Search
- Page Path
- HOME > Search
Review Articles
- Changing etiology and epidemiology of hepatocellular carcinoma: Asia and worldwide
- Do Young Kim
- J Liver Cancer. 2024;24(1):62-70. Published online March 25, 2024
- DOI: https://doi.org/10.17998/jlc.2024.03.13
- 597 Views
- 55 Downloads
-
 Abstract
Abstract
 PDF
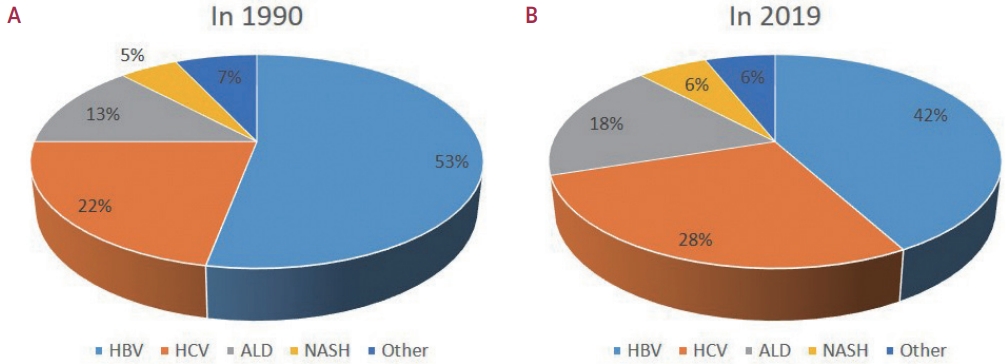
PDF - Approximately 80% of hepatocellular carcinoma (HCC) cases arise in sub-Saharan Africa and Eastern Asia, following a similarly high prevalence of chronic hepatitis B virus (HBV) carriers in these regions. The etiology and epidemiology of HCC have recently changed worldwide. Although HBV infection is the main contributor to HCC development, a slow but continuous decline in HBV infection rates has been reported since 1990. Owing to the widespread use of direct-acting antivirals, the incidence of hepatitis C virus-related HCC has remarkably decreased in Japan and European countries. In Korea, Taiwan, and Singapore, the incidence of HBV-related HCC has significantly decreased owing to vaccination against HBV. Globally, while HBV accounted for more than half of HCCs in 1990, this had decreased to 42% in 2019. In contrast, the proportion of patients with alcoholic- and nonalcoholic steatohepatitis (NASH) increased from 13% to 18% and from 5% to 6%, respectively. NASH-related HCC has characteristics that differ from those of virus-associated HCC. Compared with other etiologies, patients with NASHassociated HCC are older, have a higher body mass index, and have higher rates of type 2 diabetes mellitus, hypertension, hyperlipidemia, and cardiovascular disease. Nonalcoholic fatty liver disease (NAFLD)-associated HCC is also known to develop in the absence of cirrhosis, unlike alcohol-related and autoimmune liver diseases. Because patients with NAFLD usually have diabetes or obesity, surveying this population is challenging. Optimal selection of the target population and surveillance tools among patients with NAFLD needs to be determined.

- Non-alcoholic fatty liver disease-related hepatocellular carcinoma
- Darine Daher, Karim Seif El Dahan, Amit G. Singal
- J Liver Cancer. 2023;23(1):127-142. Published online February 9, 2023
- DOI: https://doi.org/10.17998/jlc.2022.12.30
- 3,124 Views
- 166 Downloads
- 7 Citations
-
 Abstract
Abstract
 PDF
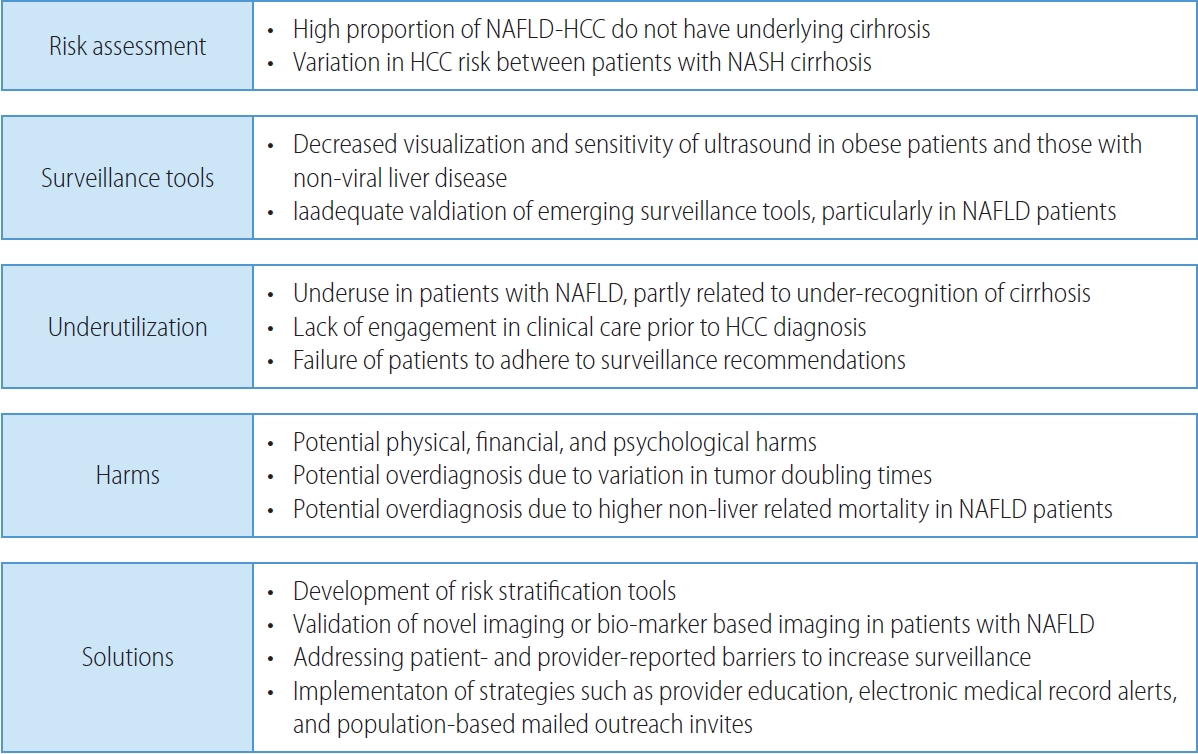
PDF - Non-alcoholic fatty liver disease (NAFLD), one of the most common causes of liver disease, is an increasingly common cause of hepatocellular carcinoma (HCC). Several demographic, clinical, and genetic factors contribute to HCC risk in NAFLD patients, which may inform risk stratification scores. Proven efficacious approaches to primary prevention approach in patients with non-viral liver disease remain an area of need. Semi-annual surveillance is associated with improved early tumor detection and reduced HCC-related mortality; however, patients with NAFLD have several challenges to effective surveillance, including under-recognition of at-risk patients, low surveillance utilization in clinical practice, and lower sensitivity of current tools for early-stage HCC detection. Treatment decisions are best made in a multidisciplinary fashion and are informed by several factors including tumor burden, liver dysfunction, performance status, and patient preferences. Although patients with NAFLD often have larger tumor burden and increased comorbidities compared to counterparts, they can achieve similar post-treatment survival with careful patient selection. Therefore, surgical therapies continue to provide a curative treatment option for patients diagnosed at an early stage. Although there has been debate about the efficacy of immune checkpoint inhibitors in patients with NAFLD, current data are insufficient to change treatment selection based on liver disease etiology.
-
Citations
Citations to this article as recorded by- Overnutrition and Lipotoxicity: Impaired Efferocytosis and Chronic Inflammation as Precursors to Multifaceted Disease Pathogenesis
Vivek Mann, Alamelu Sundaresan, Shishir Shishodia
Biology.2024; 13(4): 241. CrossRef - Risk of Hepatocellular Carcinoma by Steatotic Liver Disease and Its Newly Proposed Subclassification
Byeong Geun Song, Aryoung Kim, Myung Ji Goh, Wonseok Kang, Geum-Youn Gwak, Yong-Han Paik, Moon Seok Choi, Joon Hyeok Lee, Dong Hyun Sinn
Liver Cancer.2024; : 1. CrossRef - Smoking Increases the Risk of Hepatocellular Carcinoma and Cardiovascular Disease in Patients with Metabolic-Associated Fatty Liver Disease
Jeong-Ju Yoo, Man Young Park, Eun Ju Cho, Su Jong Yu, Sang Gyune Kim, Yoon Jun Kim, Young Seok Kim, Jung-Hwan Yoon
Journal of Clinical Medicine.2023; 12(9): 3336. CrossRef - Reply: Validation of MELD 3.0 scoring system in East Asian patients with cirrhosis awaiting liver transplantation
Jeong-Ju Yoo, Sang Gyune Kim
Liver Transplantation.2023; 29(11): E38. CrossRef - Unraveling the Janus-Faced Role of Autophagy in Hepatocellular Carcinoma: Implications for Therapeutic Interventions
Thi Ha Nguyen, Tuan Minh Nguyen, Dinh Thi Minh Ngoc, Taesik You, Mi Kyung Park, Chang Hoon Lee
International Journal of Molecular Sciences.2023; 24(22): 16255. CrossRef - Comparative Analysis of Atezolizumab Plus Bevacizumab and Hepatic Artery Infusion Chemotherapy in Unresectable Hepatocellular Carcinoma: A Multicenter, Propensity Score Study
Ji Kim, Hee-Chul Nam, Chang-Wook Kim, Hee Cho, Jae-Sung Yoo, Ji Han, Jeong Jang, Jong Choi, Seung Yoon, Hyun Yang, Si Bae, Suho Kim, Jung Oh, Ho Chun, Chang Jeon, Jaegyoon Ahn, Pil Sung
Cancers.2023; 15(17): 4233. CrossRef - A nationwide study on the current treatment status and natural prognosis of hepatocellular carcinoma in elderly
Jeong-Ju Yoo, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park
Scientific Reports.2023;[Epub] CrossRef
- Overnutrition and Lipotoxicity: Impaired Efferocytosis and Chronic Inflammation as Precursors to Multifaceted Disease Pathogenesis

Case Report
- A Case of Hepatocellular Carcinoma in Non-alcoholic Fatty Liver Disease
- Seok, Jun , Suk, Ki Tae , Kim, Dong Joon
- J Liver Cancer. 2018;18(1):51-54. Published online March 31, 2018
- DOI: https://doi.org/10.17998/jlc.18.1.51
- 1,964 Views
- 37 Downloads
-
 Abstract
Abstract
 PDF
PDF - Non-alcoholic fatty liver disease (NAFLD) has been one of the causes of cryptogenic hepatocellular carcinoma (HCC). NAFLD-associated HCC (NAFLD-HCC) have clinical features such as high body mass index, deranged lipid profiles, or diabetes mellitus. We experienced a 72-year–old woman with NAFLD associated HCC which was recurred after surgical resection.

Review Articles
- Non-alcoholic Fatty Liver Disease and Hepatocellular Carcinoma
- Hyunwoo Oh, Dea Won Jun
- J Liver Cancer. 2017;17(2):117-125. Published online September 30, 2017
- DOI: https://doi.org/10.17998/jlc.17.2.117
- 3,423 Views
- 116 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is one of the most common life-threatening cancers worldwide. Recently, many patients with non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH) have progressed to HCC even in the absence of cirrhosis. As the morbidity of metabolic syndrome increases, the proportion of HCC associated with NAFLD is expected to increase gradually. A new mechanism for the development of HCC in NAFLD has been identified; Diabetes mellitus, insulin resistance, obesity, lipotoxicity, gut dysbiosis are risk factors. Inflammatory cytokines such as adipokines, leptin, tumor necrosis factor-α, interlukin-8, nuclear factor-κB constitute dysplasia-carcinoma sequence. At the time of diagnosis, NAFLD/ NASH related HCC tend to progress to larger and in advanced tumor-node-metastasis stages compared to viral hepatitis related HCC. But there are no guidelines for early detection of NAFLD-related HCC. So, it is essential to study the screening program for the early detection of NAFLD-related HCC and precise methods for NAFLD.

- Obesity and Hepatocellular Carcinoma
- Won Sohn
- J Liver Cancer. 2016;16(2):86-91. Published online September 30, 2016
- DOI: https://doi.org/10.17998/jlc.16.2.86
- 907 Views
- 20 Downloads
-
 Abstract
Abstract
 PDF
PDF - Obesity is closely associated with hepatocellular carcinoma (HCC) as well as other malignancies. Obesity is an important risk factor for cancer development and overall mortality in HCC. Molecular mechanisms of hepatocarcinogenesis in obesity are adipose tissue remodeling, dysregulation of adipokines, increased reactive oxygen species, insulin resistance or hyperinsulinemia, alteration of gut microbiota, and dysregulation of microRNA. Obesity is the most common cause of non-alcoholic fatty liver disease (NAFLD) or non-alcoholic steatohepatitis (NASH). NAFLD or NASH leads to HCC as well as liver cirrhosis. Hepatitis C virus regulates lipid homeostasis in liver. Obesity and its’ related factors (metabolic syndrome and diabetes mellitus) are significantly related to the risk of HCC development in chronic hepatitis C. However, it is not clear whether obesity is a risk factor for HCC in chronic hepatitis B. The relationship between obesity and HCC seems to be different according to etiology of background liver disease. Further studies are needed to clarify the effect of obesity on HCC in different etiologies of chronic liver disease.

- Pathogenic Mechanism of Hepatocellular Carcinoma in Non-alcoholic Fatty Liver Disease
- Sun Min Kim, Joo Hyun Sohn
- J Liver Cancer. 2014;14(2):63-72. Published online September 30, 2014
- DOI: https://doi.org/10.17998/jlc.14.2.63
- 902 Views
- 31 Downloads
-
 Abstract
Abstract
 PDF
PDF - Non-alcoholic fatty liver disease (NAFLD) is a clinicopathologic condition that shows excessive fat accumulation in hepatocytes without significant alcohol intake, other liver diseases and the history of using hepatotoxic drugs. Recently, the incidence of hepatocellular carcinoma (HCC) related to NAFLD is increasing. However, the pathogenic mechanism of HCC developed from NAFLD has not been fully known. The most important pathogenic factor which affects the development of HCC is cirrhosis itself from any causes including NAFLD. To date, it is considered that NAFLD can cause HCC through insulin resistance, oxidative stress, and inflammatory process. In NAFLD, insulin resistance and its resulting hyperinsulinemia increase insulin-like growth factor-1 (IGF-1), which leads to cell growth and inhibition of apoptosis. Furthermore, hyperinsulinemia activates c-Jun amino-terminal kinase 1 (JNK1), increases free fatty acid (FFA) and reactive oxygen species (ROS), and increases the level of some inflammatory cytokines. In addition to that, various molecular biologic mechanisms such as deregulated NF-κB signaling, disorder in PI3K-AKT-PTEN pathway, defect in one-carbon metabolism, and dysfunction of microRNAs are involved in the NAFLD-mediated carcinogenesis. Finally, intestinal dysbiosis may also play a role in the pathogenesis of HCC. These pathogenic mechanisms will be discussed shortly in this review. (J Liver Cancer 2014;14:63-72)


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter