the previous remnant abscess, fistula tract, and gallbladder. (B) After the fistula tract embolization procedure, the percutaneous drainage catheter was removed. NBCA, n-butyl-2-cyanoacrylate.

CT showing the remnant abscess, fistula tract, and gallbladder cavity sealed with NBCA. CT, computed tomography; NBCA, n-butyl-2-cyanoacrylate.
DISCUSSION
RFA is widely used as a curative treatment modality for early HCC, which has excellent treatment outcomes and low risks for procedures. The incidence rates of complications were found to be 2.4% in domestic studies and 1.5% in other studies [4,5]. Complications include mild complications, such as fever, abdominal pain, and general weakness, which spontaneously bside over time, and serious major complications, which may lead to death if they are not adequately diagnosed and treated, such as liver abscess, intraabdominal hemorrhage, hepatic infarction, bowel perforation, tumor seeding, biliary duodenal fistula, and abscess-colonic fistula [4-6]. The incidence rates of major complications in both domestic and other multicenter studies were found to be 2.4% and 4.0%, respectively [5,6]. Among major complications, liver abscess is the most common [5]. Image-guided percutaneous drainage is the mainstay therapy, but this therapy modality often has limited effectiveness in the presence of an associated fistula. There is no standard treatment for a liver abscess with a fistula. When only an abscess is treated without the fistula resolution, it causes recurrent infection or secondary complications. Our patient refused surgical treatment for fistula that did not respond to antibiotics and percutaneous drainage therapy. Therefore, nonsurgical treatment was considered, and the fistula was treated using NBCA, which is used to embolize the vascular lumen and fistula of extravascular structures. Percutaneous treatments of non-healing fistulas with the use of NBCA have been reported in patients with colonic-abscess, biliary-enteric, tracheoesophageal, and bronchopleural fistulae [7-10].
This is the first case report of a fistula between a liver abscess and the gallbladder after RFA that was treated using percutaneous transcatheter NBCA embolization. Surgical resection may be considered for the treatment of a fistula, but the surgical risk is high when considering the patients’ reduced liver function and performance status due to underlying cirrhosis and HCC. This case suggests that percutaneous NBCA embolization may be a therapeutic option for persistent fistula between a liver abscess and the gallbladder with an alternative to major surgical intervention. However, there is no large-scale study of the results of treatment including delayed complications and recurrence after percutaneous radiologic intervention using NBCA embolization in a fistula, so further studies are needed.
Notes
The authors declare no conflicts of interest relevant to this article.