Search
- Page Path
- HOME > Search
Case Report
- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy
- Hun Kim, Tae Hoon Roh, Jun Seop Lee, Min Seong Kim, Beom Kyung Kim
- J Liver Cancer. 2024;24(1):113-117. Published online November 29, 2023
- DOI: https://doi.org/10.17998/jlc.2023.11.05
- 778 Views
- 78 Downloads
-
 Abstract
Abstract
 PDF
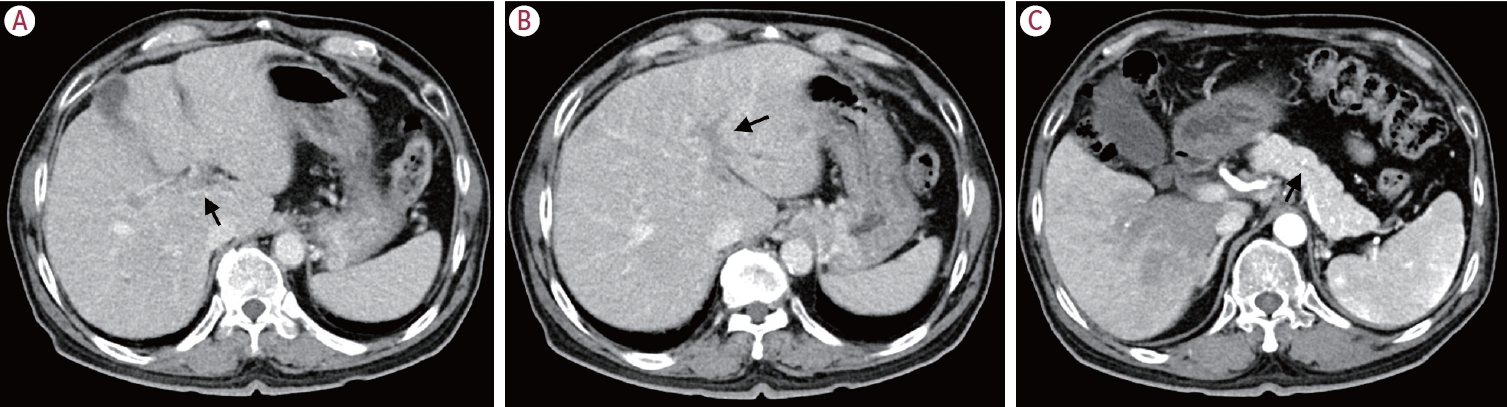
PDF - Portal vein tumor thrombosis (PVTT) is an uncommon condition in which tumor cells expand into the vessels, causing blood clot formation in the portal vein. PVTT is mainly associated with hepatocellular carcinoma, leading to an unfavorable prognosis; however, it can also develop in patients with other cancer types. Herein, we report a case of metastatic renal cell carcinoma diagnosed by a blind liver biopsy in a patient with dynamic computed tomography-confirmed portal vein thrombosis and cholangiopathy. This case illustrates the importance of systematic surveillance with routine laboratory tests and contrast-enhanced imaging studies on patients with cancer to detect potential liver infiltration of metastatic cancer.

Review Article
- Liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis
- Sang Jin Kim, Jong Man Kim
- J Liver Cancer. 2021;21(2):105-112. Published online September 2, 2021
- DOI: https://doi.org/10.17998/jlc.2021.03.17
- 4,982 Views
- 221 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
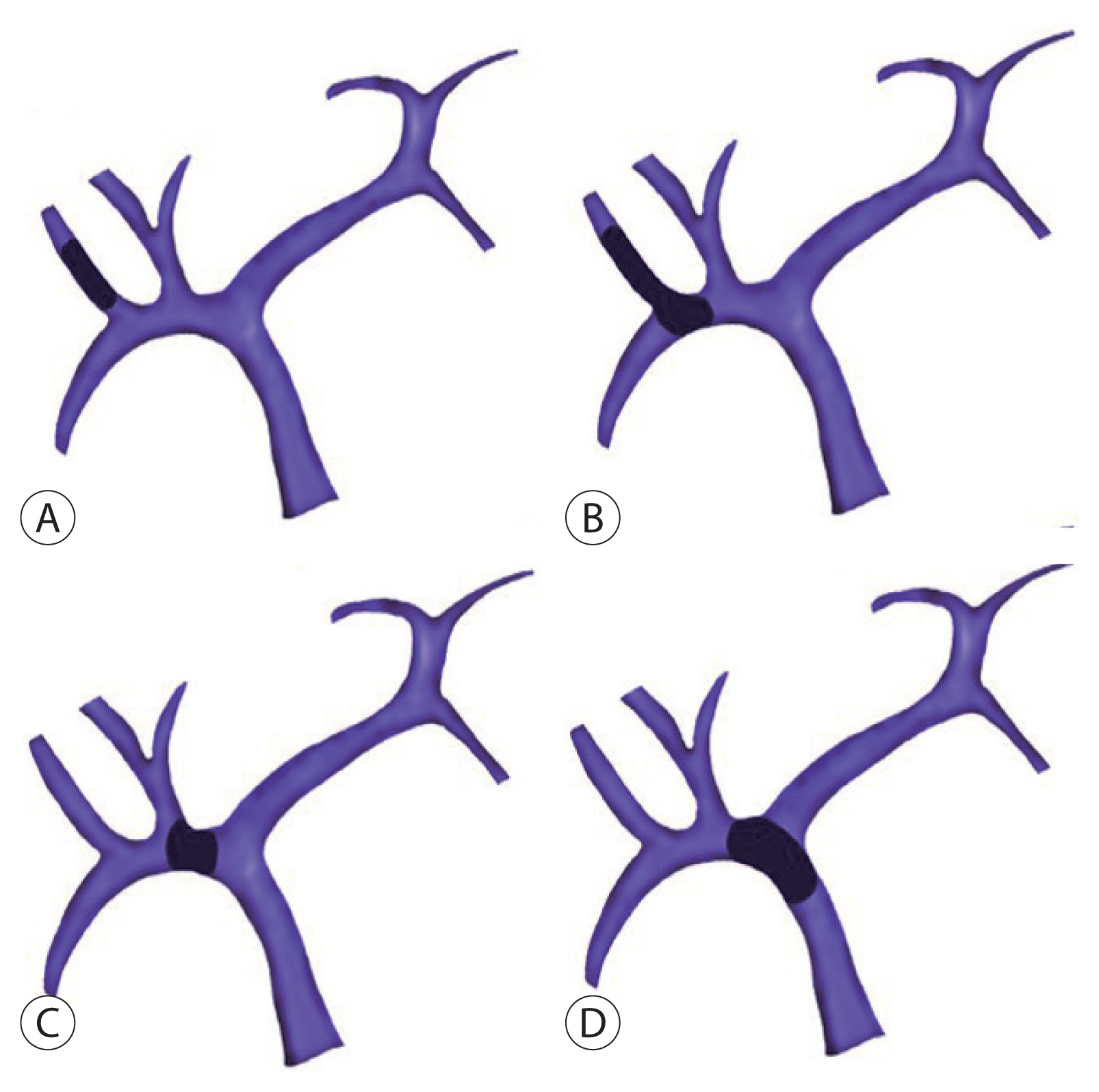
PDF - Traditionally, liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis is not recommended. However, with recent developments in locoregional therapies for hepatocellular carcinoma, more aggressive treatments have been attempted for advanced hepatocellular carcinoma. Recently, various studies on locoregional therapies for downstaging followed by living donor liver transplantation reported inspiring overall survival and recurrence-free survival of patients. These downstaging procedures included three-dimensional conformal radiation therapy, trans-arterial chemoembolization, stereotactic body radiation therapy, trans-arterial radioembolization, hepatic arterial infusion chemotherapy and combinations of these therapies. Selection of the optimal downstaging protocol should depend on tumor location, biology and background liver status. The risk factors affecting outcome include pre-downstaging alpha-fetoprotein values, delta alpha-fetoprotein values, disappearance of portal vein tumor thrombosis on imaging and meeting the Milan criteria or not after downstaging. For hepatocellular carcinoma with portal vein tumor thrombosis, downstaging procedure with liver transplantation in mind would be helpful. If the reaction of the downstaged tumor is good, liver transplantation may be performed.
-
Citations
Citations to this article as recorded by- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy
Hun Kim, Tae Hoon Roh, Jun Seop Lee, Min Seong Kim, Beom Kyung Kim
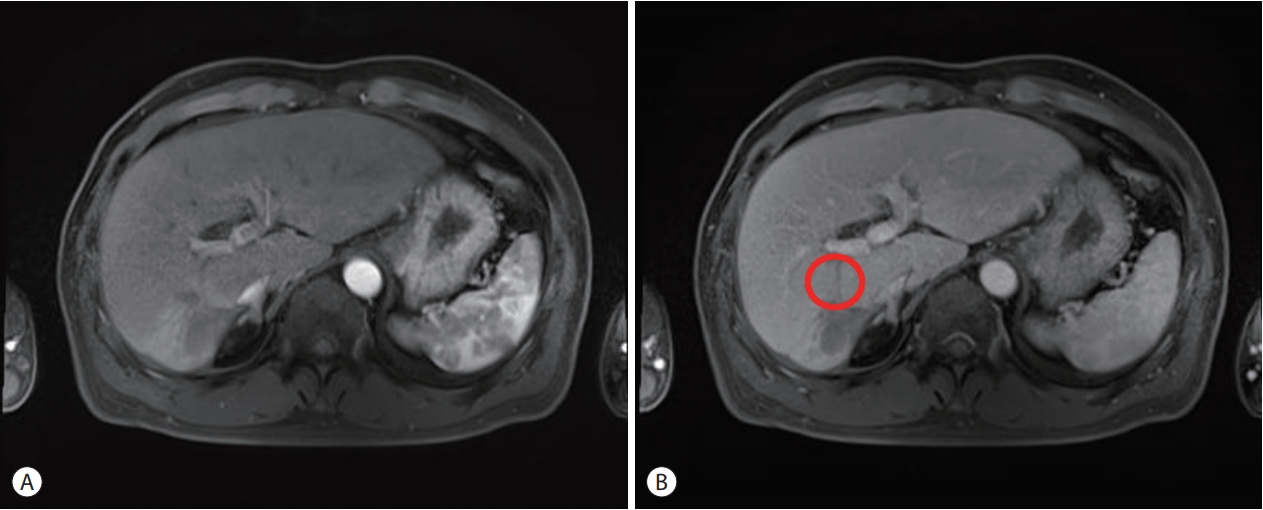
Journal of Liver Cancer.2024; 24(1): 113. CrossRef - Refining MRI-based criteria for portal vein invasion in hepatocellular carcinoma: improving sensitivity beyond portal vein tumor thrombosis
Jeongju Kim, Woo Kyoung Jeong, Jong Man Kim, Sang Yun Ha, Kyunga Kim
Abdominal Radiology.2023; 49(2): 437. CrossRef - Prediction models of hepatocellular carcinoma recurrence after liver transplantation: A comprehensive review
Sang Jin Kim, Jong Man Kim
Clinical and Molecular Hepatology.2022; 28(4): 739. CrossRef
- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy

Case Reports
- Hepatocellular Carcinoma with Segmental Portal Vein Invasion Exhibiting a Complete Response after Transarterial Radioembolization
- Jun Sik Yoon, Su Jong Yu, Yun Bin Lee, Eun Ju Cho, Jeong-Hoon Lee, Yoon Jun Kim, Jung-Hwan Yoon
- J Liver Cancer. 2019;19(2):159-164. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.159

- 5,289 Views
- 73 Downloads
-
 Abstract
Abstract
 PDF
PDF - The treatment options available for patients with hepatocellular carcinoma (HCC) with portal vein invasion (PVI) include sorafenib, transarterial radioembolization (TARE), radiation therapy (RT), transarterial chemoembolization with RT, and proton beam irradiation. Herein, we present a case of HCC with segmental PVI that was managed via TARE. The patient had a 4 cm HCC that invaded the segment VIII portal vein branch without extrahepatic spread. Liver function was Child-Pugh grade A, and performance status was good. TARE was performed without any adverse events, and a radiological complete response (CR) was achieved. Thereafter, the patient was followed-up every 3-6 months without any further treatment, and the CR was maintained for >3 years. Therefore, TARE may be a useful alternative therapeutic option for patients with HCC exhibiting segmental PVI.

- Liver Transplantation after Successful Downstaging with Hepatic Arterial Infusion Chemotherapy in a Patient with Hepatocellular Carcinoma with Portal Vein Tumor Thrombus
- Hee Chul Nam, Pil Soo Sung, Ho Jong Chun, Dong Goo Kim, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon
- J Liver Cancer. 2019;19(1):64-68. Published online March 31, 2019
- DOI: https://doi.org/10.17998/jlc.19.1.64
- 3,230 Views
- 58 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. The majority of patients with HCC are diagnosed at advanced disease stages with vascular invasion, where curative approaches are often not feasible. Currently, sorafenib is the only available standard therapy for HCC with portal vein tumor thrombosis (PVTT). However, in many cases, sorafenib therapy fails to achieve satisfactory results in clinical practice. We present a case of advanced HCC with PVTT that was treated with hepatic arterial infusion chemotherapy (HAIC) followed by liver transplantation. Three cycles of HAIC treatment resulted in necrotic changes in most of the tumors, and PVTT was reduced to an extent at which liver transplantation was possible. Further studies are required to determine the treatment strategies for advanced HCC with PVTT that can improve prognosis.

- Sorafenib Treatment in Advanced Hepatocellular Carcinoma with Tumor Thrombus Nearly Occupying the Entire Right Atrium
- Kang, Young Mo , Ryu, Soo Hyung , Lee, Bo Kyung , Ko, Kyoung Ho , Park, Tae Young , Moon, Jeong Seop , Cho, Seon Hwa
- J Liver Cancer. 2018;18(2):142-145. Published online September 30, 2018
- DOI: https://doi.org/10.17998/jlc.18.2.142
- 2,412 Views
- 36 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
PDF - Advanced hepatocellular carcinoma (HCC) with tumor thrombus extending through the hepatic veins, inferior vena cava, and right atrium (RA) is very rare. However, whether active treatments such as radiation, transcatheter arterial chemoembolization, and sorafenib in advanced HCC with RA involvement prolong survival is uncertain. We present a rare case of advanced HCC with tumor thrombus nearly occupying the entire RA that was treated with sorafenib. The patient received 400 mg sorafenib twice daily. However, her liver enzyme levels continued to increase and abdominal computed tomography showed an increase in the tumor size in the liver and RA. In the present case, active treatment with sorafenib was ineffective; thus, palliative care may be more beneficial in advanced HCC with extensive RA involvement.
-
Citations
Citations to this article as recorded by- Hepatocellular Carcinoma with Hepatic Vein and Inferior Vena Cava Invasion
Akash Shukla, Abhinav Jain
Journal of Clinical and Experimental Hepatology.2023; 13(5): 813. CrossRef - Clinical outcome and toxicity of radiotherapy for inferior vena cava tumor thrombus in HCC patients
So Jung Lee, Hong Seok Jang, Yoo Kyung Choi
Medicine.2021; 100(25): e26390. CrossRef - miR-4454 Promotes Hepatic Carcinoma Progression by Targeting Vps4A and Rab27A
Haoming Lin, Rui Zhang, Wenrui Wu, Liming Lei, Grzegorz Węgrzyn
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef
- Hepatocellular Carcinoma with Hepatic Vein and Inferior Vena Cava Invasion

Original Article
- Factors Affecting Prognosis of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis: Implications for Future Therapeutic Strategies
- Sang Jun Suh, Hyung Joon Yim, Dong Won Lee, Jong Jin Hyun, Young Kul Jung, Ji Hoon Kim, Yeon Seok Seo, Jong Eun Yeon, Kwan Soo Byun, Soon Ho Um
- J Liver Cancer. 2017;17(1):60-71. Published online March 31, 2017
- DOI: https://doi.org/10.17998/jlc.17.1.60
- 2,112 Views
- 23 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Background/Aim
s: Hepatocellular carcinoma (HCC) with portal vein tumor thrombosis (PVTT) exhibits poor prognosis. The aim of this study is to evaluate factors associated with survival of HCC patients with PVTT to suggest better therapeutic options.
Methods
Patients with HCC which were newly diagnosed at three tertiary hospitals between January 2004 and December 2012, were reviewed retrospectively. Among them, Barcelona Clinic of Liver Cancer stage C patients with PVTT were identified. Factors affecting overall survival (OS) were analyzed and efficacies of the treatment modalities were compared.
Results
Four hundred sixty five patients with HCC and PVTT were included. Liver function, tumor burden, presence of extrahepatic tumor, alfa fetoprotein, and treatment modalities were significant factors associated with OS. Treatment outcomes were different according to the initial modalities. OS of the patients who received hepatic resection, radiofrequency ablation (RFA), transarterial chemoembolization (TACE), hepatic arterial infusion chemotherapy (HAIC), sorafenib, systemic cytotoxic chemotherapy, radiation therapy (without combination), and supportive care were 27.8, 7.1, 6.7, 5.3, 2.5, 3.0, 1.8, and 0.9 months, respectively (P<0.001). Curative-intent treatments such as hepatic resection or RFA were superior to noncurativeintent treatments (P<0.001). TACE or HAIC was superior to sorafenib or systemic chemotherapy (P<0.001). Combining radiotherapy to TACE or HAIC did not provide additional benefit on OS (P=0.096).
Conclusions
Treatment modalities as well as baseline factors significantly influenced on OS of HCC patients with PVTT. Whenever possible, curative intent treatments should be preferentially considered. If unable, locoregional therapy would be a better choice than systemic therapy in HCC patients with PVTT. -
Citations
Citations to this article as recorded by- Value of surgical resection compared to transarterial chemoembolization in the treatment of hepatocellular carcinoma with portal vein tumor thrombus: A meta-analysis of hazard ratios from five observational studies
Keera Kang, Sung Kyu Song, Chul-Woon Chung, Yongkeun Park
Annals of Hepato-Biliary-Pancreatic Surgery.2020; 24(3): 243. CrossRef
- Value of surgical resection compared to transarterial chemoembolization in the treatment of hepatocellular carcinoma with portal vein tumor thrombus: A meta-analysis of hazard ratios from five observational studies

Review Article
- Locoregional Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis
- Sang Youn Hwang, Ryoung-Go Kim, Cheol-Won Choi, Sang Bu Ahn
- J Liver Cancer. 2016;16(2):69-81. Published online September 30, 2016
- DOI: https://doi.org/10.17998/jlc.16.2.69
- 993 Views
- 10 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) patients with portal vein tumor thrombosis (PVTT) have a extremely poor prognosis. According to the Barcelona Clinic Liver Cancer guideline, sorafenib is a standard therapy in this situation, but many clinicians still select locoregional therapy (LRT) such as transarterial therapy, external beam radiation therapy (EBRT), even surgical resection (SR) or combination of LRTs because the survival improvement by sorafenib is unsatisfactory. Based on recent meta-analysis and prospective study, transarterial chemoembolization (TACE) and transarterial radioembolization seem to be effective and safe therapeutic option that have comparable outcome to sorafenib. Recently large nationwide studies demonstrated that SR can be a potentially curative treatment in selected patients. Hepatic arterial infusion chemotherapy (HAIC) can be also good option, especially in Child class B patients based on small volume prospective studies. Moreover, multidisciplinary strategies based on the combination of LRTs (SR plus TACE, TACE + EBRT, TACE + Sorafenib, HAIC + EBRT etc.) may improve survival of HCC patients with PVTT. Finally we discuss individualized and tailored treatment strategies for different clinical situations.
-
Citations
Citations to this article as recorded by- Progress in Non-Surgical Treatment of Primary Hepatocellular Carcinoma with Combined Portal Vein Carcinoma Thrombosis
文豪 寇
Advances in Clinical Medicine.2023; 13(07): 11779. CrossRef
- Progress in Non-Surgical Treatment of Primary Hepatocellular Carcinoma with Combined Portal Vein Carcinoma Thrombosis

Case Reports
- A Case of Successful Hepatic Resection after Insufficient Response to Transarterial Chemoembolization and Radiation Therapy in Hepatocellular Carcinoma with Portal Vein Invasion
- Seong Kyun Na, Hyung Joon Yim, Sang Jun Suh, Young Kul Jung
- J Liver Cancer. 2016;16(2):118-122. Published online September 30, 2016
- DOI: https://doi.org/10.17998/jlc.16.2.118
- 915 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) with portal vein invasion has a poor prognosis. Treatments such as transarterial chemoembolization (TACE), radiation therapy (RT), sorafenib are done as a first line treatment. But in case of incomplete response to first line treatment, there’s no established guideline about salvage treatment. We present a 47 year-old male who was diagnosed as HCC with portal vein invasion. He was treated with RT and repeated TACE, but remnant viable tumor was observed. Surgical resection was performed as a salvage treatment, and HCC was completely removed. He has been followed up over 3 years, but there was no recurrence.

- 3 Cases of Portal Vein Thrombosis in Hepatocellular Carcinoma and Liver Cirrhosis Treated with Anticoagulation
- Byung Moo Ahn, Eaum Seok Lee, Seok Hyun Kim, Byung Seok Lee, Heon Young Lee
- J Liver Cancer. 2015;15(1):57-63. Published online March 31, 2015
- DOI: https://doi.org/10.17998/jlc.15.1.57
- 1,286 Views
- 20 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - The reported prevalence of PVT is in the range of 0.6-15.8% in patient with liver cirrhosis or portal hypertension. If the patient has hepatocellular carcinoma, thrombus is likely to be malignant thrombus. Malignancy, frequently of hepatic origin, is responsible for 21-24% of over all cases. The overall mortality rate of chronic PVT has been reported to be less than 10%, but is increased to 26% when associated with hepatocellular carcinoma and cirrhosis. However, no treatment guideline has been established on anticoagulant therapy for PVT in patients with concomitant hepatocellular carcinoma and cirrhosis. Because actually it is not easy to distinguish between malignant thrombus and benign thrombus in clinical aspect, PVT in hepatocellular carcinoma are still debatable whether or not treatment when it diagnosed. We present 3 cases of portal vein thrombosis successfully treated with anticoagulation in hepatocellular carcinoma and liver cirrhosis, and we include a literature review.
-
Citations
Citations to this article as recorded by- Evaluation of Low-Molecular-Weight Heparin for Treatment of Portal Vein Thrombosis in Liver Cirrhosis Patients
Ji Min Han, Youngil Koh, Sung Hwan Kim, Sung Yun Suh, Yoon Sook Cho, Jeong-Hoon Lee, Su Jong Yu, Jung-Hwan Yoon, Hye Sun Gwak
Medicina.2023; 59(2): 292. CrossRef
- Evaluation of Low-Molecular-Weight Heparin for Treatment of Portal Vein Thrombosis in Liver Cirrhosis Patients

- A Case of Progressive Superior Mesenteric Vein Thrombosis after Percutaneous Transhepatic Obliteration in Infiltrative Hepatocellular Carcinomaswith Portal Vein Thrombosis
- Hee Yeon Kim, Chung-Hwa Park, Sung won Lee, Do Seon Song, Myeong Jun Song, Jong Young Choi, Seung Kew Yoon, Si Hyun Bae, Jung Suk Oh, Ho Jong Chun
- Journal of the Korean Liver Cancer Study Group. 2012;12(2):146-150. Published online September 30, 2012
- 522 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - Percutaneous transhepatic obliteration of gastroesophageal varices is one of the effective emergency procedure when endoscopic therapy is not indicated or has been failed. One of the major complications of this procedure is portal thrombosis. A 53-year-old male with hepatitis B virus infection was diagnosed of infiltrative hepatocellular carcinoma with right portal vein thrombosis. On the next day after being hospitalization, the patient developed variceal bleeding. With medical management, endoscopic therapy was initially attempted, however, it ended in failure. Emergency percutaneous transhepatic obliteration of bleeding gastroesophageal varices was considered as a next option. Bleeding from gastroesophageal varices was stopped after percutaneous obliateration, however, portal thrombosis was extended to splenic vein or superior mesenteric veins.

- A Case of Hepatocellular Carcinoma Exhibited over Partial Response after Hepatic Arterial Infusion Chemotherapy
- Chang Wook Park, Young Lan Kown, Yong Jin Kim, Yoon Jung Kim, Hye Jin Seo, Kyung In Lee, Eun Soo Kim, Byung Kook Jang, Woo Jin Jeong, Kyung Sik Park, Kwang Bum Jo, Jae Seok Hwang, Young Hwan Kim, Jung Hyuk Kwon
- Journal of the Korean Liver Cancer Study Group. 2010;10(1):40-43. Published online June 30, 2010
- 582 Views
- 0 Download
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is one of the cancers with poor prognosis. Especially potal vein invasion is a grave prognostic indicator in the setting of HCC. There is currently no effective method for treatment of HCC with portal vein invasion. A 61-year-old female patient was diagnosed a massive HCCs in both hepatic lobe with portal vein thrombosis, based on computed tomography (CT) and increased tumor marker, α-fetoprotein. She was treated with intrahepatic arterial CDDP (10 mg on 1~5 day), 5-FU (250mg on 1~5 day) and leukovorin (12mg on 1~5 day) infusion via percutaneously implantable port system (PIPS) every 3 weeks, totally seven times. The patient was still living 6 months after first hepatic arterial infusion chemotherapy (HAIC) and follow-up CT showed partial response with necrosis of HCCs. We report here a case of advanced HCC with portal vein thrombosis that was effectively treated with HAIC via PIPS.

- A Case of Hepatocellular Carcinoma with Portal Vein Thrombi Successfully Treated with TACE Following Radiation Therapy
- Won Sub Choi, Sang Hoon Park, Kyung Rim Huh, Kyung Hun Lee, Tae Ho Hahn, Choong Kee Park, Min Jeong Kim, Eui-Yong Jeon, Su Ssan Kim
- Journal of the Korean Liver Cancer Study Group. 2008;8(1):106-110. Published online June 30, 2008
- 484 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - Transarterial chemoembolization (TACE) is one of treatment modalities which can give survival benefit to patients with hepatocellular carcinoma (HCC) to which curative therapies can be applied. But, TACE can encounter the risk of liver failure in case of HCC with main portal vein tumor thrombi. Advances in techniques to account for respiration motion and understanding of partial liver tolerance to radiation therapy have permitted us to deliver high dose radiation therapy without toxicity in treatment of HCC. We report a case of HCC with massive portal vein thrombosis which responded to TACE following radiation therapy.

- A Case of Advanced Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis Achieving Complete Response with New Therapeutic Modalities
- Hyun Young Woo, Jin Dong Kim, Jung Hyun Kwon, Chan Ran You, Jeong Won Jang, Si Hyun Bae, Jong Young Choi, Se Hyun Cho, Seung Kew Yoon, Dong Hoon Lee, Ho Jong Chun, Byung Gil Choi, Chul Seung Kay
- Journal of the Korean Liver Cancer Study Group. 2008;8(1):124-127. Published online June 30, 2008
- 732 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - A 45-year-old man was admitted for the treatment of hepatocellular carcinoma (HCC). He was diagnosed hepatitis B carrier 16 years ago and has not done a routine check. Abdominal CT showed a diffuse infiltrative HCC involving right hepatic lobe with portal vein tumor thrombosis (PVTT) involving right portal vein and proximal portion of left portal vein umbilical portion. With concurrent transcatheter arterial chemotherapy (TAC), helical tomotherapy for portal vein thrombosis was done. With these treatments, main tumor and PVTT was decreased in size markedly and no stain in hepatic angiogram. Due to repeated TAC, hepatic arterial stenosis occurred and TAC was stopped. 3 months after, recurrent tumor was detected in MRI. Radiofrequency ablation followed by High Intensity Focused Ultrasound (HIFU) was done for this recurrent mass. No viable mass was shown in the follow up MRI done 6 months after HIFU.

- A long-term survival case of advanced hepatocellular carcinoma with portal vein thrombosis successfully treated with multimodal treatments
- Ju Hyun Choi, Han Eul Song, Chang Il Kwon, Kwang Hyun Ko, Sung Pyo Hong, Seong Gyu Hwang, Pil Won Park, Kyu Sung Rim, Man Deuk Kim, Sung Won Kwon
- Journal of the Korean Liver Cancer Study Group. 2007;7(1):66-70. Published online June 30, 2007
- 480 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - We reported a 52-year-old women with hepatocellular carcinoma (HCC) of 10 cm in diameter involving entire right lobe with advanced tumor thrombosis in the both branches and main trunk of portal vein. She was treated with multimodal treatments resulting in a long-term survival of more than 5 years. At first, she was treated with hepatic arterial chemotherapy (HAC) using cisplatin and 5-FU for 5 cycles and radiation therapy in September 2002. The tumor size decreased and the main and left portal vein thrombosis was disappeared. Although, she had been treated with the 3th radiofrequency ablation (RFA) and the 3th transarterial chemoembolization (TACE) three times for the treatment of main tumor, follow-up CT scan still showed marginal viable tumor at the segment 5. Therefore, she was underwent right lobectomy of the liver and splenectomy. Further TACE was performed once for the small remnant tumor around inferior vena cava at the postoperative 4 months. Finally, she has been survived for over 5 years from the initial treatment and 23 months after operation without evidence of recurrence. We suggest that the long-term survival was achieved in this patient through appropriate treatment selections at the right time, such as HAC, RFA, TACE, hepatic resection and external radiotherapy based on changes in diagnostic imaging and tumor markers.

- A Case of Cyberknife Treatment for Hepatocellular Carcinoma with Portal Vein Tumor Thrombosis
- Chan Ran You, Si Hyun Bae, Hyun Young Woo, Soung Won Jeong, Jong Young Choi, Seung Kew Yoon, Hong Seok Jang, Dong Hoon Lee, Byung Gil Choi
- Journal of the Korean Liver Cancer Study Group. 2007;7(1):82-86. Published online June 30, 2007
- 768 Views
- 13 Downloads
-
 Abstract
Abstract
 PDF
PDF - A 64 year-old-male patient was transferred to our hospital for infiltrative hepatocellular carcinoma (HCC) without treatment response because of treatment failure and disease progression. He had been diagnosed infiltrating HCC 9 months ago and then treated with three times of transarterial chemolipiodolization (TACL) in other hospital. But, HCC was progressed. Abdominal CT showed infiltrating HCC in S7 and a small daughter nodule in S8 with right and main portal vein tumor thrombosis (PVTT). We performed stereotatic radiosurgery (Cyberknife) for the treatment of PVTT and four times of TACL for the treatment of intrahepatic HCC every 4weeks. The total radiation doses using with Cyberknife were 36Gy with a prescription isodose 80% in 3 fractions over the three consecutive days. After treatment, infiltrating HCC was decreased in size and PVTT was markedly regressed. Response rate of serum AFP was 57.2%. In conclusion, we report the case of good treatment response in the patient with HCC with PVTT after combination treatment of Cyberknife and TACL.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter