Search
- Page Path
- HOME > Search
Review Article
- Management of early-stage hepatocellular carcinoma: challenges and strategies for optimal outcomes
- Jae Hyun Yoon, Sung Kyu Choi
- J Liver Cancer. 2023;23(2):300-315. Published online September 21, 2023
- DOI: https://doi.org/10.17998/jlc.2023.08.27
- 2,154 Views
- 144 Downloads
- 4 Citations
-
 Abstract
Abstract
 PDF
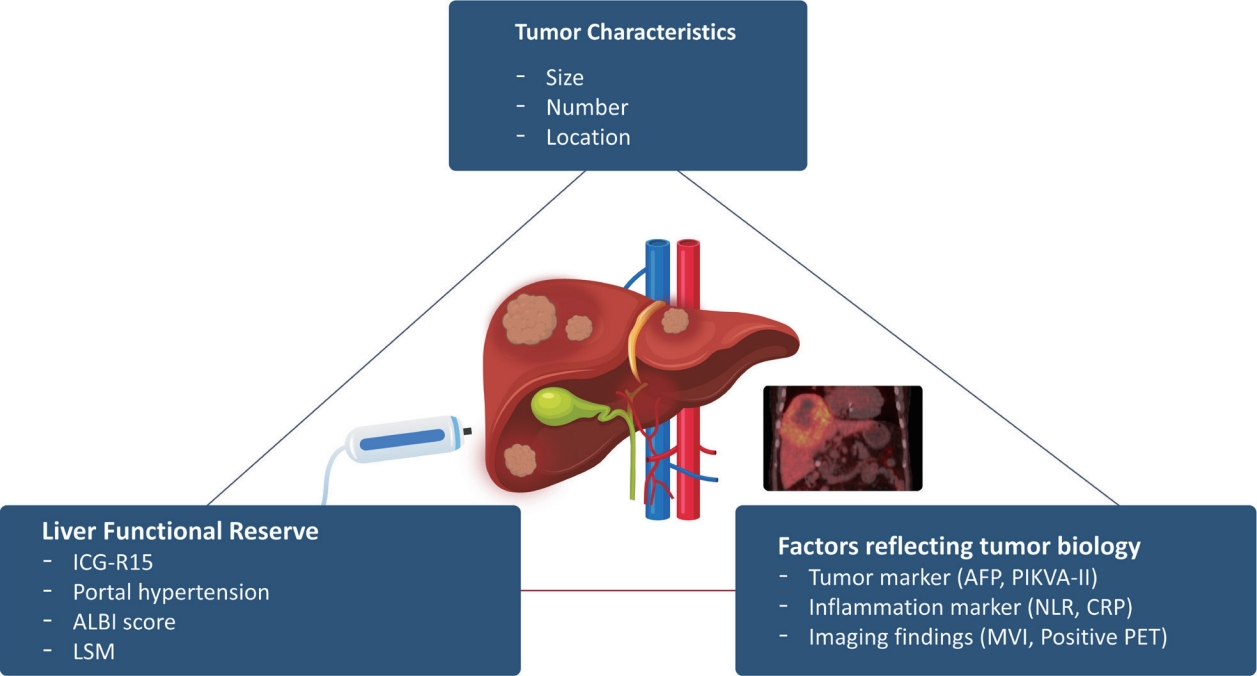
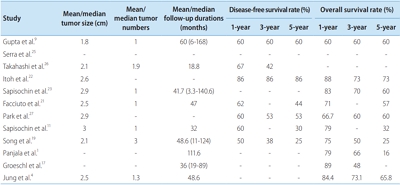
PDF - Although hepatocellular carcinoma (HCC) is associated with a poor prognosis, management of early-stage HCC is often successful with highly efficacious treatment modalities such as liver transplantation, surgical resection, and radiofrequency ablation. However, unfavorable clinical outcomes have been observed under certain circumstances, even after efficient treatment. Factors that predict unsuitable results after treatment include tumor markers, inflammatory markers, imaging findings reflecting tumor biology, specific outcome indicators for each treatment modality, liver functional reserve, and the technical feasibility of the treatment modalities. Various strategies may overcome these challenges, including the application of reinforced treatment indication criteria with predictive markers reflecting tumor biology, compensation for technical issues with up-to-date technologies, modification of treatment modalities, downstaging with locoregional therapies (such as transarterial chemotherapy or radiotherapy), and recently introduced combination immunotherapies. In this review, we discuss the challenges to achieving optimal outcomes in the management of early-stage HCC and suggest strategies to overcome these obstacles.
-
Citations
Citations to this article as recorded by- Diosgenin potentiates the anticancer effect of doxorubicin and volasertib via regulating polo-like kinase 1 and triggering apoptosis in hepatocellular carcinoma cells
Eman H. Yousef, Mohamed E. El-Mesery, Maha R. Habeeb, Laila A. Eissa
Naunyn-Schmiedeberg's Archives of Pharmacology.2024;[Epub] CrossRef - Comparison of Surgical Resection and Radiofrequency Ablation in Elderly Patients with Hepatocellular Carcinoma
Jun Il Kim, Jayoun Lee, Gi Hong Choi, Min Woo Lee, Dong Ah Park, Jeong-Ju Yoo
Digestive Diseases and Sciences.2024; 69(3): 1055. CrossRef - Radiofrequency for hepatocellular carcinoma larger than 3 cm: potential for applications in daily practice
Ji Hoon Kim, Pil Soo Sung
Journal of Liver Cancer.2024; 24(1): 1. CrossRef - Efficacy of Transarterial Chemoembolization (TACE) for Early-Stage Hepatocellular Carcinoma
Moonhyung Lee, Hyun Phil Shin
Medicina.2023; 59(12): 2174. CrossRef
- Diosgenin potentiates the anticancer effect of doxorubicin and volasertib via regulating polo-like kinase 1 and triggering apoptosis in hepatocellular carcinoma cells

Case Report
- Curative liver transplantation after lung resection for advanced hepatocellular carcinoma with lung metastasis and inferior vena cava tumor thrombosis: a case report
- Dong Jin Joo, Do Young Kim, Jinsil Seong, Hyun Jeong Kim, Jae Geun Lee, Dai Hoon Han, Gi Hong Choi, Myoung Soo Kim, Jin Sub Choi, Soon Il Kim
- J Liver Cancer. 2021;21(2):181-186. Published online September 30, 2021
- DOI: https://doi.org/10.17998/jlc.2021.09.08

- 3,606 Views
- 91 Downloads
- 1 Citation
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) with distant metastasis is an absolute contraindication for liver transplantation (LT). However, it is still unclear whether LT is feasible or acceptable in such patients, albeit after being treated with a multidisciplinary approach and after any metastatic lesion is ruled out. We report one such successful treatment with living donor LT (LDLT) after completely controlling far-advanced HCC with inferior vena cava tumor thrombosis and multiple lung metastases. The patient has been doing well without HCC recurrence for eight years since LDLT. The current patient could be an anecdotal case, but provides a case for expanding LDLT indications in the context of advanced HCC and suchlike.
-
Citations
Citations to this article as recorded by- Inferior Vena Cava Thrombectomy and Stenting as Bridge to Liver Transplantation After Radiotherapy-Induced Thrombosis
Raphael PH Meier, Shani Kamberi, Josue Alvarez-Casas, Barton F. Lane, Chandra S. Bhati, Saad Malik, William Twaddell, Kirti Shetty, Adam Fang, Hyun S. Kim, Daniel G. Maluf
Progress in Transplantation.2023;[Epub] CrossRef
- Inferior Vena Cava Thrombectomy and Stenting as Bridge to Liver Transplantation After Radiotherapy-Induced Thrombosis

Review Article
- Liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis
- Sang Jin Kim, Jong Man Kim
- J Liver Cancer. 2021;21(2):105-112. Published online September 2, 2021
- DOI: https://doi.org/10.17998/jlc.2021.03.17
- 4,995 Views
- 221 Downloads
- 3 Citations
-
 Abstract
Abstract
 PDF
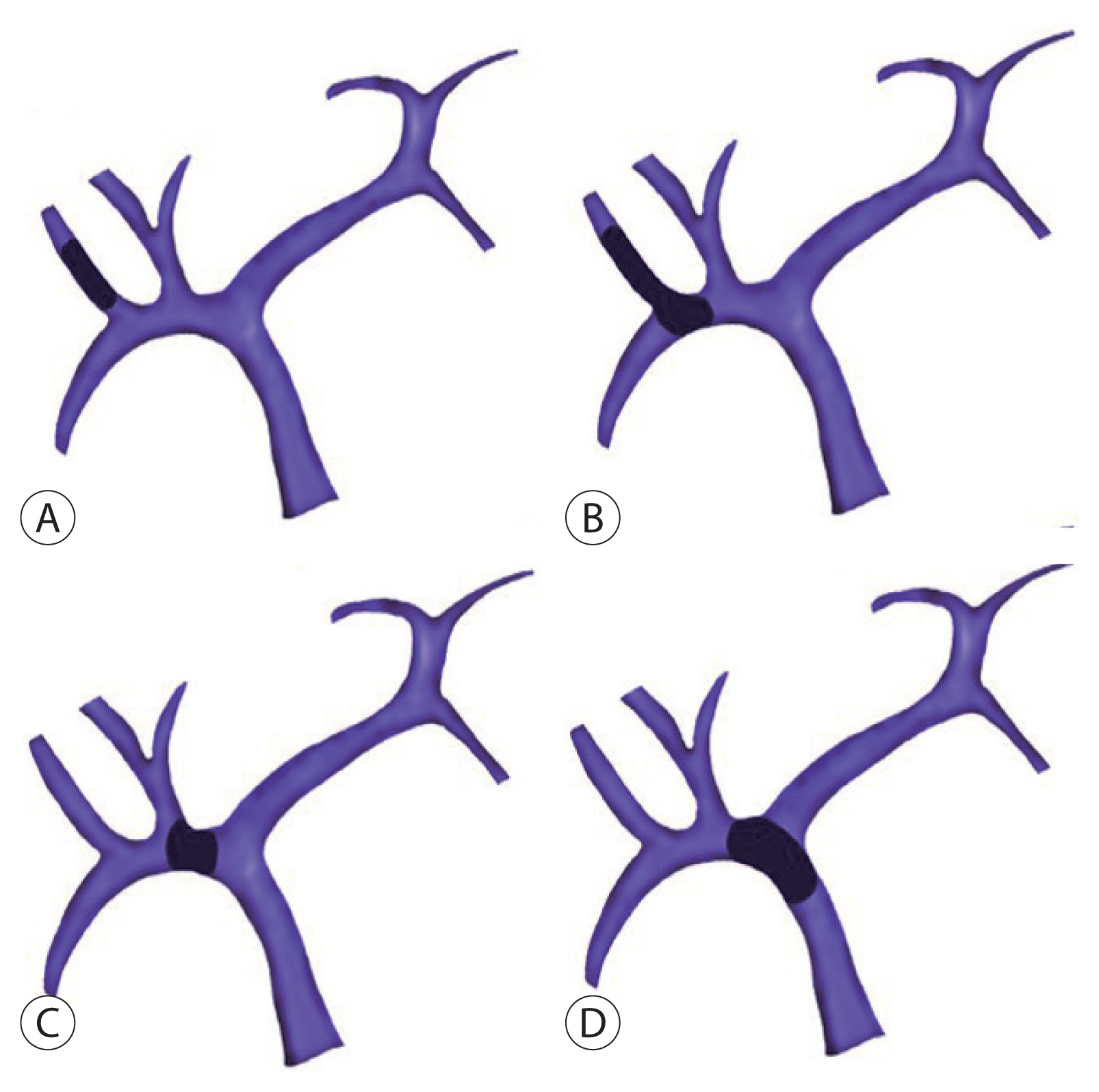
PDF - Traditionally, liver transplantation for hepatocellular carcinoma with portal vein tumor thrombosis is not recommended. However, with recent developments in locoregional therapies for hepatocellular carcinoma, more aggressive treatments have been attempted for advanced hepatocellular carcinoma. Recently, various studies on locoregional therapies for downstaging followed by living donor liver transplantation reported inspiring overall survival and recurrence-free survival of patients. These downstaging procedures included three-dimensional conformal radiation therapy, trans-arterial chemoembolization, stereotactic body radiation therapy, trans-arterial radioembolization, hepatic arterial infusion chemotherapy and combinations of these therapies. Selection of the optimal downstaging protocol should depend on tumor location, biology and background liver status. The risk factors affecting outcome include pre-downstaging alpha-fetoprotein values, delta alpha-fetoprotein values, disappearance of portal vein tumor thrombosis on imaging and meeting the Milan criteria or not after downstaging. For hepatocellular carcinoma with portal vein tumor thrombosis, downstaging procedure with liver transplantation in mind would be helpful. If the reaction of the downstaged tumor is good, liver transplantation may be performed.
-
Citations
Citations to this article as recorded by- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy
Hun Kim, Tae Hoon Roh, Jun Seop Lee, Min Seong Kim, Beom Kyung Kim
Journal of Liver Cancer.2024; 24(1): 113. CrossRef - Refining MRI-based criteria for portal vein invasion in hepatocellular carcinoma: improving sensitivity beyond portal vein tumor thrombosis
Jeongju Kim, Woo Kyoung Jeong, Jong Man Kim, Sang Yun Ha, Kyunga Kim
Abdominal Radiology.2023; 49(2): 437. CrossRef - Prediction models of hepatocellular carcinoma recurrence after liver transplantation: A comprehensive review
Sang Jin Kim, Jong Man Kim
Clinical and Molecular Hepatology.2022; 28(4): 739. CrossRef
- Metastatic papillary renal cell carcinoma with portal vein tumor thrombosis confirmed on blind liver biopsy

Case Report
- Successful Sequential Therapy Involving Regorafenib after Failure of Sorafenib in a Patient with Recurrent Hepatocellular Carcinoma after Liver Transplantation
- Soon Kyu Lee, Jeong Won Jang, Heechul Nam, Pil Soo Sung, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon
- J Liver Cancer. 2020;20(1):84-89. Published online March 31, 2020
- DOI: https://doi.org/10.17998/jlc.20.1.84
- 3,333 Views
- 89 Downloads
-
 Abstract
Abstract
 PDF
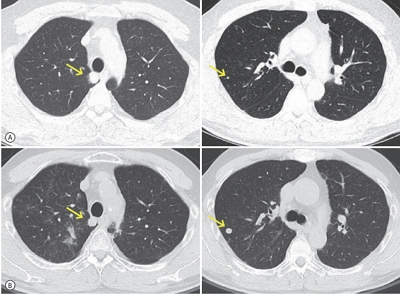
PDF - The efficacy and safety of sequential systemic therapy for the treatment of recurrent hepatocellular carcinoma (HCC) after liver transplantation (LT) are not well established. This study describes a successful experience where sequential therapy with sorafenib followed by regorafenib was used to treat recurrent HCC in a 54-year old male LT recipient. After HCC recurred in both lungs 10 months after LT, sorafenib was administered with radiation therapy to treat pulmonary metastases. However, after 4 months of sorafenib treatment showed progressive pulmonary metastases, sequential regorafenib treatment was started. After 3 months (cycles) of regorafenib treatment, tumor response was partial, and after 6 months (cycles), disease status remained stable without signs of progression or drug-related serious adverse events. This case suggests that sequential systemic therapy is feasible in patient with recurrent HCC after LT.

Review Article
- Liver Transplantation in Mixed Hepatocellular Carcinoma and Cholangiocarcinoma
- Jong Man Kim
- J Liver Cancer. 2019;19(2):85-90. Published online September 30, 2019
- DOI: https://doi.org/10.17998/jlc.19.2.85
- 3,832 Views
- 89 Downloads
- 2 Citations
-
 Abstract
Abstract
 PDF
PDF - Mixed hepatocellular carcinoma and cholangiocarcinoma (HCC-CC) are rare tumors, and the risk factors associated with them are not well understood yet. Moreover, the diagnosis of mixed HCC-CC can be complicated due to the difficulty in distinguishing mixed HCC-CC from HCC and intrahepatic CCC on radiological images. Serum tumor markers are useful when the radiological images are inconclusive. It remains unclear whether the prognosis of mixed HCC-CC differs from that of HCC. However, several studies have reported that the tumor recurrence and patient survival rates of mixed HCC-CC were similar to those of HCC after liver transplantation (LT) and liver resection. In this paper, we report that LT in patients with mixed HCC-CC achieves outcomes which are similar to those seen in LT for HCC. Therefore, the diagnosis of mixed HCC-CC should not be considered as a contraindication for LT.
-
Citations
Citations to this article as recorded by- Liver transplantation for combined hepatocellular carcinoma and cholangiocarcinoma: A multicenter study
Jongman Kim, Dong-Jin Joo, Shin Hwang, Jeong-Moo Lee, Je-Ho Ryu, Yang-Won Nah, Dong-Sik Kim, Doo-Jin Kim, Young-Kyoung You, Hee-Chul Yu
World Journal of Gastrointestinal Surgery.2023; 15(7): 1340. CrossRef - The Role of Immunosuppression for Recurrent Cholangiocellular Carcinoma after Liver Transplantation
Safak Gül-Klein, Paulina Schmitz, Wenzel Schöning, Robert Öllinger, Georg Lurje, Sven Jonas, Deniz Uluk, Uwe Pelzer, Frank Tacke, Moritz Schmelzle, Johann Pratschke, Ramin Raul Ossami Saidy, Dennis Eurich
Cancers.2022; 14(12): 2890. CrossRef
- Liver transplantation for combined hepatocellular carcinoma and cholangiocarcinoma: A multicenter study

Case Report
- A Case of Successful Living Donor Liver Transplantation after Downstaging of Hepatocellular Carcinoma with the Beyond Milan Criteria by Radioembolization, Hepatic Arterial Infusion Chemotherapy, and Stereotactic Body Radiation Therapy
- Yeong Jin Kim, Yeon Seung Chung, Beom Kyung Kim, Jin Sil Sung, Do Young Kim
- J Liver Cancer. 2017;17(2):182-185. Published online September 30, 2017
- DOI: https://doi.org/10.17998/jlc.17.2.182
- 1,901 Views
- 16 Downloads
-
 Abstract
Abstract
 PDF
PDF - Liver transplantation for patients with hepatocellular carcinoma (HCC) within the Milan criteria
generally yields a 4-year overall survival rate of 75% and 4-year recurrence free survival rate of 83%.
But, many HCC patients present with the disease beyond the Milan criteria. On the other hands, the
overall survival of patients with advanced HCC with portal vein invasion is very poor. We report a
case
of successful living donor liver transplantation for advanced HCC with portal vein invasion by down-staging through radioembolization, hepatic arterial infusion chemotherapy, and stereotactic body radiation therapy.

Review Article
- Surgical Perspectives of Hepatocellular Carcinoma beyond the Barcelona Clinical Liver Cancer Guideline; Focusing on Liver Transplantation
- Nam-Joon Yi, Gwang-Woong Lee, Kyoung-Suk Suh
- J Liver Cancer. 2015;15(1):4-10. Published online March 31, 2015
- DOI: https://doi.org/10.17998/jlc.15.1.4
- 871 Views
- 13 Downloads
-
 Abstract
Abstract
 PDF
PDF - The management of hepatocellular carcinoma (HCC) is decided according to the evidence base recommendations generated by international societies especially by Barcelona clinical liver cancer (BCLC) guideline. However, the BCLC guideline based on studies of the Western countries, has not been well matched to real life cohort in Korea. In Western countries, a deceased donor liver transplantation has been well allocated to the HCC patients with preserved liver function. Patients with mild to moderate portal hypertension and certain BCLC B patients could be eligible for hepatic resection if a chance for 50% survival rate at 5 years is perceived. If liver transplantation (LT) is back up for liver resection in those patients as a salvage therapy, widening indication of liver resection could be much easily acceptable. On the other hands, new selection criteria of HCC beyond Milan criteria considering tumor biology, has been provided in the field of LT resulting in more than 50% survival rate at 5 years. Herein, surgical perspectives beyond the BCLC recommendation for LT for HCC would be reviewed in the respect of Korean surgeon’s view in this article.

Case Report
- Living Donor Liver Transplantation for Hepatocellular Carcinoma with Portal Vein Tumor Thrombus
- YoungRok Choi, Kwang-Woong Lee, Hae Won Lee, Nam-Joon Yi, Kyung-Suk Suh
- Journal of the Korean Liver Cancer Study Group. 2013;13(1):62-64. Published online February 28, 2013
- DOI: https://doi.org/10.17998/jlc.13.1.62
- 1,200 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Malignant portal vein thrombosis is a contraindication to liver transplantation for hepatocellular carcinoma because of the high risk of its recurrence and the poor patient survival. With a newly developed immunosuppressant and a chemotherapeutic agent, however, living donor liver transplantation can be considered for a patient of hepatocellular carcinoma, showing a slow growth rate and good response for transarterial chemoembolization. We report a HBV related liver cirrhosis patient with HCC and portal vein tumor thrombus who underwent living donor liver transplantation and survived without recurrence of hepatocellular carcinoma for 18 months in our center.

Review Articles
- Strategies for the Curative Therapy of Early Stage HCC: First or SalvageTransplantation?
- Nam-Joon Yi
- Journal of the Korean Liver Cancer Study Group. 2012;12(2):102-108. Published online September 30, 2012
- 519 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) is a major cause of cancer mortality worldwide, especially in Asian countriesas well as Korea, and liver transplantation (LT) has potentials to improve survival for patients with HCC. However, major hamper to LT for HCC has been graft shortage. To solve this problem, liver resection (LR) has to be rejuvenated in the general algorithm of HCC treatment in the light of salvage transplantation (ST) strategies. The LR followed by ST in case of HCC recurrence is an attractive concept in early stage HCC and cirrhosis with acceptable liver function. These challenges in technique, indications, pre-LT observation and treatments for recurred HCC, and prioritization policies of patients on the waiting list have to be precise through prospective investigations that have to include individualization of prognosis, biological variables and pathology surrogates as stratification criteria. Accepting this challenges have been part of the history of LT and will endure for the future. This article will focus on the ST after LR in terms of intention-to-analysis

- Gobal Discrepancy of Practical Guidelines for Management of Hepatocellular Carcinoma-Resection and Transplanation
- Kwang-Woong Lee
- Journal of the Korean Liver Cancer Study Group. 2011;11(1):18-22. Published online February 28, 2011
- 482 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - Hepatocellular carcinoma (HCC) usually appears in the setting of underlying liver disease. Therefore, HCC should be managed in multidisciplinary settings. Under these circumstances, several practice guidelines were introduced around the world. Clinically useful practice guidelines should be based on evidences, but socio-economic and medical status of the country should be considered as well. In this review, 6 well-known global practical guidelines (BCLC-AASLD, NCCN, 2 from Japan, APASL, Korean) were compared in terms of resection and liver transplantation (LT). BCLC-AASLD from Europe and the United States stressed more on LT for the patients within Milan criteria. However, the guidelines from the Asia had more extended indication of liver resection. The number of living donor LT in Korea is the highest in the world. Under this circumstance, indication of LT for HCC in Korea is inevitably being expanded. Compared to other guidelines, therefore, Korean guideline allowed a limited expansion of indication for HCC into patients with Child A and/or living donor LT with outside Milan HCC. However, to make more practical guidelines, high quality evidence from Korea and validation study of current Korean guideline are needed.

Case Report
- A Case of Multiple Hepatocellular Carcinoma which was Performed Liver Transplantation after Down-staging by Transcatheter Arterial Chemoembolization
- Hee-Jung Wang, Bong-Wan Kim, Sung-Won Cho, Je-Hwan Won
- Journal of the Korean Liver Cancer Study Group. 2011;11(1):50-55. Published online February 28, 2011
- 515 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - A case of multiple hepatocellular carcinoma (HCC) which was performed a living donor liver transplantation (LDLT) after down-staging by transcatheter arterial chemoembolization (TACE) is reviewed. Generally, the recommended therapeutic strategy for this kind of HCC is TACE. However, the response of multiple HCC of this 48 year-old male patient was relatively good after 4 times of TACE, and we performed LDLT on the concept of clinical trial under the informed consent of patient and his families. Although there were two times recurrences in the liver and lung, he has overcome them and is still alive 66 months after LDLT. We suggest that liver transplantation could be an alternative strategy in the multiple HCC cases who show good responses after TACE.

Review Article
- 2009 Treatment Guideline for Hepatocellular Carcinoma: Surgical Resection and Liver Transplantation
- Sung Hoon Kim, Kyung Sik Kim
- Journal of the Korean Liver Cancer Study Group. 2010;10(1):6-10. Published online June 30, 2010
- 481 Views
- 4 Downloads
-
 Abstract
Abstract
 PDF
PDF - The effort we are trying to set up the treatment guideline for hepatocellular carcinoma has produced various guidelines after drawing a conclusion from Barcelona EASL meeting in 2000. Especially in Korea, the Korean Liver Cancer Study Group and the National Cancer Center have collaborated on making treatment guideline for hepatocellular carcinoma in the early stage of setting up the guideline, 2003, and it was a great help to treatment, study and education. However, a need of revision had been raised due to many changes in the latest treatments and an accumulation of international and domestic experience. After the proposal of amending the treatment guideline for Hepatocellular carcinoma in the Cancer Control Forum of the National Cancer Control Planning Board on October 17th, 2008, “2009 Guideline” has been reported in the Conference of the Korean Liver Cancer Study Group held on June 27th, 2009. When revising the guideline, there are some suggestions of continuous modification to reflect evidence based medical knowledge, and recently there are some debates about the drawback of the surgical field which was not handled in EASL and AASLD Guidelines. Therefore, it will broaden your understanding of liver surgical resection and liver transplantation and it will also be a place for the discussion of disputable issues.

Case Report
- Rapid recurrence following living donor liver transplantation for hepatocellular carcinoma within Milan criteria
- Hyun Young Woo, Jin Dong Kim, Jung Hyun Kwon, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon, Sung Eun Rha, Jae Young Byun, Ho Jong Chun, Byung Gil Choi, Hae Kyu Lee, Young Kyoung You, Dong Gu Kim
- Journal of the Korean Liver Cancer Study Group. 2009;9(1):45-48. Published online June 30, 2009
- 535 Views
- 5 Downloads
-
 Abstract
Abstract
 PDF
PDF - Liver transplantation is curative therapy for hepatocellular carcinoma especially if ,within Milan criteria, 4 year survival and recurrence-free survival was reported to be 85% and 92%, respectively. Herein we report a patient who experience rapid recurrence following living donor liver transplantation (LDLT) for hepatocellular carcinoma within Milan criteria. A 52 year-old-men patient with known liver cirrhosis associated with hepatitis B virus was admitted for the treatment of hepatocellular carcinoma (HCC). Abdominal CT revealed two nodules less than 3 cm in right hepatic lobe. After single session of transcatheter arterial chemoembolization (TACE), the patient underwent LDLT. After seven months following transplantation, recurrent HCC was detected on transplanted liver with concurrent metastatic nodule in lung. Although TACE and metastsectomy were performed for recurrent intrahepatic mass and lung metastasis, recurrent HCC showed rapid progression and patient died of progressive tumor after 10 months following LDLT.

Review Article
- Hepatocellular carcinoma and Liver transplantation
- Myoung Soo Kim
- Journal of the Korean Liver Cancer Study Group. 2007;7(1):35-40. Published online June 30, 2007
- 562 Views
- 3 Downloads
-
 Abstract
Abstract
 PDF
PDF - Liver transplantation is the prime management for early hepatocellular carcinoma with liver cirrhosis that is not candidate for surgical resection. Milan criteria, single tumor less than 5 cm or less than three tumors with less than 3 cm, is accepted as an indication for liver transplantation. The extended criteria do not show reliable result in long-term recurrent-free survival rate. Shortage of donor and following high drop-out rate during waiting time are main obstacle to liver transplantation, which can be alleviated by the living donor liver transplantation and priority policies in deceased donor liver allocation. The pre-operative loco-regional therapy, such as transarterial chemoembolization (TACE), radiofrequency ablation (RFA) and regional surgical resection, decreases the drop-out rate for waiting time and supplies time for preparing the liver transplantation. Generally acceptable recurrence rate after liver transplantation is less than 15%. The size of mass, vascular or lymphatic-invasion, low grade tumor and high pre-operative level of alpha-Fetoprotein (AFP) are risk factors for recurrence. The prognosis of recurred hepatocellular carcinoma is fatal. Neoadjuvant chemotherapy after liver transplantation cannot prolong the patient survival rate and decrease the recurrence rate. Above 50% of recurrence-free patient survival rate at post-transplant 5 years is reliable result after liver transplantation in hepatocellular carcinoma. The survival rate is improved after mid-1990, and is reported as 60-70% at post-transplant 5 years. The living donor liver transplantation shows more superior survival rate than deceased donor liver transplantation.

Case Report
- A Case of Hepatocellular Carcinoma Araising from Dysplastic Nodule
- Sang Hoon Ahn, Yong Nyun Park, Yoon Jae Kim, Jae Yoon Chon, Young Myoung Moon, Kwang Hyub Han
- Journal of the Korean Liver Cancer Study Group. 2003;3(1):83-86. Published online July 31, 2003
- 500 Views
- 1 Download
-
 Abstract
Abstract
 PDF
PDF - Early diagnosis is invaluable for the treatment of hepatocellular carcinoma (HCC). However, it does not seem to be easy to differentiate between HCC arising in dysplastic nodule and dysplastic nodule without HCC foci by radiologic findings. We report a case of HCC arising in dysplastic nodule, which is confirmed by pathological examination of explanted liver.


 E-submission
E-submission THE KOREAN LIVER CANCER ASSOCIATION
THE KOREAN LIVER CANCER ASSOCIATION

 First
First Prev
Prev



 Follow JLC on Twitter
Follow JLC on Twitter